Translate this page into:
Traumatic lumbar spondylolisthesis: A case report and review of literature
*Corresponding author: François de Paule Dognon Kossi Adjiou, Department of Neurosurgery, Hôpital des Spécialités, Mohammed V University in Rabat, Morocco. adjiou24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adjiou FD, Hakkou E, Abbas S, El Manouni O, Kajeou M, El Ouahabi A. Traumatic lumbar spondylolisthesis: A case report and review of literature. J Neurosci Rural Pract. 2024;15:377-80. doi: 10.25259/JNRP_330_2023
Abstract
Traumatic spondylolisthesis of the lumbosacral junction (SPL) is a spinal injury rarely seen in current practice. Few cases are reported in the literature. It arises from complex trauma of high-energy mechanisms. We discussed the case of a young patient. He is 24 years old without notable pathological history victim of a traffic road accident. Clinically, he has no sensory or motor deficit, it is a spinal trauma classified American spinal injury association E (ASIA E) with severe back pain. A whole-body CT scan performed on admission showed a grade 2 L5–S1 SPL. A lumbar MRI revealed a tear of the disc at L5–S1. We performed a laminectomy to decompress the dural sheath and cauda equina roots with transforaminal lumbar interbody fusion. A postoperative CT scan showed the reduction of the spondylolisthesis. Two months later, the patient resumed walking. Surgery is the gold standard for the management of traumatic SPL. The aim of surgery is to achieve neural structure decompression and obtain stability with fusion.
Keywords
Traumatic spondylolisthesis
Physiopathology
Management
Case report
INTRODUCTION
Spondylolisthesis (SPL) has several causes. According to Wiltse et al.,[1] there are many types of SPL: Dysplastic, isthmic, degenerative, pathological, and traumatic. The SPL due to trauma is a spinal injury rarely seen in current practice that arises from complex trauma of high-energy mechanisms. This leads to important changes in intervertebral articulations.[2] Because this injury leads to the destruction of spinal stability elements, particularly bone and discoligamentous elements, there is a substantial risk of neurological deficiency, and it is extremely unstable. Restoring stability and preventing secondary spinal cord and root compression are the goals of treatment. We discussed a case of L5–S1 SPL caused by a violent lumbar impact treated by decompression and transforaminal lumbar interbody fusion (TLIF) with a successful outcome.
CASE REPORT
We present the clinical case of a young patient aged 24, in excellent physical shape, victim of a traffic road accident, and presenting a lumbar spine trauma American spinal injury association E (ASIA E). He was a passenger, who jumped from a moving vehicle after it was about to collide with another vehicle. On the physical examination, he had severe back pain preventing him from being in a strict supine position. He had no sensory-motor deficits, and the examination of the urogenital sphere did not reveal any bladder globe or other genital-sphincter disorders. A whole-body CT scan was performed on admission. At the spinal level, we noticed a fracture of the posteroinferior corner of L5 and an intracanal displacement of the fractured fragment, a fracture of the superior articular process of S1 and L5–S1 spondylolisthesis [Figure 1a]. A lumbar spine CT scan performed later to better study the lesion objectified a reduction of the spondyloptosis [Figure 1b].
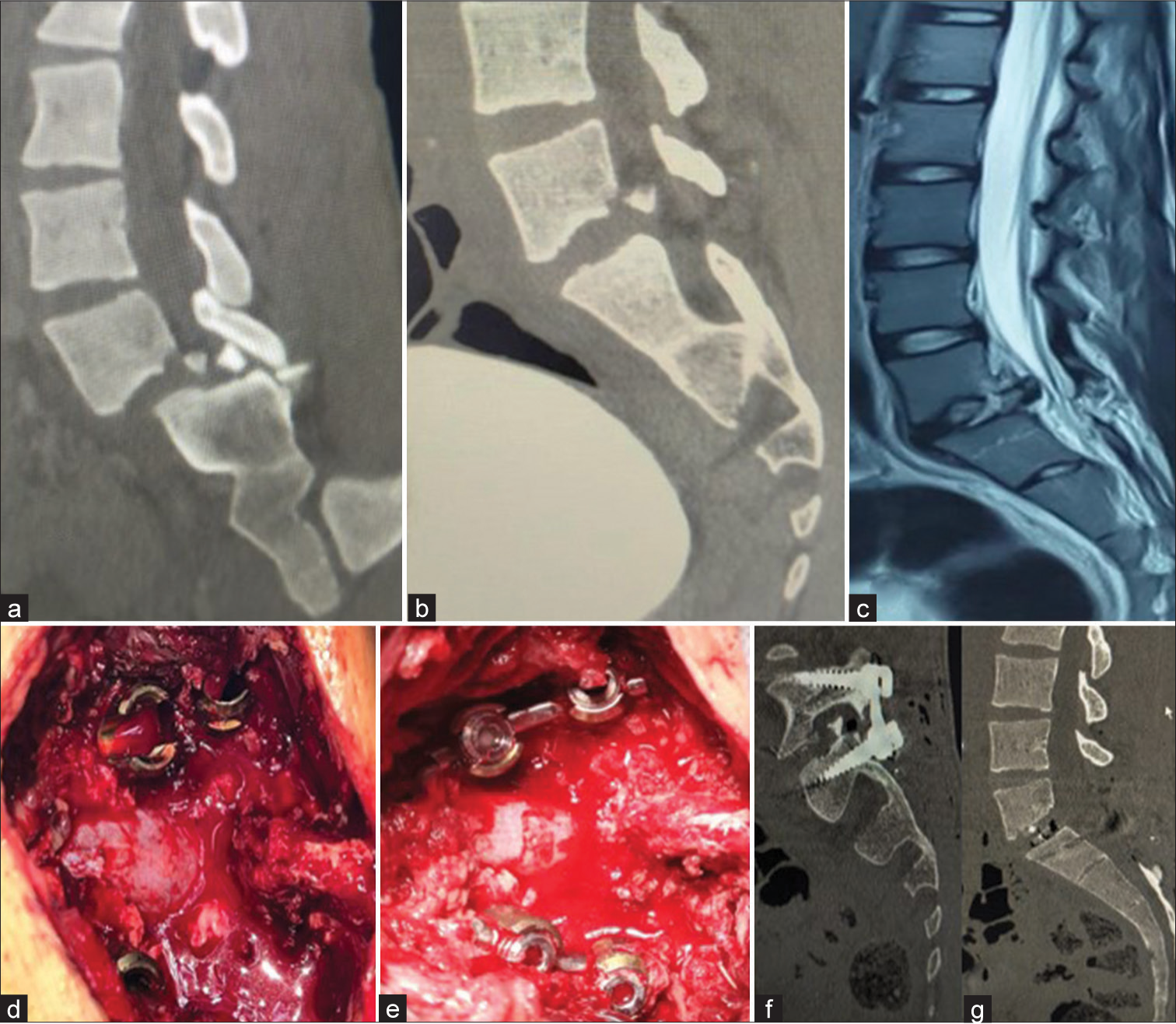
- (a) Spine computed tomography (CT) scan showing a fracture of the posteroinferior corner of the vertebral body of L5 with intracanal displacement of the fractured fragment-spondylolisthesis (SPL) grade II L5–S1 and (b) CT scan showing a spontaneous reduction of the SPL. (c) Magnetic resonance imaging: lesion of the L5–S1 disc and (d and e) Intraoperative image before reduction showing a step between the level of the screws at L5 and S1. After placement of the rods, we can see a reduction of the dislocation. (f and g) Pedicle screw fixation of L5–S1 with transforaminal lumbar interbody fusion.
An MRI revealed a lesion of the L5–S1 disc with disruption of the yellow ligament and the posterior common longitudinal ligament [Figure 1c]. The patient underwent open surgery with pedicle screw fixation of L5–S1, decompression of the dural sheath by laminectomy of L5 and S1, bilateral arthrotomy of L5–S1, discectomy of L5–S1, and placement of a cage filled with autograft by TLIF. Intraoperative fluoroscopy before the incision showed an anterior displacement of L5 on S1. At incision and after the release of paravertebral gutters, we noticed a fracture of the spinous process of L5, the paravertebral muscles were contused, and an abundant leakage of cerebrospinal fluid was seen. We performed an extended L5 laminectomy at the level of the canal sacred in front of S1. Ligament injuries (interspinous ligaments and ligamentum flavum) were confirmed. We discovered a breach of the dura mater, which was sutured. The screws were placed followed by a discectomy of L5–S1 with the placement of a cage. We also confirmed the disruption of the L5–S1 intervertebral disc. The gesture was then followed by the placement of the rods. The challenge was the reduction of the dislocation intraoperatively due to the lack of retaining screws. [Figures 1d and e] are intraoperative view before and after reduction. After the placement of the rods, the intraoperative check-up showed a reduction of the dislocation. Postoperatively, the patient did not present sensory-motor deficits or genitosphincterian disorders. Figure 1f and g showed the post-operative CT scan. Two months later, the patient resumed walking.
DISCUSSION
We report a unique case of traumatic lumbar spine SPL managed surgically with a good outcome. Traumatic SPLs are very unstable. They lead to lesions of the discoligamentous elements of the posterior column of the spine. Osteosynthesis with disc replacement remains the best therapeutic approach. According to biomechanical research, a facet dislocation requires the interaction of a rotation force and a hyperflexion mechanism that applies shearing stresses to the sacral bone.[3-5] Spinal stability would be severely compromised in the absence of the osteoligamentous elements and the pars interarticularis. Traumatic lumbar SPL is an injury of the elements of stability of the spine associated with vertebral body listhesis.[6] Our patient is a young adult victim of a high-kinetic accident with very severe lumbar pain preventing him from lying on his back. A significant decrease in pain intensity is observed postoperatively. Xu et al. reported an L3–L4 spondylisthesis case. The patient was 42 years old, a victim of a work accident due to a fall. He had severe back pain and had no neurological damage.[7] Barwar reported the case of traumatic L4–L5 SPL with cauda equina syndrome treated surgically. When the patient was seen in the follow-up, he was recovered from the deficit.[8] Signs vary from asymptomatic patients with lower back pain to patients with neurological deficits up to cauda equina syndrome.
The radiological and intraoperative lesion assessment showed in our case a fracture of the spinous and laminae of L5, a contusion at the level of the yellow ligament and a tear of the disc. Note also that the spondylolisthesis was reduced spontaneously. This testifies to the instability of the lesion. The high kinetic mechanism is responsible of lesions of the posterior ligamentous structures; the facets and the vertebrae body fractures, and anterior sliding of the L5 vertebrae body. This leads to instability at the level of the three columns of Denis. The instability criteria are, apart from root compression, the strongest argument to indicate osteosynthesis.
Osteosynthesis combined with posterior intervertebral fusion is the most used technique described in the literature. Some cases of traumatic SPL in literature are summarized in Table 1.[6-15] The optimal therapeutic strategy depends on the expertise of each surgical team but also on the different bone and discoligamentous lesions presented by the patient. The technical platform and the osteosynthesis implants available are also taken into consideration. Our patient has benefited from a TLIF. Due to technical innovations and improvements in implants, combined approaches are more and more implemented.
| Authors | Liu and Menga 2021 | Xu et al. 2020 | Park et al. 2020 | Papaioannou et al. 2021 | Fok and Cheung 2019 | Ver et al. 2019 | Barwar 2021 | Koruga et al. 2020 | Sasagawa 2022 | Hu et al. 2022 |
|---|---|---|---|---|---|---|---|---|---|---|
| Study design | Case report | Case report and literature review | Case report | Case report | Case report | Systematic review and case series 125 cases | Case report | Case report | Case report | Case series 28 cases |
| Age (Years) | 24 | 42 | 65 | 53 | 40 | 30.5 | 24 | 48 | 60 | NR |
| Level | L3–4 | L3–4 | L5–S1 | L4–5 | L4–5 | NR | L4–5 | L1–2 | L4–L5 | NR |
| Neurological statut | Radiculopathy | Back pain+spinal deformity | Cauda equina syndrome | Normal | Cauda equina syndrome | Back pain+ neurologic deficits |
ASIA A | ASIA D | Frankel D | NR |
| Management | DR+PSF+ interbody fusion through a lateral approach |
DR+PSF+ interbody fusion |
Posterior DR+PSF+and anterior reconstruction | DR+PSF | DR+ instrumented fusion |
DR+PSF+ interbody fusion |
DR+PSF+ TLIF |
PSF via posterior approach | Minimally invasive surgery anteroposterior surgery and OLIF | PSF+PLIF |
NR: Not reported, OLIF: Oblique lumbar interbody fusion, PLIF: Posterior lumbar interbody fusion, PSF: Pedicle screw fixation, DR: Decompression and reduction, TLIF: Transforaminal lumbar interbody fusion, ASIA: American spinal injury association
CONCLUSION
Post-traumatic SPL is rare; it is caused by high kinetic mechanisms associating with hyperflexion, rotation, and distraction. It is associated with discoligamentous lesions making it unstable. Surgery is the gold standard for its management. The aim of surgery is to decompress and stabilize with subsequent fusion.
Acknowledgments
We would like to give special thanks to Dr. Yao Christian Hugues Dokponou, Dr. Fresnel Lutèce Ontsi Obame, Dr. Bankole Adeniran Nourou Dine for their opinions, corrections, and contributions while writing this manuscript.
Authors’ contributions
Dognon Kossi François de Paule Adjiou: Conceptualization, Writing original draft-editing. Salma Abbas: Review and editing. El Manouni Othmane: Review and editing. Meriem Kajeou: Review and editing. Hakkou El Mehdi: Supervision, Validation. Abdessamad El Ouahabi: Supervision, Validation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res. 1976;117:23-9.
- [CrossRef] [Google Scholar]
- Traumatic lumbar spondylolisthesis In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2022.
- [Google Scholar]
- Traumatic anterior lumbosacral dislocation caused by hyperextension mechanism in preexisting L5 spondylolysis: A case report and a review of literature. J Spinal Disord Tech. 2006;19:455-62.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic posterior fracture-dislocation of the fifth lumbar vertebra: Report of two cases with review of literature. Spinal Cord Ser Cases. 2021;7:30.
- [CrossRef] [PubMed] [Google Scholar]
- A study of the mechanics of spinal injuries. J Bone Joint Surg. 1960;42-B:810-23.
- [CrossRef] [Google Scholar]
- Traumatic lumbar spondylolisthesis: A systematic review and case series. Global Spine J. 2019;9:767-82.
- [CrossRef] [PubMed] [Google Scholar]
- Mid-lumbar traumatic spondyloptosis without neurological deficit: A case report and literature review. Medicine (Baltimore). 2020;99:e19578.
- [CrossRef] [PubMed] [Google Scholar]
- Post-traumatic L4-L5 spondyloptosis with cauda equina syndrome: A case report. Trauma Case Rep. 2021;33:100475.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic bilateral L3-4 facet dislocation with open decompression and short segment fusion. Int J Spine Surg. 2021;14:S21-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture-dislocation of L5 combined with multi-level traumatic spondylolisthesis of the lower lumbar spine treated via the posterior-only approach: A case report. Korean J Neurotrauma. 2020;16:313-9.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic spondylolisthesis of the fourth lumbar vertebra without neurologic deficit or fracture of the posterior elements. Cureus. 2021;13:e13238.
- [CrossRef] [Google Scholar]
- Traumatic bilateral L4-5 facet fracture dislocation: A case presentation with mechanism of injury. BMC Musculoskelet Disord. 2019;20:558.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar spondyloptosis after severe polytrauma: A case report. Acta Clin Croat. 2020;59:555-9.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive surgery for traumatic spondylolisthesis of L4: A case report. J Orthop Sci. 2022;27:292-5.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristic and surgical treatment of traumatic lumbar spondylolisthesis: A series of 28 patients. Injury. 2022;53:1094-7.
- [CrossRef] [PubMed] [Google Scholar]






