Translate this page into:
The home-based mirror therapy in the reduction of phantom limb pain in unilateral below-knee amputees
*Corresponding author: Alireza Taheri, Departement of Orthotics and Prosthetics , School Rehabilitation of Sciences, Isfahan University of Medical Sciences, Isfahan, Iran. taheri@rehab.mui.ac.ir
-
Received: ,
Accepted: ,
How to cite this article: Shariaty S, Taheri A. The home-based mirror therapy in the reduction of phantom limb pain in unilateral below-knee amputees. J Neurosci Rural Pract. 2024;15:552-6. doi: 10.25259/JNRP_70_2024
Abstract
Objectives:
Phantom limb pain (PLP) is a common issue for amputees, leading to various long-term challenges. Mirror therapy, a low-risk and cost-effective treatment, can be done at home. This study evaluates the effect of home-based mirror therapy on PLP in unilateral below-knee amputees.
Materials and Methods:
The study included 16 male participants, aged 18 and above. They were randomly assigned to either the mirror therapy group or the control group (prosthesis use). The mirror therapy group received a single training session (15–30 min). Then, they did exercises at home for at least 15 min a day for four weeks. They also had to use their prosthesis for at least 3 h daily. Weekly phone or online check-ins recorded pain levels. Pain was measured using the Visual Analog Scale (VAS).
Results:
Participants had a mean age of 45.12 years, and initial VAS pain scores ranged from 3 to 10. After 4 weeks, the mirror therapy group showed a 37.5% reduction in pain (P < 0.05). The control group did not experience a significant pain change (P > 0.05).
Conclusion:
Mirror therapy is a promising option for managing PLP. It supports the benefits of telehealth and home-based exercises, reducing the need for in-person consultations.
Keywords
Phantom limb pain
Mirror therapy
Below-knee amputation
Prosthesis
INTRODUCTION
Phantom limb pain (PLP) is characterized by painful sensations in an amputated limb.[1-3] It significantly impacts the quality of life among amputees.[4] PLP syndrome affects 80% of individuals who have undergone limb amputation.[5] The causes of this syndrome are influenced by physiological, environmental, and psychological factors.[3,6-8] The experience of PLP varies among individuals, ranging from short-term discomfort to persistent pain. This pain can manifest as muscle cramping, burning, or shooting pain.[9]
The pathophysiology of PLP is not fully understood. However, it is believed that both the peripheral and central nervous systems play a significant role in its development. One hypothesis suggests that changes in the brain’s cortical map following amputation contribute to the syndrome.[2,8,10]
At present, there are various treatments for PLP, but their effects are often unpredictable. These treatments include medications, psychological, acupuncture, transcutaneous electrical nerve stimulation, hypnosis, and mirror therapy.[2,3,6] There is a need to develop a non-invasive treatment that does not require surgery or drugs with potential side effects.
Ramachandran pioneered a simple, cost-effective approach to treat this syndrome, known as mirror therapy. The therapy stemmed from a theory of “learned paralysis.”[11] According to this postulate, after amputation, the brain still transmits efferent motor commands to the limb.[11] In mirror therapy, a mirror is placed between the patient’s sound limb and their amputated limb. The patient executes a series of movements with the intact limb while trying to mimic the same movements with the amputated limb. This generates an illusion for the patient, making them perceive the presence of the missing limb.[7-9,12,13]
This treatment does not require specific procedures or additional medications and can be done wherever a mirror is available. The emphasis on reducing clinic visits has grown due to the COVID-19 pandemic.[14] With telehealth, individuals can manage or eliminate their PLP independently, making this treatment accessible and cost-effective.
The aims of this study are:
Is a home-based program of mirror therapy and prosthesis wearing more effective in reducing PLP compared to prosthesis wearing alone?
Is a home-based telehealth mirror therapy program feasible?
MATERIALS AND METHODS
This is an interventional study. Approval was obtained from the Research and Ethics Committees of Isfahan University of Medical Sciences. Criteria included unilateral below-knee amputation, age over 18, pain score higher than 3, no prior mirror therapy, and use of a PTB prosthesis.
Exclusion criteria included severe stump infections, soft tissue deformities, psychological problems, vision problems, and the use of painkillers, sleeping pills, or antidepressants. Data were analyzed from two independent cohorts with unilateral lower-limb amputation. A questionnaire collected demographic data such as sex, age, height, weight, body mass index (BMI), side of amputation, time since amputation, occupation, and prosthesis use duration.
Most participants were from the Iranian Red Crescent Society in Tehran, chosen for its high patient influx. Participants were informed of the treatment’s lack of known side effects and agreed to participate after completing the consent form.
Participants received a 15–30-min in-person session to learn safe mirror use [Figure 1]. Once confirmed, they could perform the exercises independently and commit to daily practice for 4 weeks.

- Mirror exercise technique.
Daily exercises included foot rotation from heel to toe, forefoot rotation, finger bending and straightening, foot tapping, and writing numbers in the air with the foot. Based on power analysis using G*Power software (version 3.1.9.7, Dusseldorf, Germany) and assuming the mean value and standard deviation from the study by M. Yildirim and N. Kanan (26), the sample size was calculated. With a significance level of 0.05, statistical power of 0.8(β-1), and an allocation ratio of 1:1, the sample size for each group was 8.
This study enrolled 16 male patients aged 18 and above with unilateral below-knee amputation at least a year prior. They wear prosthesis for a minimum of 3 h daily. Eligible participants had never undergone mirror therapy and had a pain score of at least 3 on the visual analog scale (VAS).[15]
The Shapiro–Wilk test and normality plots examined the distribution of continuous variables. Normally distributed variables were expressed as mean and standard deviation. Paired t-tests compared the groups. Pearson’s test analyzed the relationship between times since amputation, hours of prosthesis use, and pain reduction. The significance level for all tests was set at 0.05. Statistical analysis was conducted using the Statistical Package for the Social Sciences 22 software.
RESULTS
The mean age was 45.12 years (standard deviation [SD] = 8.7), and the mean BMI was 26.7 (SD = 4.62). All patients experienced PLP at least once a week. Before the study, the mirror therapy group’s VAS pain scores were two participants with moderate pain and six with severe pain. After the intervention, three participants experienced mild pain, two had moderate pain, and three continued to have severe pain.
The average pain score in the mirror therapy group decreased from 7.25 (SD = 2.12) to 4.62 (SD = 1.92) (P < 0.05). No significant decrease in pain was observed in the control group, with pain scores changing from 5.7 (SD = 2.31) to 4.6 (SD = 2.19) (P > 0.05).
The changes in perceived pain in both groups are shown in Figures 2 and 3. The intervention group reported lower pain levels after four weeks, while pain levels in the control group remained largely unchanged.
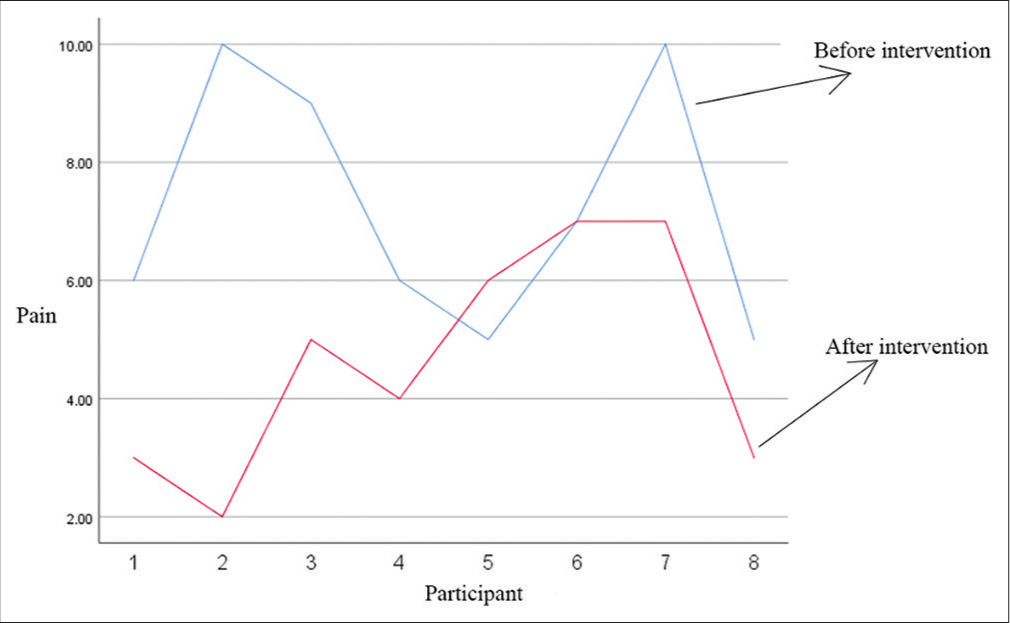
- Pain before and after a 4-week period in the mirror group.
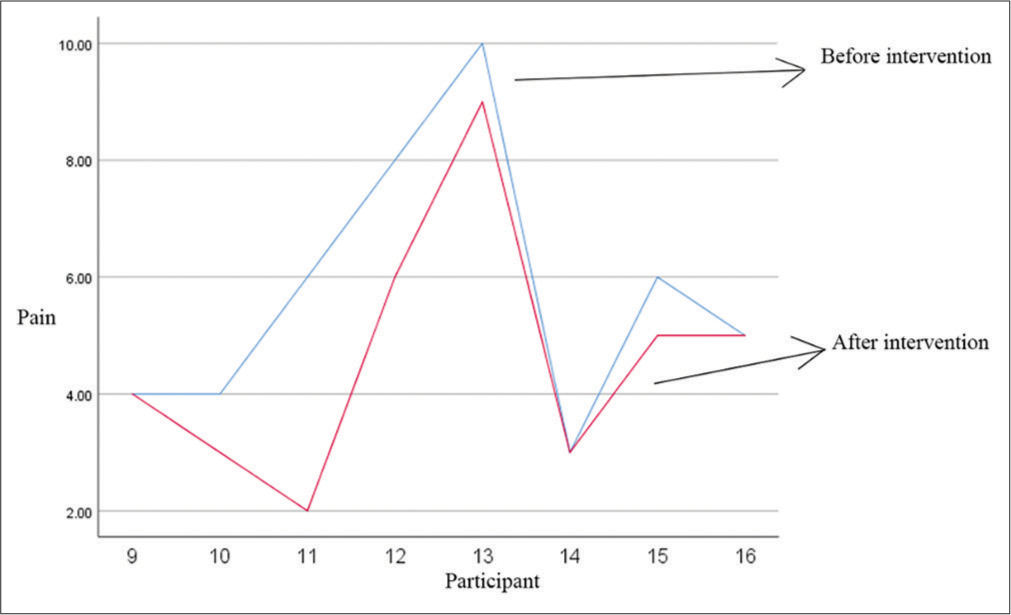
- Pain before and after a 4-week period in the control group.
The mirror therapy group showed a significant reduction in pain intensity (P = 0.029). The control group did not show a significant reduction (P = 0.051). Statistical analysis indicated that one month of mirror therapy significantly reduced perceived pain (P = 0.029). The control group did not experience a significant decrease in perceived pain (P = 0.051) [Table 1]. The perceived pain did not significantly decrease for the control group (P = 0.051). When comparing perceived pain before and after mirror therapy in pairs, the mean was 2.62.
| Group | Before (mean±SD) | After (mean±SD) | P-value within groups | P-value between groups |
|---|---|---|---|---|
| Mirror therapy | 7.25±2.12 | 4.62±1.92 | 0.029 | 0.038 |
| Control | 5.75±2.31 | 4.62±2.19 | 0.051 |
SD: Standard deviation.
There was a moderate positive correlation (0.464) between the time since amputation and pain reduction. However, this correlation was not statistically significant (P = 0.070). This correlation suggests that pain generally decreases with more time post-amputation.
The relationship between the duration of prosthesis use and pain reduction was also measured. The data showed a moderate negative correlation (r = −0.330) between these variables, which was not statistically significant (P = 0.212). This suggests that longer prosthesis use is not associated with greater pain reduction.
DISCUSSION
Mirror therapy has emerged as a promising approach for treating PLP over the past two decades. It is a non-surgical method that requires no hospitalization and lacks the side effects typically associated with medications. Moreover, it enables patients to manage their PLP independently at home without frequent therapist visits.
Our findings show that mirror therapy was more effective in reducing PLP compared to prosthesis use alone. Mirror therapy was particularly useful for patients with severe PLP. This feasibility study indicates that a telehealth home-based mirror therapy program was effective in reducing PLP.
This study showed a 37.5% reduction in pain using VAS. These findings align with those of Foell et al., who reported a 27% decrease in pain in a similar four-week study involving 13 participants.[16] This alignment is also observed in other studies.[17-20] However, it contradicts the study by Brodie et al., which found no significant difference in pain reduction between mirror exercises and control groups. Their study only conducted a single exercise session.[19,21-26] Darnall noted that PLP returned within one or two days after stopping mirror therapy, despite daily 20-min exercises. No significant correlation was found between the success of mirror therapy and exercise duration or frequency. Consistent daily exercise is key, but increasing frequency or duration did not significantly impact success.[13]
Yildirim and Kanan explored the effects of a four-week mirror therapy program on 15 individuals with upper or lower-limb amputations. They found the treatment more effective for non-prosthetic users.[26] Our study compared the effect of using a prosthesis alone versus combining mirror therapy with a prosthesis. We found that combining mirror therapy with a prosthesis significantly reduced PLP for most participants.
Folch et al.’s case study on a 53-year-old woman with a left leg amputation showed a 48% decrease in average pain intensity over two years.[19] In our study, despite the one-month duration, we observed a 37.5% decrease in PLP.
Telehealth, conducted through email, messaging applications, and forums, is a strength of this home-based mirror therapy program. Telehealth encourages individuals to engage in and maintain their exercises, potentially leading to more reliable results than in-person visits due to increased motivation.
Participants who reported weekly pain reductions had a positive perception of mirror therapy. They attribute their improved mental states to physical activity and pain reduction. The combination of in-person and online exercises contributed to participant satisfaction. Online follow-ups help identify psychological and physical issues early, allowing intervention to prevent disruption in pain reduction and increasing the likelihood of successful treatment.
This study focused only on below-the-knee amputations. Although there was no significant change in prosthesis use, home and remote treatment methods represent an innovative approach to managing PLP and are acceptable to patients.
Given the clinically significant 37.5% average pain reduction in the mirror therapy group, we recommend future studies with larger sample sizes and extended follow-up periods. One limitation of this study was that it only included male amputees. Individuals with amputations due to vascular diseases were not investigated.
CONCLUSION
Mirror therapy is a viable method for reducing PLP, aiding individuals in managing their discomfort. It was particularly useful for patients with severe PLP. This method is easily adaptable for home use, and telehealth can help maintain consistency in exercises, enhancing efficacy.
Acknowledgments
We thank the research assistant of Isfahan University of Medical Sciences for funding this research project.
Ethical approval
Ethics Committee of Isfahan University of Medical Sciences issued permission to conduct this study, using registration number IR.MUI.RESEARCH.REC.1400.264.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Self-reported treatments used for lower-limb phantom limb pain pain: Descriptive findings. Arch Phys Med Rehabil. 2006;87:270-7.
- [CrossRef] [Google Scholar]
- Maladaptive plasticity, memory for pain and phantom limb pain: Review and suggestions for new therapies. Expert Rev Neurother. 2008;8:809-18.
- [CrossRef] [Google Scholar]
- Phantom limb pain limb related phenomena and their rehabilitation after lower limb amputation. Eur J Phys Rehabil Med. 2009;45:559-66.
- [Google Scholar]
- Motor control over the phantom limb pain limb in above-elbow amputees and its relationship with phantom limb pain. Neuroscience. 2009;162:78-86.
- [CrossRef] [Google Scholar]
- Wall and Melzack's textbook of pain e-dition London, United Kingdom: Churchill Livingstone, (Elsevier Health Sciences); 2005.
- [Google Scholar]
- Exploratory findings with virtual reality for phantom limb pain; from stump motion to agency and analgesia. Disabil Rehabil. 2009;31:846-54.
- [CrossRef] [Google Scholar]
- The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain. 2009;132:1693-710.
- [CrossRef] [Google Scholar]
- Mirrored, imagined and executed movements differentially activate sensorimotor cortex in amputees with and without phantom limb pain. Pain®. 2010;149:296-304.
- [CrossRef] [Google Scholar]
- Mirror visual feedback therapy. A practical approach. J Hand Ther. 2011;24:170-9.
- [CrossRef] [Google Scholar]
- Synaesthesia in phantom limb pain limbs induced with mirrors. Proc R Soc Lond Ser B Biol Sci. 1996;263:377-86.
- [CrossRef] [Google Scholar]
- Self-delivered home-based mirror therapy for lower limb phantom limb pain. Am J Phys Med Rehabil. 2009;88:78-81.
- [CrossRef] [Google Scholar]
- The war on COVID-19 pandemic: Role of rehabilitation professionals and hospitals. Am J Phys Med Rehabil. 2020;99:571-2.
- [CrossRef] [Google Scholar]
- Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153-7.
- [CrossRef] [Google Scholar]
- Mirror therapy for phantom limb pain: Brain changes and the role of body representation. Eur J Pain. 2014;18:729-39.
- [CrossRef] [Google Scholar]
- Mirror therapy and transcutaneous electrical nerve stimulation for management of phantom limb pain in amputees-a single blinded randomized controlled trial. Physiother Res Int. 2016;21:109-15.
- [CrossRef] [Google Scholar]
- Treating phantom limb pain following amputation: The potential role of a traditional and teletreatment approach to mirror therapy Netherlands: Zuyd Hogeschool; 2019.
- [Google Scholar]
- Mirror therapy for phantom limb pain in moderate intellectual disability. A case report. Eur J Pain. 2022;26:246-54.
- [CrossRef] [Google Scholar]
- Home-based mirror therapy with individual set of exercises improves phantom limb pain and limb sensation of lower extremity amputees. Biomed J Sci Tech Res. 2021;37:226-31.
- [CrossRef] [Google Scholar]
- Analgesia through the looking-glass? A randomized controlled trial investigating the effect of viewing a 'virtual'limb upon phantom limb pain, sensation and movement. Eur J Pain. 2007;11:428-36.
- [CrossRef] [Google Scholar]
- The use of mirror therapy in the treatment of phantom limb pain in amputees. World J Adv Res Rev. 2021;10:214-9.
- [CrossRef] [Google Scholar]
- Mirror therapy in the management of phantom limb pain. AJN Am J Nurs. 2020;120:41-6.
- [CrossRef] [Google Scholar]
- A randomized, controlled trial of mirror therapy for upper extremity phantom limb pain in male amputees. Front Neurol. 2017;8:267.
- [CrossRef] [Google Scholar]
- Intervention for phantom limb pain: A randomized single crossover study of mirror therapy. Indian J Psychiatry. 2017;59:457-64.
- [Google Scholar]
- The effect of mirror therapy on the management of phantom limb pain. Agri. 2016;28:127-34.
- [CrossRef] [Google Scholar]






