Translate this page into:
To Compare Diagnostic Ability of Contrast-Enhanced Three-Dimensional T1-SPACE with Three-Dimensional Fluid-Attenuated Inversion Recovery and Three-Dimensional T1-Magnetization Prepared Rapid Gradient Echo Magnetic Resonance Sequences in Patients of Meningitis
Address for correspondence: Dr. Suresh Kumar, Department of Radiodiagnosis and Imaging, IGMC, Shimla - 171 001, Himachal Pradesh, India. E-mail: thakursuresh67@yahoo.co.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
The aim of this study is to compare postcontrast three-dimensional (3D) T1-Sampling perfection with application-optimized contrasts by using different flip angle evolutions, 3D fluid-attenuated inversion recovery (FLAIR), and 3D T1-magnetization prepared rapid gradient echo (MPRAGE) sequences in patients of meningitis.
Settings and Design:
A hospital-based cross-sectional study done in the Department of Radiodiagnosis, IGMC Shimla for a period of 1 year from June 1, 2016, to May 30, 2017.
Subjects and Methods:
A total of 30 patients suspected of meningitis underwent magnetic resonance imaging evaluation with postcontrast 3D T1-MPRAGE, 3D T1-SPACE, and 3D FLAIR sequences. The abnormal leptomeningeal enhancement was noted by two radiologists together on these sequences and scores were given to the abnormal leptomeningeal enhancement.
Statistical Analysis Used:
The sensitivity of 3D T1-SPACE, 3D T1-MPRAGE, and 3D FLAIR was calculated and compared. The level of agreement between these sequences was assessed by kappa coefficient. P < 0.05 was taken as statistically significant.
Results:
3D T1-SPACE shows superiority in meningeal enhancement along basal cisterns, Sylvian fissure and along cerebral convexities. It is also found to be better in delineating parenchymal lesions. 3D FLAIR failed to demonstrate enhancement along cerebral convexities however found to be better than 3D T1-MPRAGE in delineating enhancement along basal cisterns and Sylvian fissures. 3D T1-MPRAGE has shown subtle enhancement in basal cisterns, Sylvian fissure and along cerebral convexities. 3D T1-SPACE, 3D FLAIR, and 3D T1-MPRAGE has sensitivity of 91.67%, 66.67%, and 54.17%, respectively.
Conclusion:
Postcontrast 3D T1-SPACE sequence is an excellent tool than postcontrast 3D T1-MPRAGE and 3D FLAIR sequences in the evaluation of meningeal enhancement and depiction of additional lesions in brain parenchyma.
Keywords
Fluid-attenuated inversion recovery
meningitis
T1-magnetization prepared rapid gradient echo
T1-Sampling perfection with application-optimized contrasts by using different flip angle evolutions
INTRODUCTION
The contrast-enhanced magnetic resonance imaging (MRI) is superior in demonstrating leptomeningeal enhancement as the disease process may be detected at an early stage.[1] It is superior because it is free of bony artifacts and has greater inherent soft-tissue contrast resolution. The normal pattern of dural enhancement is thin, linear, and discontinuous.[2] Leptomeningeal enhancement follows into sulci whereas pachymeningeal enhancement appears along inner surface of skull. The normal meningeal enhancement is of short segment (<3 cm) and is likely due to enhancement of meningeal vessels.[3] The enhancement pattern in bacterial and viral meningitis is thin and linear. Fungal and neoplastic meningitis exhibits thick and nodular leptomeningeal enhancement.[4] Postcontrast fluid-attenuated inversion recovery (PCFLAIR) has less incidence of cerebrospinal fluid (CSF) motion artifacts.[5] 3D-magnetization prepared rapid gradient echo (MPRAGE) sequence has a better contrast between gray and white matter than with spin echo sequence. T1-W 3D SPACE sequence has a better depiction of meningeal diseases because of better suppression of blood flow signal from vessels on the brain surface.[6]
SUBJECTS AND METHODS
The patients who met inclusion criteria are patients with clinical features suggestive of meningitis and age more than 10 years irrespective of gender. The patients excluded were patients with cochlear implants, cardiac pacemakers, aneurysmal clips, and claustrophobic patients.
Magnetic resonance imaging acquisition
Magnetic resonance (MR) images were obtained on 1.5T Magnetom Avanto system (Siemens, Erlangen, Germany) using 18-channel head coil.
The MRI protocol included precontrast T1-W, T2-W, FLAIR, diffusion-weighted imaging, susceptibility-weighted imaging sequences and postcontrast 3D T1-SPACE, 3D T1-MPRAGE and 3D FLAIR sequences.
MR imaging sequences obtained after contrast administration:
-
3D T1-MPRAGE (repetition time [TR] = 1900 ms, echo time [TE] = 3.25 ms, slice thickness = 1.0 mm, number of averages = 1, field of view [FOV] = 256 mm2, bandwidth = 150 hz, matrix size = 208 × 256, time of acquisition = 3:40 min)
-
3D T1-SPACE (TR = 600 ms, TE = 8 ms, slice thickness = 1.0 mm, number of averages = 1, FOV = 256 mm2, bandwidth = 630 hz, matrix size = 256 × 256, time of acquisition = 5:34 min)
-
3D FLAIR (TR = 5000 ms, TE = 331 ms, slice thickness = 1.0 mm, number of averages = 1, FOV = 256 mm2, bandwidth = 592 hz, matrix size = 224 × 254, time of acquisition = 5:15 min).
Other tests include blood glucose, serum urea, and creatinine estimation, CSF analysis, Mycobacterium tuberculosis complex (MTBC) and adenosine deaminase (ADA).
Two radiologists together viewed the imaging and evaluated leptomeningeal enhancement in basal cisterns, Sylvian fissure and along cerebral convexities on post contrast 3D T1-MPRAGE, 3D T1-SPACE, and 3D FLAIR images. The scoring system was adopted to give scores to the leptomeningeal enhancement according to 4-point scoring system where 3 = definite abnormal leptomeningeal enhancement which is clearly differentiable from meningeal vessel, 2 = probable abnormal leptomeningeal enhancement which appears to be different from meningeal vessel, 1 = possible abnormal leptomeningeal enhancement which is not differentiable from meningeal vessel, 0 = no abnormal leptomeningeal enhancement. The scores were given, and the results were compared for 3D T1-MPRAGE, 3D T1-SPACE and 3D FLAIR.
Statistical analysis
The data were entered on Microsoft Excel spreadsheet and was analyzed using Epi Info 7.2.2.2 Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (US) for windows. The discrete variables were expressed regarding frequencies, proportions, and percentages with 95% confidence interval. The continuous variables were expressed as means ± standard deviation. The sensitivity of 3D T1-SPACE, 3D T1-MPRAGE, and 3D FLAIR was calculated and compared. The level of agreement between these sequences was assessed by kappa coefficient. P < 0.05 was taken as statistically significant.
Ethical considerations
Prior permission was taken from the Institutional Ethical Committee before commencing the study. Informed consent was taken from the participants of the study. All information collected was for research work, and personal identifiers were omitted to maintain confidentiality and anonymity of the patients.
RESULTS
A total of 30 patients were enrolled in the study. The age of patients in our study ranged from 15 years to 80 years. The mean age was 35.66 ± 16.03 years.
Most of the patients (n = 10) were in the range of 21-30 years comprising 33.3% of total. There were 17 male (56.6%) and 13 female (43.3%) patients. The most frequent complaints were fever (90%), altered sensorium (63.3%) and headache (53.3%). The CSF analysis revealed positive CSF findings in 28 (93.3%) cases and was normal in 2 (6.6%) cases. The MTBC was detected in four patients (13.3%), and ADA was positive in three patients (10%). The findings observed on conventional sequences included hydrocephalous (40%), infarct (30%), and hemorrhage (3.33%).
The leptomeningeal enhancement was observed in 26 patients out of total 30 patients in basal cisterns and Sylvian fissures on postcontrast images [Table 1].

3D T1-SPACE and 3D-FLAIR sequences are clearly better in demonstrating leptomeningeal enhancement than 3D T1-MPRAGE which failed to demonstrate enhancement in 6 (23%) cases. Leptomeningeal enhancement was seen along left Sylvian fissure and basal cisterns better appreciable on 3D T1-SPACE (Image A) and 3D FLAIR (Image C), respectively [Figure 1]. The level of agreement between two radiologists has been found to be excellent for leptomeningeal enhancement along basal cisterns and Sylvian fissures on 3D T1-SPACE (K - 0.780 [confidence interval: 0.569–0.991]), 3D-FLAIR (K - 0.917 [confidence interval: 0.836–0.998]) and 3D T1-MPRAGE [K - 0.845 [confidence interval: 0.74–0.95]).
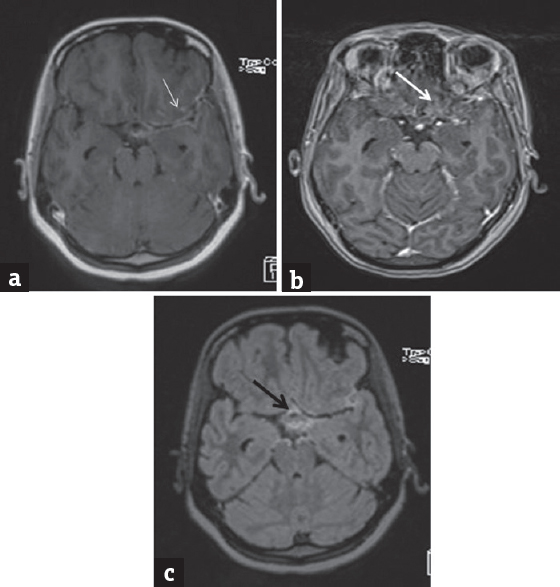
- A 24-year-old female with chief complaints fever, headache for 1 month and altered behaviour for 15 days. (a) Three-dimensional T1-SPACE shows subtle leptomeningeal enhancement along crural cisterns and definite leptomeningeal enhancement along left sylvian fissure (thin white arrow). (b) Three-dimensional T1-magnetization prepared rapid gradient echo shows no definite enhancement (thick white arrow). (c) Three-dimensional fluid-attenuated inversion recovery shows definite enhancement in basal cisterns (black arrow) and subtle enhancement along left sylvian fissure
Leptomeningeal enhancement was also observed along cerebral convexities which was present in 8 out of 30 cases. Out of 8 patients, 4 patients had enhancement along cerebral convexities as well as Sylvian fissure and basal cisterns. 3D T1-SPACE depicted leptomeningeal enhancement in all the 8 (100%) patients under study whereas 3D FLAIR failed to depict leptomeningeal enhancement in all the 8 (100%) patients as demonstrated in [Figure 2]. Both the radiologists assigned score 2 in 4 (50%) patients out of total 8 patients on MPRAGE sequence. The level of agreement between two radiologists has been found to be excellent for leptomeningeal enhancement along cerebral convexities on 3D T1-MPRAGE (K - 0.750 [confidence interval: 0.524–0.976]).
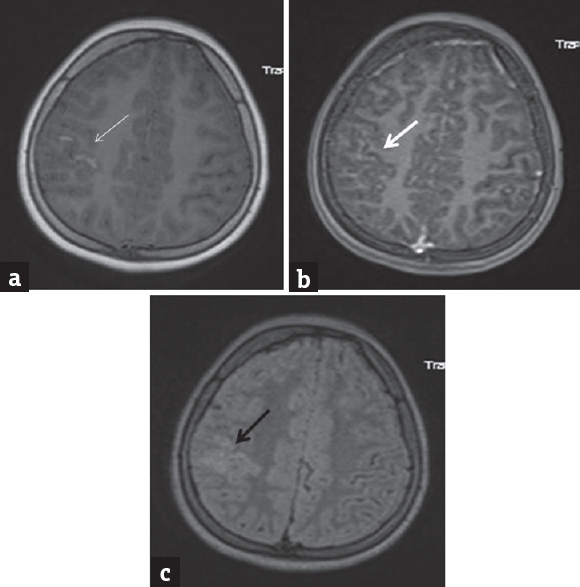
- A 27-year-old female with fever, headache for 8 days. (a) Three-dimensional T1-SPACE demonstrates definite leptomeningeal enhancement along cerebral convexity on the right side (thin white arrow). (b) Three-dimensional T1-magnetization prepared rapid gradient echo shows enhancement indistinguishable from enhancement (thick white arrow). (c) Three-dimensional fluid-attenuated inversion recovery shows only ill-defined enhancing area (black arrow)
For calculating sensitivity, the findings on 3D T1-SPACE, 3D FLAIR, and 3D T1-MPRAGE are compared with CSF findings separately [Chart 1].
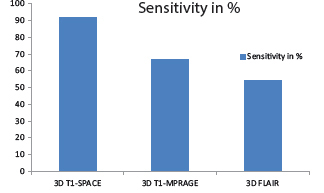
- Sensitivity of three-dimensional T1-SPACE, three-dimensional fluid-attenuated inversion recovery and three-dimensional T1-magnetization prepared rapid gradient echo
Additional findings include (1) Nodular and ring-enhancing lesions in 12 (40%) patients appreciated on 3D T1-SPACE as compare to 3D T1-MPRAGE and 3D FLAIR sequence as demonstrated in [Figure 3]. (2) Dural venous sinus thrombosis in 2 (6.6%) patients out of total 30 patients was demonstrated with 3D T1-MPRAGE and 3D T1-SPACE sequences.
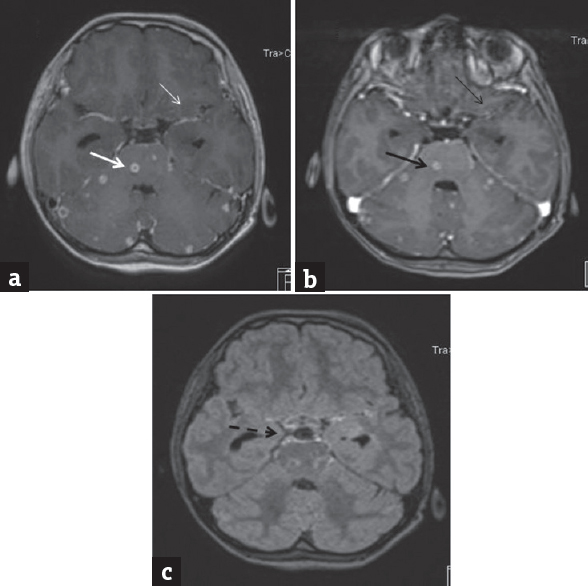
- A 36-year-old female with fever and headache. (a) Three-dimensional T1-SPACE shows definite leptomeningeal enhancement along perimesencephalic cisterns, sylvian fissures (thin white arrow). Nodular and ring enhancing lesions are delineated (thick white arrow). (b) Three-dimensional T1-magnetization prepared rapid gradient echo - subtle enhancement along the left sylvian fissure (thin black arrow) and parenchymal lesions (thick black arrow). (c) Three-dimensional fluid-attenuated inversion recovery - leptomeningeal enhancement along perimesencephalic cisterns, Sylvian fissures (interrupted black arrow)
DISCUSSION
The most common type of CNS disorder is meningitis.[7] For evaluation of meningeal diseases contrast enhanced T1-W MR imaging has been the standard.[8] 3D MPRAGE is the most widely used T1-weighted 3D gradient echo sequence that incorporates a magnetization prepared inversion pulse to increase T1 weighting. It can give excellent contrast, between gray matter (GM) and white matter (WM) than with T1-weighted spin echo sequence.[9] The depiction of meningeal enhancement becomes difficult because of masking by enhancing cortical vessels, thus it is a major drawback of 3D MPRAGE sequence.[10]
3D T2-FLAIR can generate 3D volume data with ability to acquire thinner section images in any plane, thus minimizing the partial volume effect between small lesions and surrounding tissue. It is valuable in evaluation of meningitis because of less incidence of CSF motion artifacts.[5] The drawback of PCFLAIR sequence is difficulty in differentiation between meningeal disease and underlying hyperintense edema.[11]
T1-W SPACE is a 3D fast spin-echo sequence in which refocusing of the transverse magnetization is done by radiofrequency pulse, is least affected by magnetic field in homogeneities, and shows the absence of flow-related signal from vessels.[12] In this multiple refocusing, pulses are applied which provide magnetization transfer (MT) effect. This MT effect causes suppression of signal intensity from white matter of brain resulting in better delineation of lesions.[13] The residual T2 blurring effect results in obscuration of gray and white matter junction resulting in less differentiation between gray and white matter.[14]
This study has been found to be helpful and has shown the superiority of 3D T1-SPACE in the MR evalution of meningeal pathologies.
In a study done by Aneel Kumar Vaswani et al.,[15] they observed that sensitivity and specificity of postcontrast FLAIR sequence was 96% and 85.71%, respectively. The sample size of our study, sensitivity and specificity of postcontrast FLAIR is less as compared with their study. Tsuchiya et al.,[8] Griffiths et al.,[16] Ercan et al.,[17] Parmar et al.,[18] Ahmad et al.,[19] Vaswani et al.,[15] and Lee et al.[20] studies have shown similar results of improved detection by FLAIR sequence as compared to T1 W sequence.
Alesssandra Splendiani et al.[7] did a study on 27 patients. The sensitivity and specificity of postcontrast FLAIR is 100% whereas the sensitivity and specificity of postcontrast T1W is 50% and 100%, respectively. The sensitivity of our postcontrast FLAIR is less as compared with this study and the sensitivity of postcontrast T1W is almost comparable with 3D T1-MPRAGE of our study. A study done by Singh et al.[21] and Galassi et al.[4] had found that T1 W MR imaging is superior to FLAIR imaging in the detection of leptomeningeal diseases.
Another study was done by Jeevanandham et al.[22] on 78 patients with suspicion of meningeal abnormalities. They observed that 3D T1-SPACE was useful in detecting meningeal abnormalities along sulci whereas 3D T2-FLAIR was useful in detecting meningeal abnormalities along basal cisterns. The sample size of our study is less as compared to their study. Our study shows that 3D T1-SPACE is more sensitive in detecting leptomeningeal enhancement along basal cisterns, Sylvian fissure and along cerebral convexities. Fukuoka et al.[10] were done study on 12 patients with leptomeningeal disease. Score 3 had been given in 9 (75%) and in 2 (16.66%) patients on 3D T2-FLAIR and MPRAGE sequences, respectively. Komada et al.,[6] Kato et al.[13] and Chang et al.[12] had found that SPACE images are better for detecting meningeal, brain metastases and small enhancing lesions, respectively. Rastogi et al.[11] found that postcontrast T2 FLAIR is better than postcontrast T1 GRE sequence in patients with tumours and shows more extensive enhancement. Brant-Zawadzki et al.[9] found that MPRAGE sequence may be an alternative to T1-weighted SE imaging because of better GM and WM differentiation. Kioumehr et al.[23] and Quint et al.[3] studied patterns of meningeal enhancement and found that infectious meningitis presents as leptomeningitis.
CONCLUSION
3D T1-SPACE is better in delineating leptomeningeal enhancement along basal cisterns, Sylvian fissure and also along cerebral convexities. 3D T1-SPACE was also found to be better in delineating the nodular and ring-enhancing lesions in brain. The 3D T1-SPACE should be included in the routine postcontrast examination of the MRI Brain in the evaluation of meningitis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Gd-DTPA-enhanced MR imaging of the brain in patients with meningitis: Comparison with CT. AJNR Am J Neuroradiol. 1990;11:69-76.
- [Google Scholar]
- Patterns of contrast enhancement in the brain and meninges. Radiographics. 2007;27:525-51.
- [Google Scholar]
- Magnetic resonance imaging of normal meningeal enhancement at 1.5 T. Acad Radiol. 1996;3:463-8.
- [Google Scholar]
- Intracranial meningeal disease: Comparison of contrast-enhanced MR imaging with fluid-attenuated inversion recovery and fat-suppressed T1-weighted sequences. AJNR Am J Neuroradiol. 2005;26:553-9.
- [Google Scholar]
- The technical and clinical features of 3D-FLAIR in neuroimaging. Magn Reson Med Sci. 2015;14:93-106.
- [Google Scholar]
- Contrast-enhanced MR imaging of metastatic brain tumor at 3 tesla: Utility of T(1)-weighted SPACE compared with 2D spin echo and 3D gradient echo sequence. Magn Reson Med Sci. 2008;7:13-21.
- [Google Scholar]
- Contrast-enhanced FLAIR in the early diagnosis of infectious meningitis. Neuroradiology. 2005;47:591-8.
- [Google Scholar]
- FLAIR MR imaging for diagnosing intracranial meningeal carcinomatosis. AJR Am J Roentgenol. 2001;176:1585-8.
- [Google Scholar]
- MP RAGE: A three-dimensional, T1-weighted, gradient-echo sequence – Initial experience in the brain. Radiology. 1992;182:769-75.
- [Google Scholar]
- Comparison of the added value of contrast-enhanced 3D fluid-attenuated inversion recovery and magnetization-prepared rapid acquisition of gradient echo sequences in relation to conventional postcontrast T1-weighted images for the evaluation of leptomeningeal diseases at 3T. AJNR Am J Neuroradiol. 2010;31:868-73.
- [Google Scholar]
- Can postcontrast-T2 FLAIR be a boon over postcontrast-T1GRE images in MR brain imaging? J Neuroinfect Dis. 2016;7:5.
- [Google Scholar]
- Contrast Enhanced 3D T1-Weighted SPACE: Pictorial Essay of Appearances, Advantages and Disadvantages Compared with Conventional Contrast Enhanced 3D T1-Weighted Imaging (MPRAGE) 2012. Available from: http://www.ranzcr.edu.au
- [Google Scholar]
- Usefulness of contrast-enhanced T1-weighted sampling perfection with application-optimized contrasts by using different flip angle evolutions in detection of small brain metastasis at 3T MR imaging: Comparison with magnetization-prepared rapid acquisition of gradient echo imaging. AJNR Am J Neuroradiol. 2009;30:923-9.
- [Google Scholar]
- Which to choose for volumetry: MPRAGE or SPACE? Proc Int Soc Mag Reson Med 2011:19.
- [Google Scholar]
- Diagnostic accuracy of contrast-enhanced FLAIR magnetic resonance imaging in diagnosis of meningitis correlated with CSF analysis. ISRN Radiol 2014 2014 578986
- [Google Scholar]
- Contrast-enhanced fluid-attenuated inversion recovery imaging for leptomeningeal disease in children. AJNR Am J Neuroradiol. 2003;24:719-23.
- [Google Scholar]
- Diagnostic value of contrast-enhanced fluid-attenuated inversion recovery MR imaging of intracranial metastases. AJNR Am J Neuroradiol. 2004;25:761-5.
- [Google Scholar]
- Contrast-enhanced flair imaging in the evaluation of infectious leptomeningeal diseases. Eur J Radiol. 2006;58:89-95.
- [Google Scholar]
- Differentiation of leptomeningeal and vascular enhancement on post-contrast FLAIR MRI sequence: Role in early detection of infectious meningitis. J Clin Diagn Res. 2015;9:TC08-12.
- [Google Scholar]
- Importance of contrast-enhanced fluid-attenuated inversion recovery magnetic resonance imaging in various intracranial pathologic conditions. Korean J Radiol. 2016;17:127-41.
- [Google Scholar]
- MR imaging of leptomeningeal metastases: Comparison of three sequences. AJNR Am J Neuroradiol. 2002;23:817-21.
- [Google Scholar]
- Comparison of post-contrast 3D-T1-MPRAGE, 3D-T1-SPACE and 3D-T2-FLAIR MR images in evaluation of meningeal abnormalities at 3-T MRI. Br J Radiol. 2017;90:20160834.
- [Google Scholar]
- Postcontrast MRI of cranial meninges: Leptomeningitis versus pachymeningitis. J Comput Assist Tomogr. 1995;19:713-20.
- [Google Scholar]






