Translate this page into:
Symptomatic Vertebral Hemangioma in a Young Child
Address for correspondence: Dr. Ravi Rajmohan, Department of Pharmacology and Neuroscience, School of Medicine, Texas Tech University Health Sciences Center, 3601 4th St., Lubbock, Tx 79430, USA. E-mail: ravi.rajmohan@ttuhsc.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vertebral hemangiomas (VHs) are the most common benign vertebral neoplasm and typically are asymptomatic, only to be discovered incidentally on imaging from the fourth to fifth decade of life. Seldom do they enlarge to a point of compression, causing pain and focal neurologic deficits. We present the rare case of an 8-year-old female who presented with paraparesis after a fall. Imaging revealed a pathological fracture of the T8 vertebra with retropulsion and spinal cord compression from both fracture and epidural tumor tissue. The patient underwent an anterior and posterior removal of the tumor, decompression, and fusion. Pathological report of specimen biopsy confirmed a benign hemangioma. To the best of our knowledge, this is the same age as the youngest previously reported case of symptomatic VH and it is the longest to be recurrence-free at follow-up. The hemangioma was successfully treated with tumor removal, decompression, and fusion. No adjuvant treatment was required, and she remained asymptomatic without recurrence at her 4-year follow-up.
Keywords
Benign vertebral neoplasm
jailhouse striations
pediatric vertebral hemangioma
vertebral decompression and fusion
INTRODUCTION
A rare subtype of vertebral hemangiomas (VH) includes a locally aggressive lesion that can lead to spinal cord compression, vertebral crush fractures, or vertebral body expansion.[123] We report the case and management of an aggressive VH at the T8 level presenting with signs of spinal cord compression in an 8-year-old female. To the best of our knowledge, this is the youngest case to present with motor deficits and to be corrected with surgical intervention.[4] The hemangioma was successfully treated with tumor removal, decompression, and fusion. No adjuvant treatment was required, and she remained asymptomatic without recurrence at her 4-year follow-up.
CASE REPORT
A previously healthy 8-year-old female presented after falling on her back while on the stairs. At the time of injury, she experienced no symptoms, but 3 days later, she begun to walk with a limp, experienced some leg weakness, and she had one episode of urinary incontinence. Neurological physical examination revealed bilateral proximal and distal weakness in her legs. Computed tomography (CT) imaging of the thoracic spine revealed a burst fracture of the T8 vertebra with an approximately 90% height loss at maximum. All vertebral components were involved with thickening of the pedicles [Figure 1]. Magnetic resonance imaging (MRI) showed a strongly enhancing lesion, including the epidural soft tissues [Figure 2] with severe spinal canal stenosis and resulting cord compression. Our initial differential diagnosis included eosinophilic granuloma, lymphoma, or metastatic disease. Since there was significant spinal cord compression with resulting neurological deficits, we elected for surgical intervention.

- Preoperative sagittal (a) and axial (b) computed tomography scans showing vertebra plana, erosion of pedicles, abnormal vertebral body surfaces, extension into the neural arch, and irregular trabeculae
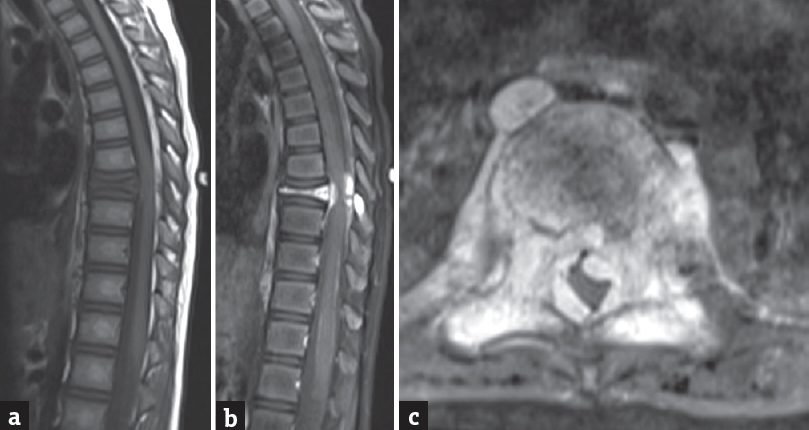
- Preoperative noncontrast sagittal T1 (a), postcontrast T1 sagittal (b) and postcontrast axial (c) magnetic resonance images showing significant contrast enhancement and soft-tissue involvement marking severe cord compression
The patient underwent a two-stage surgery while under the same anesthesia. First, an anterior T8 corpectomy was performed with tumor removal, placement of cage, and fusion. Subsequently, we completed a posterior T8 laminectomy, tumor removal, decompression, and T5 to T11 fusion. We were unable to obtain an intraoperative frozen study because the resected tissues were mostly composed of bone. There was significant intraoperative bleeding requiring multiple transfusions. No further immediate intraoperative complications were encountered, and overall, the patient tolerated the procedure well.
Postoperatively, the patient exhibited complete resolution of leg weakness. Pathology was confirmed to be a benign VH. Early postoperative scans confirmed a successful T8 corpectomy, laminectomy, and anterior/posterior fusion [Figure 3]. They also displayed one of the T10 pedicle screws to be violating the medial wall, and it was removed. Given the resolution of her symptoms, no further adjuvant treatment was warranted. At the time of her 4-year follow-up, she is doing well without recurrence. Her fusion appears free of signs of complication or deformity [Figure 4].
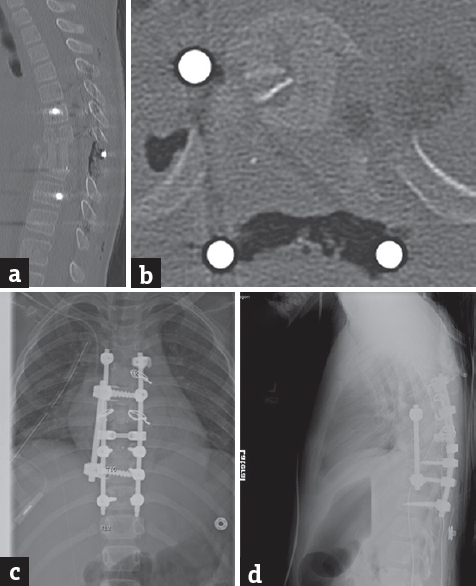
- Postoperative sagittal (a) and axial (b) computed tomography scans and posteroanterior (c) and lateral (d) X-rays showing decompressed spinal canal with hardware in place
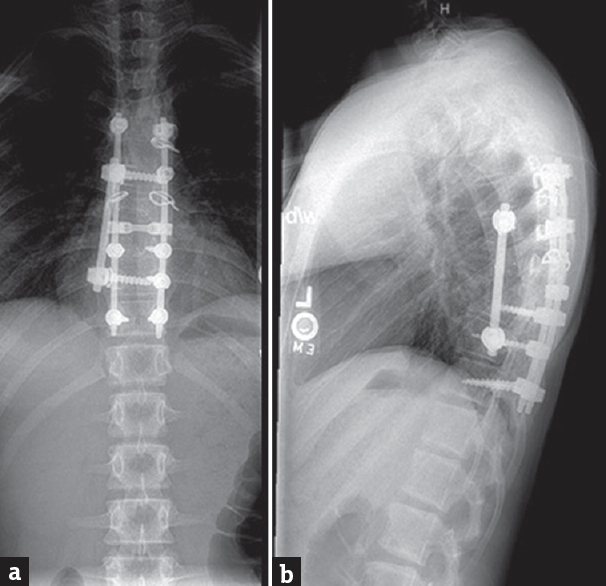
- Fourth year posteroanterior (a) and lateral (b) X-rays showing good fusion without significant deformity
DISCUSSION
Our case demonstrates the inherent difficulty in diagnosing these lesions. However, preoperative diagnosis of aggressive VH is advantageous since preoperative embolization allows for a reduction in the risk of life-threatening intraoperative bleeding.[56]
Diagnosis of an aggressive VH may be confused with metastatic disease due to its radiologic depiction, but characteristic findings exist to help with its differentiation.[1] Observation of “jailhouse striations” on plain radiographs, hyperintense signaling on T1-weighted MRI, and “polka-dot” pattern on CT are more typical of nonaggressive lesions, and their absence has been shown to be a reliable predictor of aggressiveness.[3578] Furthermore, compressive and aggressive lesions have a wider spectrum of radiographic findings, which include erosion of pedicles, abnormal vertebral body surfaces, extension into the neural arch, lytic areas, poorly defined cortical margins, and irregular trabeculae as was seen in our case [Figure 1].[167]
Initially, evidence of epidural soft-tissue involvement, which significantly narrowed the canal, caused us to reason that this was likely a lymphoma, metastatic disease, or eosinophilic granuloma. However, lesions that exhibit low-fat content with isointense signaling on T1-weighted and high signal on T2-weighted MRI are findings suggestive of hypervascularity and therefore possess an increased potential for cord compression as was also seen in our case [Figure 2].[910]
For aggressive cases with complete encasement of the vertebra, including both the anterior and posterior element, as with our case, conservative measures such as canal decompression with stabilization alone may not be curative.[2] We were able to accomplish gross debulking of the lesion, however, not without significant intraoperative bleeding requiring transfusions, a complication that could have been potentially minimized with embolization. We elected not to perform preoperative embolization because we did not want to delay surgery given the context of acute neurological deficit, rarity in children, and aggressive presentation, which lead us to suspect a more malignant lesion.
This case demonstrates that VHs, although a benign entity, can present with devastating spinal cord compression in pediatric patients. Due to their typical asymptomatic nature, VHs may fail to be included in the differential of mass lesion with resulting neurologic deficits. Characteristic imaging findings exist and can allow for the diagnosis and assessment of their severity. Preoperative diagnosis is beneficial because it allows for the consideration of preoperative embolization so that the risk of significant intraoperative bleeding requiring multiple transfusions can be lessened.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Vertebral hemangioma: An important differential in the evaluation of locally aggressive spinal lesions. Spine (Phila Pa 1976). 2010;35:E917-20.
- [Google Scholar]
- Comprehensive management of symptomatic and aggressive vertebral hemangiomas. Neurosurg Clin N Am. 2008;19:17-29.
- [Google Scholar]
- Lumbar vertebral hemangioma causing cauda equina syndrome: A case report. Spine (Phila Pa 1976). 2005;30:E662-4.
- [Google Scholar]
- Vertebroplasty for vertebral hemangioma in children: A report of two cases with 2-year follow-up. Childs Nerv Syst. 2015;31:2179-83.
- [Google Scholar]
- Clinical and imaging findings in patients with aggressive spinal hemangioma requiring surgical treatment. J Clin Neurosci. 2011;18:209-12.
- [Google Scholar]
- Symptomatic thoracic vertebral hemangioma: A case report and literature review. Arch Phys Med Rehabil. 2004;85:1544-7.
- [Google Scholar]
- Extraosseous extension of vertebral hemangioma, a rare cause of spinal cord compression. Spine (Phila Pa 1976). 1999;24:2111-4.
- [Google Scholar]






