Translate this page into:
The Pattern of Psychiatric Morbidity in Chronic Obstructive Pulmonary Disease: A Cross-Sectional, Case–Control Study from a Tertiary Care Hospital in Kashmir, North India
Address for correspondence: Dr. Shabir Ahmad Dar, Department of Psychiatry, Government Psychiatric Diseases Hospital Srinagar, G4, Residential Quarters, Srinagar - 190 001, Jammu and Kashmir, India. E-mail: shabir1055@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Psychiatric morbidity has an increased prevalence in chronic obstructive pulmonary disease (COPD). Patients overall psychosocial status plays an important role in the development of depression which, when major, is said to occur in 19%–42% of cases of COPD. We aimed to study patterns of psychosocial issues in patients with COPD.
Materials and Methods:
This study was conducted over a period of 6 months in an Outpatient Department of Government Chest Disease Hospital Srinagar. A total of 100 COPD patients and 100 sex- and age-matched controls were included in this study and compared. The diagnosis of COPD was assessed by spirometry. Patterns of psychiatric morbidities were assessed using the Mini-International Neuropsychiatric Interview.
Results:
The frequency of psychiatric comorbidities was significantly higher (P < 0.001) in COPD patients (47%) as compared to controls (12%). The highest frequency of psychiatric morbidities in COPD patients was major depressive episode in 28% in comparison to 9% of controls. Other morbidities include panic disorder, dysthymia, generalized anxiety disorder, and suicidality.
Conclusion:
The frequency of psychiatric morbidities is increased in COPD patients as compared to controls. We recommend that all patients with COPD should be screened for psychiatric morbidity as there is enough scope for psychiatric services to be made available to these patients.
Keywords
Chronic obstructive pulmonary disease
depression
panic disorder
suicidality
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a progressive, partially reversible, preventable, and treatable lung disease characterized by long-term breathing problems which typically worsens over time. The main symptoms include shortness of breath and cough with sputum production.[12] Acute exacerbations and frequent comorbidities contribute to the overall severity in individual patients eventually everyday activities, such as walking or getting dressed, become difficult.[3]
The prevalence of COPD among Indian males is 5% and 3.2% in females. It usually affects over 35 years of age.[4] Smoking is the most common cause of COPD with factors such as air pollution and genetics playing a minor role.[5] Long-term exposures to the irritants start an inflammatory response in the lungs resulting in narrowing of the small airways and breakdown of lung tissue.[6]
The diagnosis of COPD is based on poor airflow as measured by lung function tests in contrast to asthma, where airflow reduction does not improve much with the use of a bronchodilator.[78] COPD is diagnosed on the basis of symptoms, pulmonary function tests and the finding of a post-bronchodilator forced expiratory volume in 1 (FEV1)/forced vital capacity (FVC) <70%. Chronic inflammation of the small bronchoalveolar tree leads to progressive destruction of the lungs leading to physical disability. This often leads to psychiatric comorbidities such as depression and anxiety disorders and poor quality of life in such patients.[910]
Chronic inflammation followed by hypoxemia leads to disruption in noradrenergic and dopaminergic synthesis, release, and replenishment that may lead to symptomatology seen in depressive disorders.[11] Anxiety and depressive symptoms are common in patients affected by COPD, even when their disease is mild in terms of FEV1 and respiratory symptoms. The etiology between COPD and depression seems to be complex and bidirectional.[12]
The prevalence of depression varies widely in different populations, which could be attributed to different ethnicity, different cultural backgrounds, and heterogeneous demography of the study populations and different screening tools.
We undertook this study to estimate the prevalence of psychiatric morbidity in patients with a diagnosis of COPD presenting to the outpatients department at the postgraduate department of chest disease Srinagar, Jammu and Kashmir. To the best of our knowledge, this is the first study to look into the psychological issues in patients of COPD from the lone tertiary care hospital in Kashmir Valley.
MATERIALS AND METHODS
Postgraduate department of chest diseases provides tertiary medical care to the whole of Kashmir region along with some adjoining areas of Jammu and Ladakh, the population of about 6 million. One hundred consecutive consenting patients diagnosed with COPD were included in the study. The study was approved by the Institutional Ethical Committee of Government Medical College Srinagar. The diagnosis of COPD was made by consultant pulmonologist using clinical, biochemical, radiological, and pulmonary function tests. It was a hospital-based, cross-sectional, case–control study conducted from October 2015 to March 2016.
An equal number of age- and gender-matched normal healthy volunteers unrelated to patients were randomly assigned and were taken in the comparison group. Patients with uncontrolled chronic physical illnesses such as hypertension, hypothyroidism, and diabetes mellitus were excluded from the study. Those not consenting, on corticosteroids or oral contraceptives, or having an acute exacerbation of COPD were excluded from the study. Detailed history, physical examination, and relevant investigations were done by the resident psychiatrist before screening for any psychiatric diagnosis.
An informed written consent was taken from participants and was briefed about the study before participation. All of the cases were interviewed for sociodemographic parameters such as age, gender, and socioeconomic level. Smoking history was taken as number of pack-years smoked in both groups. Both the cases and comparison group were evaluated to investigate the psychiatric morbidity using Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) criteria by means of Mini-International Neuropsychiatric Interview (M.I.N.I.) is a short structured diagnostic interview, developed jointly by psychiatrists and clinicians in the United States and Europe, for DSM-IV and ICD-10 psychiatric disorders. administered by qualified psychiatrist. The choice of MINI as an instrument was based on its high levels of reliability and validity, which have been reported in several studies.[13]
The MINI is a structured interview tool, designed to evaluate the presence of psychiatric disorders according to Axis I, of the DSM-IV.
Statistical analysis
During 6-month study, a total of 100 patients with COPD and 100 ages and sex-matched controls were enrolled as per our inclusion and exclusion criteria. The sociodemographic and clinical variables of patients and controls were tabulated in an excel sheet and results were statistically analyzed. Data were analyzed using the SPSS version 20.0. P < 0.05 was taken as statistically significant.
RESULTS
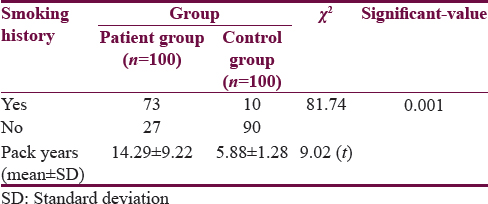
An equal number of cases and controls were recruited for the study. Mean age of patients was 56.24 years (ranges between 42–72 years) in comparison to controls 54.78 years. Majority of cases and controls were from rural background belonging to middle socioeconomic class. A significant difference was found with regards to cigarette smoke exposure [Table 1]. About 73% of case group were smokers as compared to only 10% in the control group. The mean pack-years of smoking were significantly higher in cases (14.29 ± 9.22) as compared to (5.88 ± 1.28) in control group.
The average FEV1 in our cases was 37.64% ± 12.62% as compared to 89.10% ± 1.64% in controls. The mean FEV1/FVC ratio in our cases was 54.85% ± 10.32% as compared to 97.20% ± 1.88% in controls.
47% of patients in COPD group were having a morbid psychiatric illness as compared to only 12% of healthy voluntary controls in the comparison group [Table 2].

The frequency of psychiatric morbidity was highest for major depressive episode with a prevalence of 28% followed by panic disorder in both the cases and the control group [Table 3]. The frequency of psychiatric morbidity in COPD patients increased with the severity of the illness.

DISCUSSION
COPD is characterized by progressive obstruction to airflow due to pulmonary inflammatory reactions to noxious particles.[14] COPD is not only the leading cause of morbidity and mortality worldwide but also associated with considerable social and economic burden as well as significant impairments in occupational capacity and quality of life.[15] Patients with diagnosis COPD, especially with advanced conditions, usually suffer from differing degrees of depression, in response to unfavorable health status, an increased degree of immobility and dependence on others, and to a worsening quality of life. The overall impact of the psychosocial status of patients plays an important role in the development of depression which, when major, is said to occur in 19%–42% of cases.[1617]
Depression is a highly prevalent comorbidity in patients with COPD and its other associated negative aspects in the course of the disease. It contributes significantly to the social and economic burden of patients. Other studies also indicate that there is a high prevalence of anxiety and depression in patients with COPD (44.1%).[18] The reason for the higher prevalence of depression in patients with COPD seems to be the biological factors like increased levels of 5-hydroxyindoleacetic acid as reported by Sekiduka-Kumano et al.[19]
It has been seen that increased plasma 5-hydroxyindoleacetic acid levels are associated with poor lung function, hypoxia, and hypercapnia. Poor lung function is closely correlated with a poor Health-related quality of life and may result in depression. In COPD patients, it has been shown that hypoxia and/or hypercapnia induces oxidative stress and results in an increase of reactive oxygen species throughout the whole body including the lungs, brain, and muscles.[202122]
The other possible factors responsible for the increased prevalence of psychiatric comorbidities in COPD patients could be psychological factors such as low self-esteem and low self-worth resulting from suffering a chronic medical illness. Social factors such as social isolation and low productivity may also contribute to this increased prevalence.
In our study, 73% of cases were smokers compared to 10% in controls (P < 0.001). In a study in Northern Sweden by Lindberg et al., the prevalence of COPD among men who were smokers was 89%.[23] The mean pack years in cases was 14.29 ± 9.22 while in controls, it was 5.88 ± 1.28 (P = 0.001). These findings of ours are consistent with smoking being a risk factor in pathophysiology of COPD. It has been seen that smoking enhances the chances and intensity of COPD, makes routine activities effortful and full of stress, therefore increases the risk of depression in patients with COPD.[24]
Smoking and depression are linked in bidirectional manner. Individuals with depression are more likely to smoke, have a higher risk to commence smoking and find smoking cessation more difficult. Conversely, smokers are more likely to be depressed, which could be caused by the activation of nicotinic acetylcholine receptors, or direct inflammatory effects of smoking.[25]
In our study, cases had psychiatric comorbidity of 47% as compared to 12% in controls (P = 0.005). This was in unison with Sharma et al., where the prevalence of psychiatric comorbidity in cases was found to be around 44.8%.[26] The most frequent psychiatric comorbidity in our studied patients was major depressive episode with a frequency of 28%. Our study results are concordant with Negi et al. where depression was seen in 33.3% of patients.[27] The prevalence of depressive symptoms in COPD patients varies considerably. Mikkelsen et al.[28] found an incidence ranging from 6% to 57%, and Van Ede et al.[29] from 6% to 42%, whereas recent studies have found a range of 42%–57%.[3031] In a review of three studies, Solano et al.[32] had observed the prevalence of depression ranged from 37% to 71% of COPD patients and the cumulative prevalence rate of depression in our study is comparable with their results.
Little is known about the prevalence of depression in patients with COPD in India. A study done in Indian COPD patients has shown the cumulative prevalence of depression in 72% of patients.[33] However, studies from other countries reported the prevalence of depression in patients with COPD varying from 6% to 56%.[343536] The variation in the prevalence of depression in COPD can be partly attributed to the use of different measures for depression. Studies from other countries such as Japan and Turkey reported the prevalence of depression in patients with COPD ranging from 40.5% to 46.7%.[3738] Maurer et al. also found a prevalence of depression in COPD patients to vary from 10% to 42%.[39] The risk of depression in COPD patients is high in comparison to healthy individuals. The presence of under-recognized subclinical depression in patients with COPD is a major concern, as they are at the risk of developing major depression and may increase the burden of physical disability.[40]
Several factors can be attributed for developing depression in patients with COPD. Severe shortness of breath, progressive and irreversible condition and associated hypoxia may be responsible for organic causes of depression in severe COPD. In addition, advanced age, low socioeconomic condition, and the chronic nature of the disease may result in social isolation and leads to more depressive feelings.[41] In patients with COPD even after adjusting the severity, depression is responsible for fatigue, shortness of breath and disability.[39]
Panic disorder was the second-common diagnosis with a frequency of 9% in cases and only 3% of controls. Karajgi et al.,[42] in their study using the Structured Clinical Interview for DSM-III-R, found a prevalence rate of 8% for panic disorder which is 5.3 times as high as in the general population and the results are concordant with our results.[43] Moore and Zebb[44] on the other hand have however found an even higher rate of panic disorder (32%) using self-report measures of panic disorder symptoms based on DSM-IV criteria for panic disorder. Porzelius et al.[45] found that 37% of patients experienced a panic attack in the previous 3 weeks. Not only is anxiety highly common among COPD patients but the reverse is also true. The lifetime prevalence of the respiratory disease is higher in people with panic disorder (47%) than with other psychiatric diagnoses.[46]
Dysthymia, generalized anxiety disorder, and suicidality were the other morbid diagnosis. The prevalence of generalized anxiety disorder among patients with COPD ranges from 10% to 15.8% when using standard diagnostic procedures[474849] compared with lifetime rates of 3.6% to 5.1% in the general public.[5051] It has been reported that the severity of depression in patients with COPD is closely associated with suicidal ideation.[5253]
Therefore, it would be worthwhile to rank COPD patients in terms of current suicide risk. Taken together, the data suggest that a depressive status and the severity of COPD may be related to increased plasma 5-HIAA level in depressed COPD patients.
Limitations
It was a hospital-based study, and its results cannot be generalized for the community. The number of subjects enrolled in our study was not estimated by any statistical tool. The study was conducted in a single center.
CONCLUSION
In view of high psychiatric morbidity associated with COPD, there is enough scope for psychiatric services to be made available to these patients. In additions, personal involved in the treatment of these patients should be trained for early detection of psychiatric symptoms for better treatment outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would like to thank Dr. Mudasir Hassan, lecturer clinical psychology for his valuable statistical inputs.
REFERENCES
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. American journal of respiratory and critical care medicine. 2001;163:1256-76.
- [Google Scholar]
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163:1256-76.
- [Google Scholar]
- Chronic obstructive lung disease: A rising problem for the world. Pak J Chest Med. 2018;23:130-3.
- [Google Scholar]
- COPD: The unrecognized epidemic in India. J Assoc Physicians India. 2012;60(Suppl):14-6.
- [Google Scholar]
- Adequacy of inhaler technique in the patients of copd and asthma. KJMS. 2015;8:221.
- [Google Scholar]
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532-55.
- [Google Scholar]
- COPD diagnosis related to different guidelines and spirometry techniques. Respir Res. 2007;8:89.
- [Google Scholar]
- Chronic Obstructive Pulmonary Disease (COPD)- World Health Organization. Available from: http://ww.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- Alternative projections of mortality and disability by cause 1990-2020: Global burden of disease study. Lancet. 1997;349:1498-504.
- [Google Scholar]
- The association between depressive symptoms and acute exacerbations of COPD. Lung. 2009;187:128-35.
- [Google Scholar]
- Prevalence and impact of depression in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2006;12:113-7.
- [Google Scholar]
- Dyspnoea: A multidimensional and multidisciplinary approach. Eur Respir J. 2014;43:1750-62.
- [Google Scholar]
- The mini-international neuropsychiatric interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22-33.
- [Google Scholar]
- Burden and clinical features of chronic obstructive pulmonary disease (COPD) Lancet. 2004;364:613-20.
- [Google Scholar]
- Comparison of health-related quality of life between patients with chronic obstructive pulmonary disease and the general population. Scand J Caring Sci. 2013;27:905-12.
- [Google Scholar]
- Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167:60-7.
- [Google Scholar]
- Positive association between the plasma levels of 5-hydroxyindoleacetic acid and the severity of depression in patients with chronic obstructive pulmonary disease. BMC Psychiatry. 2013;13:159.
- [Google Scholar]
- COPD: Epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121:121S-6S.
- [Google Scholar]
- Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178:913-20.
- [Google Scholar]
- Prevalence and underdiagnosis of COPD by disease severity and the attributable fraction of smoking report from the obstructive lung disease in Northern Sweden studies. Respir Med. 2006;100:264-72.
- [Google Scholar]
- Depression, anxiety, and COPD: The unexamined role of nicotine dependence. Nicotine Tob Res. 2012;14:176-83.
- [Google Scholar]
- Systemic inflammation and comorbidity in COPD: A result of ‘overspill’ of inflammatory mediators from the lungs? Review of the evidence. Thora×. 2010;65:930-6.
- [Google Scholar]
- Psychiatric morbidity in chronic respiratory disorders in an Indian service using GMHAT/PC. Gen Hosp Psychiatry. 2013;35:39-44.
- [Google Scholar]
- Presence of depression and its risk factors in patients with chronic obstructive pulmonary disease. Indian J Med Res. 2014;139:402-8.
- [Google Scholar]
- Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD). A review. Nord J Psychiatry. 2004;58:65-70.
- [Google Scholar]
- Prevalence of depression in patients with chronic obstructive pulmonary disease: A systematic review. Thora×. 1999;54:688-92.
- [Google Scholar]
- The use of the hospital anxiety and depression scale (HADS) in patients with chronic obstructive pulmonary disease: A pilot study. N Z Med J. 2001;114:447-9.
- [Google Scholar]
- Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2001;21:80-6.
- [Google Scholar]
- A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
- [Google Scholar]
- Quality of life measurement for patients with diseases of the airways. Thora×. 1991;46:676-82.
- [Google Scholar]
- Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med. 2007;167:2345-53.
- [Google Scholar]
- Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27:788-94.
- [Google Scholar]
- The effects of depressed mood on smoking cessation: Mediation by postcessation self-efficacy. J Consult Clin Psychol. 2003;71:292-301.
- [Google Scholar]
- Prevalence of depressive symptoms in Japanese male patients with chronic obstructive pulmonary disease. Psychiatry Clin Neurosci. 2011;65:82-8.
- [Google Scholar]
- Anxiety and depression in COPD patients and correlation with sputum and BAL cytology. Multidiscip Respir Med. 2011;6:226-31.
- [Google Scholar]
- Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest. 2008;134:43S-56S.
- [Google Scholar]
- Prevalence of sub-threshold depression in elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2003;18:412-6.
- [Google Scholar]
- The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990;147:200-1.
- [Google Scholar]
- Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry. 1984;41:949-58.
- [Google Scholar]
- The catastrophic misinterpretation of physiological distress. Behav Res Ther. 1999;37:1105-18.
- [Google Scholar]
- Respiratory function, cognitions, and panic in chronic obstructive pulmonary patients. Behav Res Ther. 1992;30:75-7.
- [Google Scholar]
- Higher lifetime prevalence of respiratory diseases in panic disorder? Am J Psychiatry. 1991;148:1583-5.
- [Google Scholar]
- Psychiatric morbidity in patients with chronic airflow obstruction. Med J Aust. 1987;146:305-7.
- [Google Scholar]
- Specific psychiatric morbidity among patients with chronic obstructive pulmonary disease in a Nigerian general hospital. J Psychosom Res. 2001;50:179-83.
- [Google Scholar]
- Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: Applicability of GHQ-12. Gen Hosp Psychiatry. 2001;23:77-83.
- [Google Scholar]
- Dyspnea, anxiety, and depression in chronic respiratory impairment. Gen Hosp Psychiatry. 1992;14:20-8.
- [Google Scholar]
- DSM-III-R generalized anxiety disorder in the national comorbidity survey. Arch Gen Psychiatry. 1994;51:355-64.
- [Google Scholar]
- Randomized trial of paroxetine in end-stage COPD. Monaldi Arch Chest Dis. 2004;61:140-7.
- [Google Scholar]






