Translate this page into:
Three-territory infarct in Trousseau syndrome: A case series and review of literature
*Corresponding author: Manoj Kumar Nayak, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. tuna.manoj@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alagappan A, Naik S, Bhoi SK, Sahoo B, Pitchaimuthu A, Nayak M. Three-territory infarct in Trousseau syndrome: A case series and review of literature. J Neurosci Rural Pract. doi: 10.25259/JNRP_294_2024
Abstract
Multiple arterial territorial cerebral infarcts of unknown etiology are typically described as cardioembolism, a common etiology attributed to atrial fibrillation. However, there is under evaluation of the association of multiple territorial arterial infarcts in the brain in association with malignancy. In the existing literature study, small lesions affecting several arterial regions in the brain can be the hallmarks of cancer-associated hypercoagulation-induced embolism. Herein, we report a series of three cases, who presented with multiple arterial territorial infarcts (three-territory sign) in the brain in a known case of malignancy.
Keywords
Case report
Hypercoagulation
Malignancy
Stroke
Three-territory infarcts
Trousseau syndrome
INTRODUCTION
Between 25% and 33% of ischemic strokes are categorized as embolic strokes of an unknown source because no recognized etiology is identified.[1] Recent studies reported that 5–10% of these patients have active malignancy.[2] Cerebrovascular disease is the second most frequent neurological condition in cancer patients, following metastases.[3] The cancer patients have cerebrovascular ischemia up to 15%[4] and twice-as-high six-month cumulative incidence of ischemic stroke compared to the general population.[5] Even though they are most commonly linked to a cardioembolic etiology, multiple territorial cerebral infarcts are a characteristic of stroke associated with malignancy. Finelli et al. adapted this as a “three-territory sign (TTS)” and suggested it as a radiological marker for malignancy-associated stroke.[6] This case series presents three cases of malignancy presented with TTS.
CASE SERIES
Case 1
A 70-year-old gentleman, a known case of carcinoma stomach with post-explorative laparotomy, presented to our hospital with complaints of paraparesis. He had a previous history of one episode of unconsciousness and focal seizures one month back. Central nervous system (CNS) examination showed reduced power in the bilateral lower limbs with preserved sensory perceptions. Cranial nerve and cortical examination were normal. The magnetic resonance imaging (MRI) of the brain showed multiple ill-defined T2 and fluid-attenuated inversion recovery (FLAIR) hyperintense lesions in bilateral frontoparietal lobes, corpus callosum, and adjacent periventricular white matter showing restricted diffusion without postcontrast enhancement. No blooming was noted in the susceptibility-weighted imaging sequence. At the time of flight imaging, no large vessel occlusion was present [Figure 1]. No evidence of atrial fibrillation on electrocardiogram (ECG) and echocardiography showed mild reduced systolic function of the left ventricle with an ejection fraction of 49%. No evidence of thrombus was present.
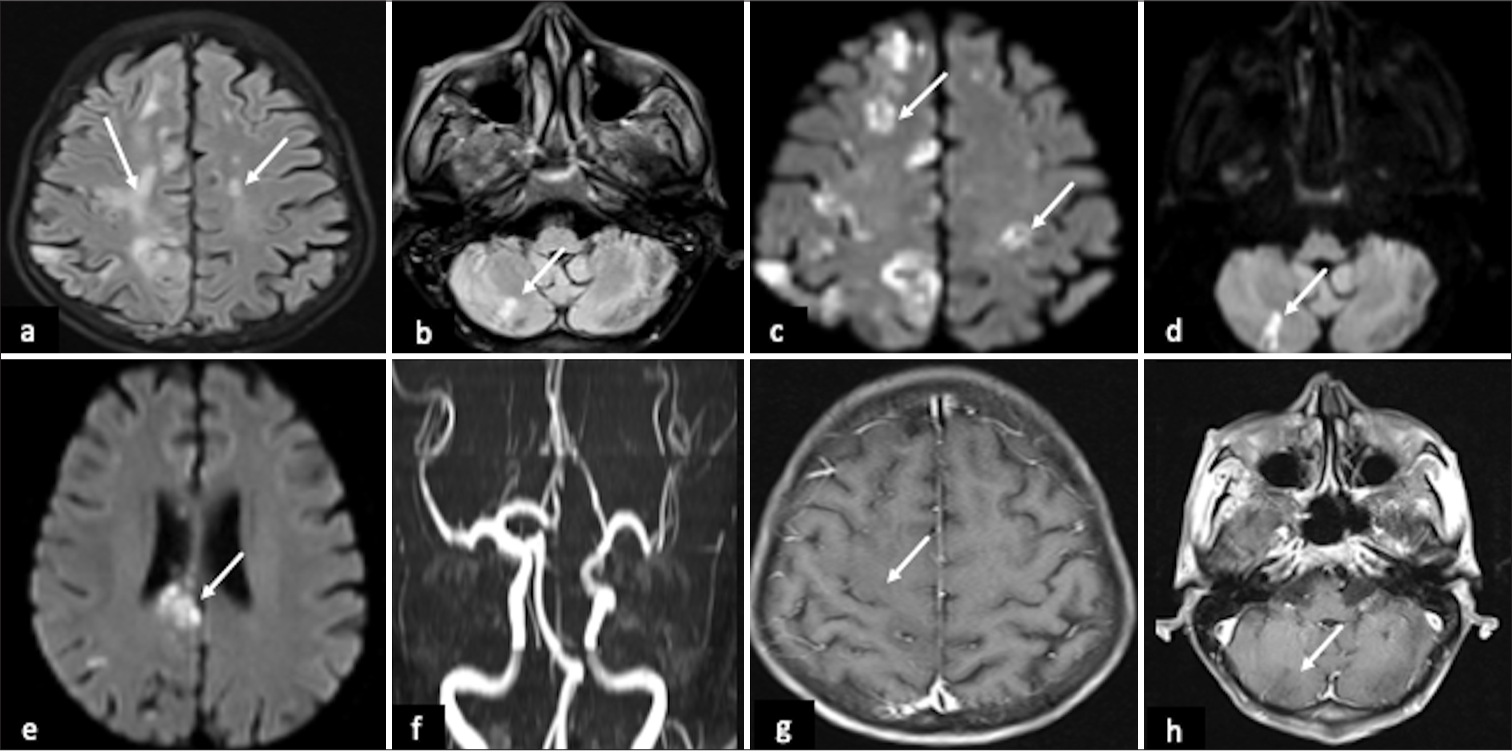
- Magnetic resonance imaging (MRI) images showed the “three-territory sign” in malignancy-associated stroke. MRI of the brain images showing (a and b) multiple ill-defined fluid-attenuated inversion recovery (FLAIR) hyperintense patchy and irregular lesions in bilateral frontoparietal cortical and subcortical regions, right cerebellar hemisphere (white arrows), (c-e) the corresponding FLAIR hyperintense lesions showed restricted diffusion on DWI (white arrows). (f) On-time of flight image, no apparent stenosis/occlusion were evident. (g and h) There was no evidence of post-contrast enhancement (white arrows).
Case 2
A 69-year-old gentleman with a known case of interstitial lung disease with superimposed adenocarcinoma of the lung was sent for staging evaluation without specific CNS/cardiovascular system complaints. Pulmonary arterial hypertension with the right ventricular hypertrophy was seen in echocardiography. No evidence of thrombus was seen. CNS examination showed left homonymous hemianopia with macular sparing and mildly reduced power in the right upper and lower limbs. MRI brain showed multiple T2/FLAIR hyperintense foci with restricted diffusion in bilateral centrum semiovale, frontoparietal subcortical white matter, and left corona radiata. A wedge-shaped T2/FLAIR hyperintensity was seen in the right occipital lobe, which showed diffusion restriction and gyriform enhancement on post contrast study [Figure 2].

- Magnetic resonance imaging (MRI) images showed the “three-territory sign” in malignancy-associated stroke MRI of the brain images (a and b) showing multiple tiny fluid-attenuated inversion recovery (FLAIR) hyperintense foci in bilateral centrum semiovale, frontoparietal subcortical white matter, and left corona radiata (white arrows) and (c) wedge-shaped FLAIR hyperintensity in the right occipital lobe (white arrow). (d-i) the corresponding FLAIR hyperintense lesions showed restricted diffusion on DWI (white arrows). (j and k) gyriform enhancement was noted in the right occipital lobe and left frontal lobe lesion on post-contrast study (white arrows).
Case 3
A 47-year-old gentleman, a known case of periampullary carcinoma, post biliary stenting, presented with left-sided hemiparesis and deviation of angle of mouth to the right side. He was on chemotherapy when he noticed the onset of neurological symptoms. Examination showed left-sided upper motor neuron type of facial palsy and reduced power on the left upper and lower limbs. His hemoglobin was 6 g/dL with a total leucocyte count of 25000 and elevated D-dimer, fibrinogen, and C-reactive protein levels. Screening for deep vein thrombosis was negative. MRI brain showed multiple small T2 and FLAIR hyperintense foci in the bilateral centrum semiovale and right front-parietal-temporal subcortical white matter, showing restricted diffusion. A wedge-shaped T2/FLAIR hyperintensity with restricted diffusion was noted in the right frontotemporal region and insula. An incidental finding of an arachnoid cyst in the left frontoparietal convexity was noted [Figure 3]. ECG and echocardiography were unremarkable. The details of our cases were summarized in Table 1.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Clinical history | Stomach carcinoma | Interstitial lung disease with adenocarcinoma of lung | Periampullary carcinoma |
| Complaints | Paraparesis one episode of unconsciousness and focal seizure | Nil | Left-sided hemiparesis and deviation of angle of mouth to right side |
| Examination | Reduced power in the bilateral lower limbs | Left homonymous hemianopia with macular sparing and mild reduced power in the right upper and lower limb. | Left-sided upper motor neuron type of facial palsy and reduced power on left upper and lower limb. |
| MRI findings | Multiple ill-defined T2 and FLAIR hyperintense lesions in bilateral frontoparietal lobes, corpus callosum, and adjacent periventricular white matter showing restricted diffusion. | Multiple T2/FLAIR hyperintense foci with restricted diffusion in bilateral centrum semiovale, frontoparietal subcortical white matter, and left corona radiata. A wedge-shaped T2/FLAIR hyperintensity showing diffusion restriction in right occipital lobe with gyriform post-contrast enhancement. |
Multiple small T2 and FLAIR hyperintense foci in the bilateral centrum semiovale and right front-parietal-temporal subcortical white matter, showing restricted diffusion. A wedge-shaped T2/FLAIR hyperintensity with restricted diffusion was noted in the right frontotemporal region and insula |
MRI: Magnetic resonance imaging, FLAIR: Fluid-attenuated inversion recovery.

- Magnetic resonance imaging (MRI) images showed the “three-territory sign” in malignancy-associated stroke MRI brain images (a and b) showing multiple small fluid-attenuated inversion recovery (FLAIR) hyperintense foci in the bilateral centrum semiovale, the right front-parietal-temporal subcortical white matter, and right cerebellar parenchyma (white arrows) and (a) wedge-shaped FLAIR hyperintensity in the right frontotemporal region and insula (thin black arrow). (c-h) showing diffusion restriction (white arrows). (a) Incidental arachnoid cyst in the left frontoparietal convexity (thick black arrow).
DISCUSSION
The hypercoagulable condition associated with malignancy is often referred to as “Trousseau syndrome.”[7] While cancer is commonly linked to venous thrombosis, new research indicates that it also poses a substantial risk for arterial thromboembolism.[8] The pathophysiology of arterial thrombosis in cancer patients involves hypercoagulability, chemotherapy, infections, paraneoplastic diseases, and direct effects of the tumor.[6] In our case 3, where he was on chemotherapy, a hypercoagulable state was evident in laboratory parameters. In our cases, all three patients were known cases of malignancy. Two of them presented with sudden onset neurological deficits, while one patient did not have any specific neurological complaints. However, on examination, all three patients had neurological deficits. Cardioembolic screening was negative in all of our patients. All three patients had anterior and one posterior circulation (three-territory) involvement. The term TTS refers to ischemic strokes that affect the bilateral anterior and posterior circulations, among other three vascular territories.[6] In a study by Nouh et al., the TTS was found to be quite specific (96.4%) for hypercoagulability resulting from cancer (Trousseau syndrome) but not sensitive (23.4%). Notably, patients with underlying malignancy in the same study had a six-fold higher likelihood of observing the TTS compared to patients with underlying atrial fibrillation who might have experienced multi-territory cardioembolic ischemic stroke.[9]
Moreover, stroke risk varies according to the kind of cancer. It is higher in those that are most associated with a risk of venous thromboembolism, such as lung and pancreatic cancer.[10] It has been reported that adenocarcinoma in the lung is mainly associated with hypercoagulability.[11] In our case, case 3 had severe neurological manifestations when compared to the other two patients, and the histological type was adenocarcinoma lung. The underlying pathophysiology with primary lung malignancies which are situated around the pulmonary veins or heart chambers can invade and embolize to brain.[8] It is also becoming more well-acknowledged that stroke may be the first sign of malignancy. In a study, the risk of an ischemic stroke rose by 59% in the year preceding a cancer diagnosis, based on Medicare claims data linked to the American Cancer Registry.[8] However, in our cases, all three patients were known cases of malignancy and presented with neurological deficits in later stages. Cancer is often disregarded as a cause of stroke and is usually not detected until a second incident occurs. Since cancer-associated hypercoagulation may be the first sign of latent cancer, it is essential to diagnose the condition. Heparin therapy is beneficial in preventing thrombotic events, such as stroke. Work-up should be done for D-dimer and fibrinogen levels; tumor biomarkers; screening for deep vein thrombosis; computed tomography of the chest, abdomen, and pelvis; and positron emission tomography scan when other tests are negative, as TS-related stroke may be the precursory symptom of an undetected malignancy.[6]
CONCLUSION
When infarcts affect three distinct vascular territories without known embolic cause or comorbidity linked to these lesions, it strongly suggests hypercoagulation stroke related to malignancy. Timely identification is critical because heparin effectively prevents thrombotic episodes in cancer-associated hypercoagulation. The three-territory diffusion-weighted imaging infarct pattern can offer a crucial diagnostic hint to an otherwise overlooked stroke etiology.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that AI was used for editing the manuscript; however, it was not used for writing, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cancer and embolic stroke of undetermined source. Stroke. 2021;52:1121-30.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in cancer diagnoses among inpatients hospitalized with stroke. J Stroke Cerebrovasc Dis. 2013;22:1146-50.
- [CrossRef] [PubMed] [Google Scholar]
- Stroke risk factor, pattern and outcome in patients with cancer. Acta Neurol Scand. 2006;114:378-83.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebrovascular complications in patients with cancer. Medicine (Baltimore). 1985;64:16-35.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of arterial thromboembolism in patients with cancer. J Am Coll Cardiol. 2017;70:926-38.
- [CrossRef] [PubMed] [Google Scholar]
- Three-territory DWI acute infarcts: Diagnostic value in cancer-associated hypercoagulation stroke (Trousseau syndrome) AJNR Am J Neuroradiol. 2016;37:2033-6.
- [CrossRef] [PubMed] [Google Scholar]
- Trousseau's syndrome: Multiple definitions and multiple mechanisms. Blood. 2007;110:1723-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arterial thromboembolic events preceding the diagnosis of cancer in older persons. Blood. 2019;133:781-9.
- [CrossRef] [PubMed] [Google Scholar]
- Three territory sign: An MRI marker of malignancy-related ischemic stroke (Trousseau syndrome) Neurol Clin Pract. 2019;9:124-8.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic signatures in cancer. N Engl J Med. 2019;381:1378-86.
- [CrossRef] [PubMed] [Google Scholar]
- Association of cancer cell type and extracellular vesicles with coagulopathy in patients with lung cancer and stroke. Stroke. 2018;49:1282-5.
- [CrossRef] [PubMed] [Google Scholar]






