Translate this page into:
The Conundrum of Ventricular Dilatations Following Decompressive Craniectomy: Is Ventriculoperitoneal Shunt, The Only Panacea?
Address for correspondence: Dr. Sunilkumar Balakrishnan Sreemathyamma, Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India. E-mail: sunilkumarbs2017@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Ventriculomegaly and hydrocephalus (HCP) are sometimes a bewildering sequela of decompressive craniectomy (DC). The distinguishing criteria between both are less well defined. Majority of the studies quoted in the literature have defined HCP radiologically, rather than considering the clinical status of the patient. Accordingly, these patients have been treated with permanent cerebrospinal fluid (CSF) diversion procedures. We hypothesize that asymptomatic ventriculomegaly following DC should undergo aspiration with cranioplasty and be followed up regularly.
Materials and Methods:
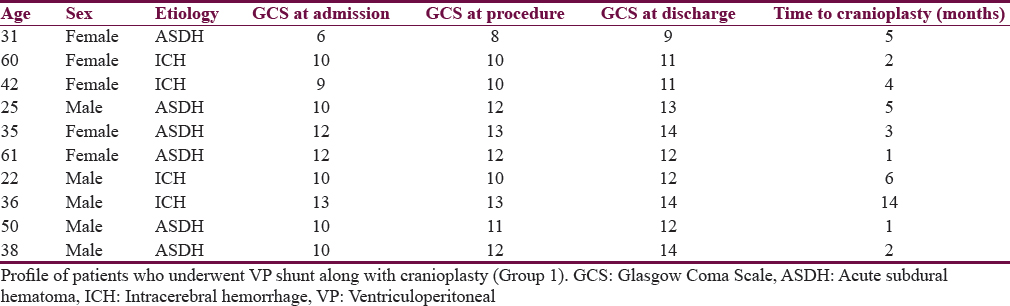
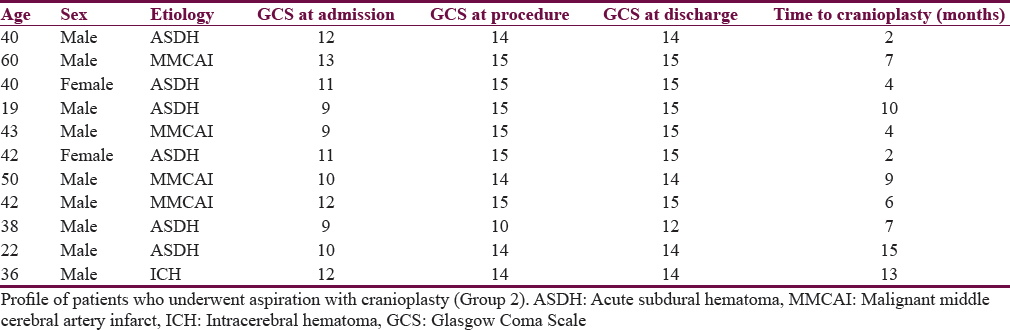
All patients with post-DC who were scheduled for cranioplasty and satisfied the radiological criteria for HCP were included. These patients were categorized into two groups. Group 1 included ventriculomegaly with clinical signs attributable to HCP and Group 2 constituted ventriculomegaly but no clinical signs attributable to HCP. All patients in Group 1 underwent ventriculoperitoneal shunt followed by cranioplasty, whereas all patients in Group 2 underwent cranioplasty along with simultaneous ventriculostomy and temporary aspiration of the lateral ventricle. All patients were regularly followed as the outpatient basis.
Results:
There were 21 patients who developed ventriculomegaly following DC. There were 10 patients in Group 1 and 11 patients in Group 2. The average duration of follow-up was from 6 months to 2 years. Two patients in the shunt group - (group 1) had over drainage and required revision. One patient in aspiration group - (group 2) required permanent CSF diversion.
Conclusions:
Cranioplasty with aspiration is a viable option in selected group of patients in whom there is ventriculomegaly but no signs or symptoms attributable to HCP.
Keywords
Decompressive craniectomy
hydrocephalus
ventriculoperitoneal shunt
ventriculostomy
INTRODUCTION
The occurrence of ventriculomegaly/hydrocephalus (HCP) following decompressive craniectomy (DC) estimates a wide range around 10%–45%.[1234] These figures vary widely because of the different criteria chosen for the determination of HCP following DC. Most studies have set radiological parameters to determine the onset of HCP following DC.[15] However, this alone along with clinical manifestations of HCP should determine the course of treatment. We, in our institution, have followed a treatment protocol for management of patients who have post-DC HCP (PDCH)/post-DC ventriculomegaly (PDCV). Patients who had ventricular enlargement and clinical manifestations of HCP, viz., poor MMSE, gait disturbances, and papilledema, underwent ventriculoperitoneal shunt (VPS), while others who did not have symptoms and papilledema but had ventriculomegaly underwent a ventricular puncture and aspiration of the lateral ventricle at the time of cranioplasty. By this ventriculostomy, the brain shrunk back into the confines of the cranial defect and facilitated to anchor the bone flap accurately in the cranial defect.
MATERIALS AND METHODS
All patients who developed brain swelling and radiologically confirmed ventricular dilatation following DC were included in the study. The study was done after obtaining clearance from the Institutional Review Board and the Ethics Committee. The study was a prospective observational study conducted in accordance with the Ethical Standards on Human Experimentation of the Helsinki Declaration of 1975, as revised in 2000. Evan's index >30% was used as the limit to define HCP. The patients were divided into two groups. Patients who had clinical signs of HCP and papilledema were assigned Group 1 and patients who did not have clinical signs of HCP and papilledema constituted Group 2. Patients in Group 1 underwent cranioplasty with VPS either as a staged or concurrent procedure, whereas patient in Group 2 underwent simple aspiration of ventricles followed by cranioplasty. The mean follow-up period was 6 months to 2 years. All patients were examined for development of papilledema and signs of neurological deterioration. All patients underwent DC in a uniform manner as follows.
Decompressive hemicraniectomy
A typical surgery performed in our institution is by marking a large bone flap covering the frontal, parietal, temporal, and occipital region. We usually keep our medial margin 2.5 cm away from the midline. The dural is opened in a stellate fashion and the etiology, i.e., hematoma/contusion is let out. After attaining the hemostasis, the brain is usually covered with a double layer of dural substitute, G-Patch (G. Surgiwear Ltd.). A drain is kept and wound is closed in two layers. The bone flap is usually kept in the left upper quadrant in the abdomen.
Ventriculoperitoneal shunt and cranioplasty
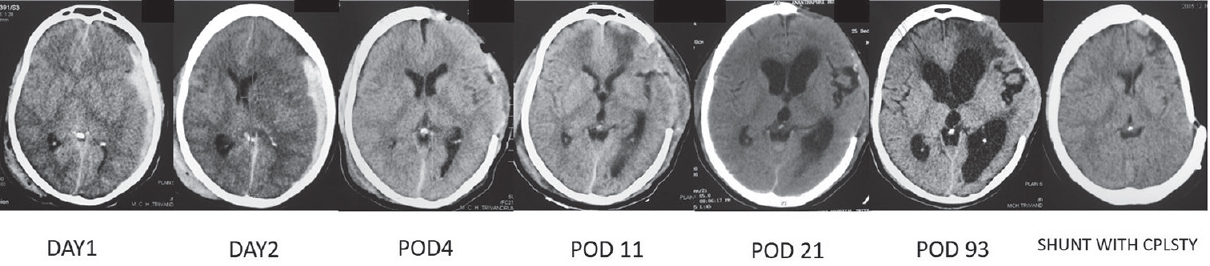
VPS and cranioplasty was done as a staged procedure in eight patients and concurrently in two patients. The site usually chosen for the shunt insertion was ipsilateral to the side of craniectomy in patients who underwent shunt concurrently and contralateral to craniectomy site when done as a staged procedure. A burr hole was made just behind posterior-most edge of the craniectomy when done concurrently, whereas the site of entry in staged procedure was keen's point. The ventricular catheter was guided into the occipital horn of the lateral ventricle and advanced further to reach the frontal horns. The medium pressure Chhabra VPS shunt was the most commonly chosen shunt for the procedure. The abdomen incision was put over the lumbar or hypochondrium region depending on the surgeon's preference and subcutaneous tunneling was done, and the procedure was completed as with the standard VPS. Timeline of events on a computed tomography (CT) scan of a patient undergoing the procedure is illustrated in Figure 1. The clinical profile, etiology, and Glasgow coma scale GCS at presentation, during the procedure, and at discharge are summarized in Table 1.
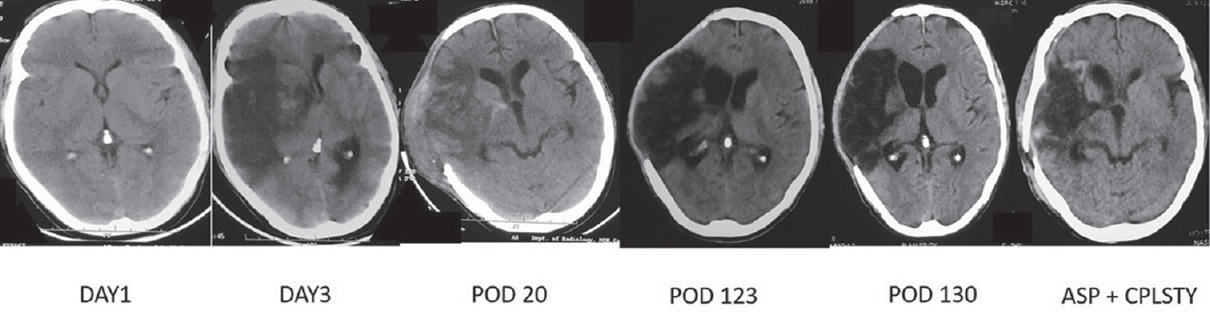
- Timeline of events on a computed tomography scan of a typical patient who developed ventriculomegaly following a malignant middle cerebral artery infarct and underwent aspiration with cranioplasty. POD: Postoperative day, Asp + Cplsty: Aspiration with cranioplasty
Aspiration and cranioplasty
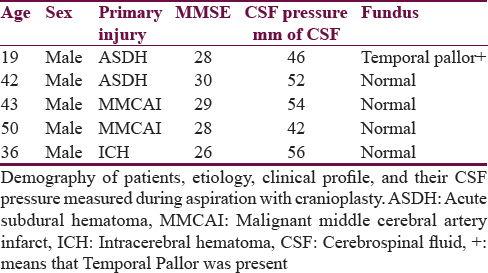
A typical procedure is illustrated in Figure 2. The patient is supine with head turned to the side opposite to the craniectomy. The bone flap is harvested first and the abdominal wound is closed by the assistant. The cranial would is opened in the line of the previous incision under sterile precautions. The skin flap is raised and the bony edges are defined. The Paine's point was usually chosen as the entry site for ventricular catheterization but was left to the discretion of a surgeon. A ventricular end of a VPS catheter is inserted into the ventricle and the cerebrospinal fluid (CSF) is aspirated until the brain becomes lax. In the latter part of the study, we started to measure the intracranial pressure (ICP) to rule out high-pressure HCP. When adequately lax and the bone flap fits in snuggly to the defect, it is anchored to the craniectomy site with plate and screws. At the end of the procedure, the ventricular catheter is removed. There were cases where the neuro-ophthalmic findings were equivocal. In such patients, ICP was measured to rule out high-pressure HCP. Timeline of events in CT scan of a patient undergoing the procedure is illustrated in Figure 3. The clinical profile, etiology, and GCS at presentation, during the procedure, and at discharge are summarised in Table 2.
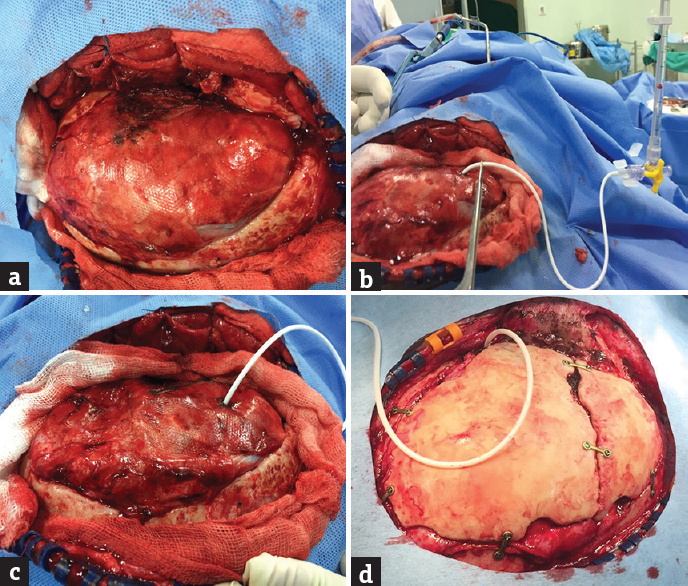
- Intraoperative images of a patient with acute subdural hematoma and coronal sutural diastasis 3 months after decompressive craniectomy. Patient is undergoing aspiration with cranioplasty. (a) The mildly tense brain is visualized after raising of skin flap. (b) Intracranial pressure being measured after cannulation ventricles at the Paine's point. (c) The brain becoming very lax after sufficient amount of cerebrospinal fluid is let off. (d) The bone pieces being anchored at the craniectomy site with plate and screws
- Timeline of events on a computed tomography scan of a typical patient who developed ventriculomegaly following acute subdural hematoma and underwent Ventriculoperitoneal shunt. POD: Postoperative day, Cplsty: Cranioplasty
RESULTS
Two hundred and ten patients underwent decompressive craniotomies between 2014 and 2016. Majority of the patients comprised of traumatic brain injury, middle cerebral artery infarct, and intracerebral hematoma. Twenty-six patients died and were excluded from this study. Of the remaining 174 patients who were followed up and scheduled for cranioplasty, 21 (12.07%) patients developed ventricular dilatations. There were 14 males and 7 females in the study. There were 12 cases of acute subdural hematoma, 4 cases of malignant middle cerebral artery infarct, and 5 cases of intracerebral hematoma. The mean age of the patients was 37.1 ± 13.4 years. The mean Evan's index in the shunt group (38.58 ± 1.69) was higher than in the aspiration group (33.75 ± 1.46), and this difference was found to be statistically significant. Figure 4 illustrates the boxplot for Evan's index in the two groups.
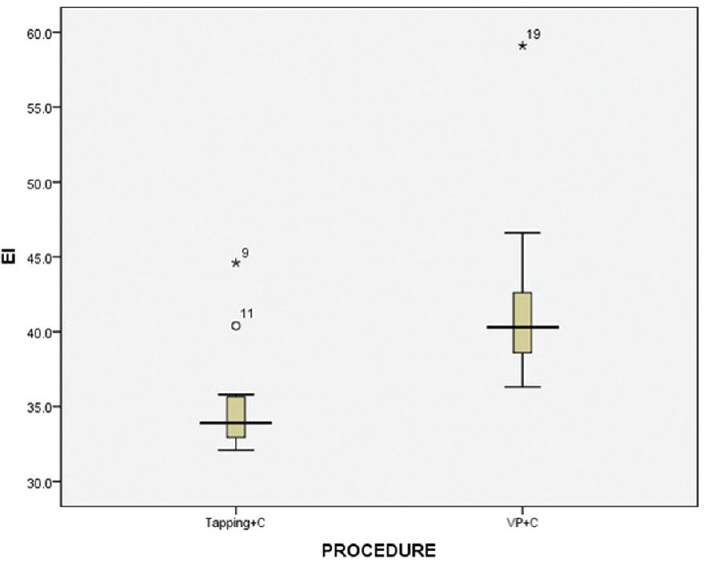
- Boxplot showing Evan's index for the two groups. The median Evan's index was higher in the shunt group than the aspiration group
Ten patients with ventriculomegaly had poor GCS and had papilledema. These patients underwent a VPS followed by cranioplasty. The rest of the 11 patients underwent aspiration of lateral ventricles along with cranioplasty. ICP was measured in five patients in Group 2 [Table 3]. The mean ICP was 50 mm of CSF. The average duration of time elapsed between cranioplasty and initial injury was not uniform due to poor follow-up in the initial period. The mean time to cranioplasty was 4.2 months in the shunt group and 7.1 months in the aspiration group. The boxplot for time to cranioplasty in the aspiration group and the shunt group is shown in Figure 5. The aspiration group had higher GCS than the shunt group.
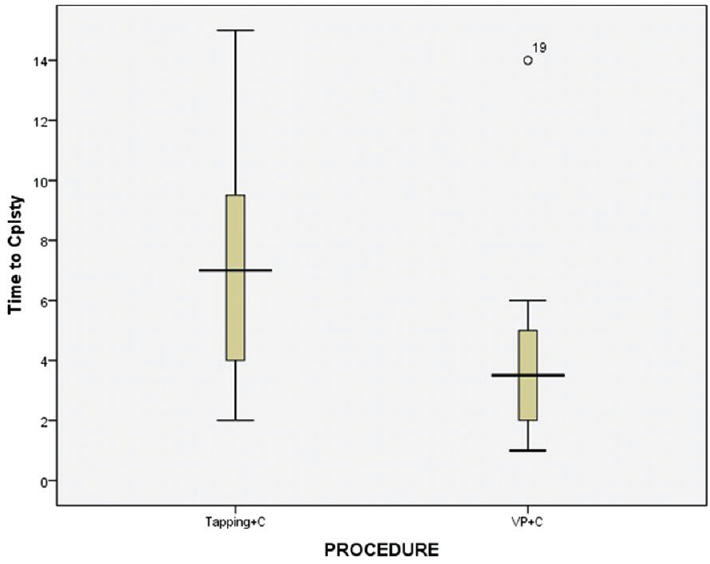
- Boxplot showing time to cranioplasty between two groups. The median time to cranioplasty in the shunt group was much earlier than the aspiration group
Complications
There were no procedure-related complications in the VPS group. One patient in the aspiration group had complication wherein his brain became suddenly tense while doing the ventricular puncture at the keens point. Anticipating an intracranial bleed, an external ventricular drain (EVD) was inserted at the Paine's point while the procedure was abandoned. Emergency CT scan was done which revealed an intracerebral hematoma at the initial puncture site [Figure 6]. He was ventilated without evacuating the hematoma, and he was back to his preoperative status after 48 h after which the EVD was removed. This patient was not willing for any further procedures while he is still in follow-up with good neurological status.
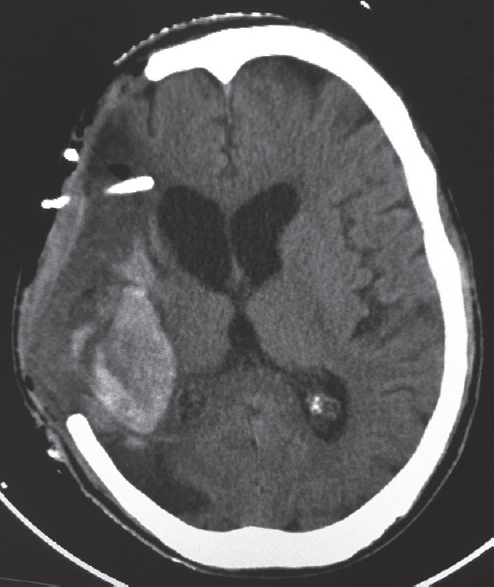
- Computed tomography brain plain showing intracerebral hematoma along the tract on the posterior parietal region. The external ventricular drain has been pulled out in transit to the computed tomography scan which was reinserted later
Follow-up
All patients in both groups recovered well, and they were discharged with regular follow-up on outpatient basis. The improvement in was more pronounced in the aspiration group compared to the VPS group. The mean duration of follow-up period of patients in both groups was 22 months. One patient in the shunt group died due to causes unrelated to the procedure. Two patients in the shunt group developed over drainage of the ventricle, and consequently, their VPS was tied off. These two patients underwent a programmable shunt at a later stage.
One patient in the aspiration group developed mild aphasia and headache at a follow-up of 12 months. This patient had mild increase in ventricular size with regard to previous CT findings and fundus showed evidence of papilledema; hence, he underwent VPS. The patient improved symptomatically after the CSF diversion.
DISCUSSION
DC has become cornerstone in the management of intractable raised intracranial hypertension, particularly in places where there are no ICP monitors available. Mostly reserved for trauma-related causes, the indications for DC have been broadened to include a variety of etiologies such as spontaneous intracerebral hematoma, cerebral venous sinus thrombosis, malignant middle cerebral artery infarct, and subarachnoid hemorrhage.[26789] The growing acceptance of this technique for various etiologies began to expose the different complications associated with it. PDCH is one peculiar complication associated with this technique. The popular postulations cited as to the cause of this etiology are disturbances in the pulse wave pressure across the convexity of the brain following DC[10] as well as decreased venous outflow at the medial margin of the craniectomy.[14] Studies also describe the size of the craniectomy to be an inciting factor in the development of HCP.[41112]
The incidence of PDCH in the literature varies between 0.7% and 86%.[11] This wide range is most likely due to the difference in criteria adopted for defining HCP in various studies. Conventionally, this has to be associated with clinical manifestations of HCP. Since these signs and symptoms are difficult to be elicited in the background of clinical decline following trauma, many authors have defined this only by the size of ventricles on CT scan.[113] Consequently, there has been exponential increase in reporting this entity.[11] In this study, Evan's index of >30% was chosen as the criteria for ventriculomegaly. In our series, the incidence of HCP was 10%. This was in spite of the margins of craniectomy being 2.5 cm away from the midline. This controllable etiology has been postulated to be an important inciting factor for the development of PDCH.[14] On the contrary, there are studies refuting these hypotheses.[31415] The primary indication for DC in our patients was mainly stroke, intracerebral hematoma, and acute subdural hematoma. Interestingly, none of our patients who underwent DC for malignant middle cerebral artery infarct developed a shunt-dependant HCP. The finding whether DC for stroke causes shunt-dependant HCP is a matter of dispute. Rahme et al. noted 0% shunting rates in their cohort of 12 patients who underwent DC for middle cerebral artery infarction.[16] Various other authors who have contradicted this finding by reporting the incidence of HCP following DC for middle cerebral artery infarct in the range of 29%[17]–71%.[10] As the total number of patients who undergo DC for traumatic brain injury in our center fairly outnumbers patients who undergo DC for stroke, nothing conclusively can be derived from our finding.
Owing to the higher incidence of complications following a DC, researchers have investigated and found that by doing a cisternostomy and replacing the bone flap back after craniotomy, the incidence of HCP has decreased.[1819] In this method, the authors have described wide opening of the basal cisterns of the brain, whereby adequate CSF is drained until optimal brain relaxation is achieved. This facilitates the replacement of bone flap easily contrary to conventional decompressive hemicraniectomy where this is not possible.
We have noted that there are a subset of patients who have post DC ventriculomegaly and aslo satify the radiological criteria for hydrocephalus but are clinically asymptomatic. Hence, we believe that in such, subgroup of a permanent CSF diversion is unnecessary. It would be wiser to call it PDCV. Authors have estimated that such ventriculomegaly to be very common and around 45%, but only a third of this require any form of CSF diversion.[3] Lin et al. in their study noted ventriculomegaly in all their 13 patients who underwent a DC for malignant middle cerebral artery infarct.[20] They noted that the neurologic findings were disproportionate to the degree of ventriculomegaly in their patients. However, a mildly bulging brain will hinder the proper placement of bone flap back into the craniotomy defect during cranioplasty. To circumvent this, we do a ventriculostomy at defined entry points till the brain regresses back into the confines of the cranial vault. This will facilitate the placement of bone flap to be accurately placed into the craniotomy defect. Having said this, we do acknowledge the presence of patients who have PDCH and are symptomatic. Such patients tend to have tense brain bulging outside the confines of the skull defect with associated papilledema. They need a permanent CSF diversion procedure. We generally do this at the time of cranioplasty or as a staged procedure. We had only one complication during cannulation of the ventricle in the aspiration group with the development of intraparenchymal hematoma. Since it was on the side of the gliotic brain, we did not anticipate any further deficits. An immediate insertion of EVD into the Paine's point negated the temporary rise of ICP. Some authors have advocated the use of external lumbar drains for post-DC brain swellings. Although not widely reported, this technique is a valid alternative to EVDs.[2122]
Alternatively, Yang and Pirouzmand have described an innovative method to mitigate the effect of brain bulges due to underlying psuedomeningoceles following DC.[23] In this method, they have described controlled reduction duroplasty with radial coagulation of dura, akin to spokes of wheel pattern using a bipolar cautery under low current. This has effectively lessened the protrusion caused by underlying psuedomeningoceles by shrinking of the overlying dura aiding in the bone flap replacement into the desired craniectomy defect. We had tried this method in the above patient in whom the complication of intracerebral hematoma occurred before the aspiration technique, but the reduction achieved was not sufficient to anchor the bone flap successfully.
Postcraniotomy bulges have been classified by different authors.[122425] According to them when the brain is tense and herniating outside, the skull needs cranioplasty with permanent CSF diversion. In cases where the brain is flaccid and not tense, a cranioplasty may be sufficient. None of our patients in Group 2 had tense bulging brain.
The disappearance of ventriculomegaly after cranioplasty is well documented.[262728] This has been shown in various case series of patients who were waiting to undergo staged operation for cranioplasty and VPS. The return of the CSF and hemodynamic within the brain after the placement of the bone flap may play a role in the resolution of HCP.[2930] Pachatouridis et al. from Greece studied the patients with PDCH with VPS as a single as well as staged procedure along with cranioplasty.[28] The single-staged surgery was accomplished with programmable shunt while staged surgery included insertion of ventricular catheter and measurement of ICP and choosing the most appropriate shunt according to the pressure. In that study, the author describes three patients, one from concomitant group and two from staged group who did not eventually require a VPS for HCP following cranioplasty. In their respective studies of PDCH following DC for middle cerebral artery infarction, Lee et al.[17] and Lin et al.[20] reported two out of seven and nine out of thirteen patients who did not require a VPS.
In another series by Tsang et al., the authors reported that five out of 21 patients who had undergone cranioplasty with VPS in situ were eventually found to be nonshunt dependent after their shunts were exteriorized for malfunction.[31] In these patients, CSF dynamics might have returned to normal following cranioplasty, leading them to live a shunt independent life.[31]
Patients who had such resolution of HCP also need to be followed up as it has been documented in the literature that HCP can develop even as a late sequelae following head injury.[32] An ophthalmologic follow-up to look for papilledema is a good test to screen patients for the evidence of developing HCP. This has been validated in the literature in patients who have undergone DC.[33] All our patients in Group 2 were screened for development of papilledema in the follow-up period, but this occurred only in one patient. As he also developed mild aphasia, the possibility of late high-pressure HCP was thought of, and he underwent VPS. Insertion of VPS in not without complications which are well described in the literature.[343536] By doing aspiration along with cranioplasty, we could avoid a VPS in 10 out of 11 patients.
Two patients in the shunt group had over drainage of the CSF and required a revision with programmable shunt. The incidence of over drainage and subdural collections has been reported to be more in patients undergoing VPS for PDCH.[20] This happened around 3 months in one patient and in the 5th month in the second patient. The use of programmable shunts has been very effectively proven for the PDCH in various case series.[25283738] The feasibility to titrate the pressure of the programmable valve is prominent advantage over fixed pressure valve in this situation as the blood and CSF dynamic may take time to return to normal following cranioplasty. Since this study was done in a tertiary care government hospital, the socioeconomic status of the patients is not well developed to afford a programmable shunt.
Limitations of the study
Only ten patients underwent aspiration and cranioplasty in Group 2. This cohort sample was too small to derive a definitive conclusion. ICPs were not measured in all cases to select the appropriate pressure for fixed pressure shunt. Marmarou et al.[39] studied the CSF dynamics in posttraumatic patients and showed that the mere presence of ventriculomegaly does not indicate high-pressure HCP. It can also occur in cases of atrophy and normal pressure HCP. In our study, we did not measure ICP in all cases, and hence, this might have led to failure to identify cases of normal pressure HCP which can occur in cases of trauma.
CONCLUSIONS
Not all cases of PDCH warrant permanent CSF diversion surgery such as VPS. The strategy of aspiration with cranioplasty is a valid option in the management of PDCV. By the described procedure, a permanent VPS may be avoided in a selected group of patients with craniectomy-related HCP who undergo cranioplasty. However, these patients need to be followed up to detect the possibility of development of late HCP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Post-traumatic hydrocephalus after decompressive craniectomy: An underestimated risk factor. J Neurotrauma. 2010;27:1965-70.
- [Google Scholar]
- Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364:1493-502.
- [Google Scholar]
- Incidence and risk factors for post-traumatic hydrocephalus following decompressive craniectomy for intractable intracranial hypertension and evacuation of mass lesions. J Neurotrauma. 2012;29:1872-8.
- [Google Scholar]
- Hydrocephalus after decompressive craniectomy for hemispheric cerebral infarction. J Clin Neurosci. 2013;20:377-82.
- [Google Scholar]
- Factors associated with shunt-dependent hydrocephalus after decompressive craniectomy for traumatic brain injury? J Neurosurg. 2017;16:1-6. doi: 10.3171/2017.1.JNS162721. [Epub ahead of print]
- [Google Scholar]
- Ventriculomegaly after decompressive craniectomy with hematoma evacuation for large hemispheric hypertensive intracerebral hemorrhage. Clin Neurol Neurosurg. 2013;115:317-22.
- [Google Scholar]
- Decompressive craniectomy in hemorrhagic cerebral venous thrombosis: Clinicoradiological features and risk factors. J Neurosurg. 2017;127:709-15.
- [Google Scholar]
- Time is brain! Analysis of 245 cases with decompressive craniectomy due to subarachnoid hemorrhage. World Neurosurg. 2017;98:689-94.e2.
- [Google Scholar]
- Outcome after decompressive craniectomy in different pathologies. World Neurosurg. 2016;93:389-97.
- [Google Scholar]
- Postoperative hydrocephalus in patients undergoing decompressive hemicraniectomy for ischemic or hemorrhagic stroke. Neurosurgery. 2007;61:489-93.
- [Google Scholar]
- Clinical factors for the development of posttraumatic hydrocephalus after decompressive craniectomy. J Korean Neurosurg Soc. 2008;43:227-31.
- [Google Scholar]
- Posttraumatic hydrocephalus associated with decompressive cranial defect in severe brain-injured patients. Chin J Traumatol. 2011;14:343-7.
- [Google Scholar]
- Cranioplasty after postinjury decompressive craniectomy: Is timing of the essence? J Trauma. 2010;69:270-4.
- [Google Scholar]
- Risk factors of post-traumatic hydrocephalus after decompressive craniectomy for patients with craniocerebral trauma. Chin J Trauma. 2014;30:307-10.
- [Google Scholar]
- Hydrocephalus after decompressive craniectomy for malignant hemispheric cerebral infarction. Int J Neurosci. 2016;126:707-12.
- [Google Scholar]
- Decompressive craniectomy is not an independent risk factor for communicating hydrocephalus in patients with increased intracranial pressure. Neurosurgery. 2010;67:675-8.
- [Google Scholar]
- Hydrocephalus following decompressive craniectomy for malignant middle cerebral artery infarction. Clin Neurol Neurosurg. 2012;114:555-9.
- [Google Scholar]
- Cisternostomy: Replacing the age old decompressive hemicraniectomy? Asian J Neurosurg. 2013;8:132-8.
- [Google Scholar]
- Cisternostomy for traumatic brain injury: Pathophysiologic mechanisms and surgical technical notes. World Neurosurg. 2016;89:51-7.
- [Google Scholar]
- Role of post-decompressive hydrocephalus in patients with malignant cerebral infarction. Turk Neurosurg. 2015;25:742-8.
- [Google Scholar]
- Persistent Brain Herniation after Decompressive Hemicraniectomy: Role of Lumbar Drainage for Cranioplasty.Case Report. Open Access Library Journal. 2016;3:e2346. http://dx.doi.org/10.4236/oalib.1102346.
- [Google Scholar]
- CSF lumbar drainage: A Safe surgical option in refractory intracranial hypertension associated with acute posttraumatic external hydrocephalus. Acta Neurochir Suppl. 2016;122:55-9.
- [Google Scholar]
- A simple method for controlled reduction duraplasty during cranioplasty. Br J Neurosurg. 2016;30:269-71.
- [Google Scholar]
- Evaluation of simultaneous cranioplasty and ventriculoperitoneal shunt procedures. J Neurosurg. 2014;121:313-8.
- [Google Scholar]
- Comparative study of outcomes between shunting after cranioplasty and in cranioplasty after shunting in large concave flaccid cranial defect with hydrocephalus. J Korean Neurosurg Soc. 2008;44:211-6.
- [Google Scholar]
- Decompressive craniectomy: Past, present and future. Nat Rev Neurol. 2013;9:405-15.
- [Google Scholar]
- Management of hydrocephalus after decompressive craniectomy. Turk Neurosurg. 2014;24:855-8.
- [Google Scholar]
- The effect of cranioplasty on cerebral hemodynamics: Evaluation with transcranial Doppler sonography. Neurol India. 2003;51:479-81.
- [Google Scholar]
- Complications of post-craniectomy cranioplasty: Risk factor analysis and implications for treatment planning. J Clin Neurosci. 2015;22:834-7.
- [Google Scholar]
- Computed tomography in the evaluation of incidence and significance of post-traumatic hydrocephalus. Radiology. 1981;141:397-402.
- [Google Scholar]
- Papilloedema as a non-invasive marker for raised intra-cranial pressure following decompressive craniectomy for severe head injury. Clin Neurol Neurosurg. 2011;113:635-8.
- [Google Scholar]
- [Semiology of ventriculoperitoneal shunting dysfunction in children - a review] Neurochirurgie. 2016;62:53-9.
- [Google Scholar]
- Surgical outcome of the shunt: 15-year experience in a single institution. Childs Nerv Syst. 2016;32:2377-85.
- [Google Scholar]
- Review of the management of peroral extrusion of ventriculoperitoneal shunt catheter. J Clin Diagn Res. 2016;10:PE01-6.
- [Google Scholar]
- An improved one-stage operation of cranioplasty and ventriculoperitoneal shunt in patient with hydrocephalus and large cranial defect. Korean J Neurotrauma. 2015;11:93-9.
- [Google Scholar]
- Cranioplasty for patients developing large cranial defects combined with post-traumatic hydrocephalus after head trauma. Brain Inj. 2008;22:333-7.
- [Google Scholar]
- Posttraumatic ventriculomegaly: Hydrocephalus or atrophy.A new approach for diagnosis using CSF dynamics? J Neurosurg. 1996;85:1026-35.
- [Google Scholar]






