Translate this page into:
Surgical treatment of 137 cases with chronic subdural hematoma at the university clinical center of Kosovo during the period 2008–2012
Address for correspondence: Dr. Ymer H. Mekaj, Institute of Pathophysiology, Faculty of Medicine, University of Prishtina, Rrethi i spitalit p.n. Prishtina 10000, Kosovo E-mail: ymer_mekaj@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Chronic subdural hematoma (CSDH) is frequent pathology in neurosurgical practice. The aim of this study is to present the first series of patients with CSDH, who got surgically treated in Clinic of Neurosurgery, University Clinical Center of Kosovo.
Materials and Methods:
This is a retrospective study that included 137 patients with CSDH who had been treated during the period 2008–2012. The data were collected and analyzed from the archives and protocols of the University Clinical Center of Kosovo. Patients were analyzed in many aspects such as age, gender, etiological factors, clinical features, localization, diagnoses, methods of surgical interventions, recurrences and mortality of patients.
Results:
From 137 patients with CSDH, 106 (77.3%) were males and 31 (22.7%) females. Average age of patients was 62.85 years. Analyzed according to the decades, the highest number of causes with CSDH was between 70 and 79 years (46%). The head trauma has been responsible for CSDH in 88 patients (64.3%), while the main symptom was headache (92 patients or 67.1%). One burr-hole trepanation with closed drainage system has been used in majority of cases (in 101 patients or 73.7%). The recurrence of CSDH was 6.5%, whereas mortality 2.9%.
Conclusion:
CSDH is more common in elderly patients. The male-female ratio is 3.4:1. Like other authors we also think that treatment with one burr-hole and drainage is a method of choice, because of its simplicity and safety.
Keywords
Burr-hole trepanation
chronic subdural hematoma
hematoma recurrence
subdural drainage
Introduction
Chronic subdural hematoma (CSDH) is an amount of liquid blood with dark red color surrounded by a thin capsule which usually formed for approximately 3 weeks.[1]
CSDH is one of the most common problems encountered in daily neurosurgical practice.[2] The incidence of CSDH is approximately 3.4 per 100.000 residents younger than 65 years. The old age increases greatly the incidence of CSDH, which amounts to 8-58 per 100.000 residents over the age 65.[23] According to Virchow chronic inflammation of the meninges, it can be considered as the cause of CSDH.[4] Head trauma is usually considered responsible for the development of CSDH, especially in older people, which initially seems insignificant, may be the cause for the genesis of CSDH.[5] Most of patients with CSDH, which is manifested with clinical symptoms, should be operated for evacuation of CSDH. The surgical intervention can be performed with a range of procedures starting from twist drill craniostomy to craniotomy and membranectomy.[6]
Burr-hole craniostomy is an easier and more efficient surgical procedure, which is usually selected for drainage of uncomplicated CSDH.[7] Evacuation of CSDH through burr-hole becomes the procedure of choice in many hospitals because of its simplicity and the lower operative risks. However, it has been reported that recurrence rate range from 9.2% to 26.5% after application of this procedure for surgical evacuation.[8] However, there are some studies that have been reported of other recurrence values, which were from 2.3% to 37%.[5] Stanisic et al. have mentioned some studies about numerous factors potentially associated with recurrences after the surgical procedures which are still highly controversial.[9]
The present retrospective study analyzed the results a single one versus two burr-hole trepanation with closed-system drainage or craniotomy.
Materials and Methods
This is a retrospective study that included 137 patients with CSDH treated in Clinic of Neurosurgery, University Clinical Center of Kosova during the period 2008–2012. The data were collected and analyzed from the archives and protocols of the University Clinical Center of Kosova. Diagnosis was confirmed by computed tomography (CT) scans and/or by magnetic resonance (MR) images in all patients. A surgical evacuation was performed when the hematoma's thickness was larger than 10 mm, when focal symptoms were present, or when there were significant changes in neurologic status in patients with CSDH of any thickness. In patients who have used oral anticoagulants, this therapy has been stopped until normalization of international normalized ratio (INR). In case of an emergency procedure and coagulopathy, anticoagulant status was reversed with vitamin K and fresh frozen plasma, in order to immediately perform surgery procedure. In order to prevent infections preoperatively, we used antibiotics of third generation cephalosporin.
Operations were performed under either general or local anesthesia. In our patients we used different surgical procedures such as one or two burr-hole trepanation with closed-system drainage or craniotomy with membranectomy. The selection of the number of burr-holes was dependent on the neurosurgeon's preference. The burr-hole trepanation was made at the site of the maximal existing hematoma. After the dura has been opened, the collection of blood was evacuated under its own tension, and irrigation was performed using physiological saline solution until clear fluid came out. Thereafter, a closed subdural system has been placed, which works without any negative pressure, (infant feeding tube was used instead of subdural catheter). Subdural drainage was continued up to 72 h after surgery. After evacuation of the hematoma, the patients routinely received intravenous fluid therapy consisted of crystalloids approximately 2000 ml/day over at least 3 postoperative days. Subcutaneous injection of 40 mg of enoxaparin was used after 24 h of surgical procedures for prophylaxis against deep vein thrombosis during the patient's hospitalization. The patients were analyzed by age, sex, the presenting signs and symptoms, Glasgow Coma Scale (GCS), origin type of surgical procedure, side of the skull in which the hematoma occurred, days of hospitalization, Glasgow Outcome Scale (GOS) at discharge, recurrence and mortality. Data processing was done with the statistical package In Stat 3. From statistical parameters arithmetic median and standard deviation were calculated. Data testing is done with T-test and the difference is significant if P < 0.05.
Results
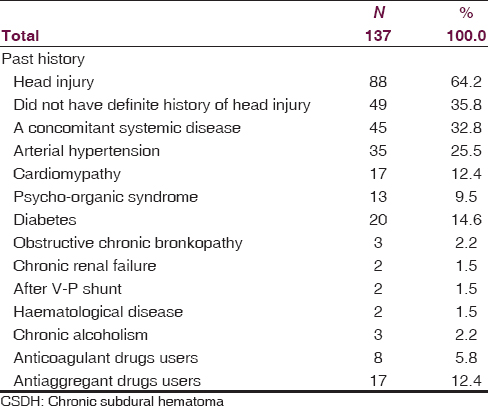
In this retrospective study are included 137 patients in a 5 year period with CSDH treated in Clinic of Neurosurgery, University Clinical Center of Kosova. Out of 137 patients, CSDH was predominant in male gender with 106 cases or 77.3%, while 31 cases were female or 22.7%, and male to female ratio was 3.4:1. Patients with CSDH had a very wide age distribution from 1 to 89 years with an average age of 62.85 years. Regarding the age group, the age group 70-79 with 44 cases dominates, followed by the age group 60-69 years 30 cases, 80-89 years 22 cases, 40-49 years 11 cases, 10-19 years 5 cases, 01-09 years 4 cases, 20-29 years 2 cases, and 30-39 years 2 cases [Table 1]. Clinical presentation of patients with CSDH was characterized with a lot of symptoms [Table 2], from which the headache was a common symptom, occurring in 92 patients (67.1%), which was followed by contralateral motor deficit 66 patients (48.1%), speech disturbance 37 patients (27%), and altered behavior 34 patients (24.8%). Etiological causes of CSDH are numerous. Head trauma was the most frequent cause, which has been responsible for CSDH in 88 patients or 64.2% while 49 patients (35.7%) did not have definite history of head trauma [Table 3]. As shown in this table there are other presented factors associated with CSDH such as: Concomitant systemic disease was identified in 45 patients (32.8%), arterial hypertension in 35 patients (25.5%), cardiopathy in 17 (12.4%), psycho-organic syndrome in 13 (9.4%), diabetes 20 (14.5%), obstructive chronic bronchopathy in 3 (2.1%), chronic renal failure in 2 cases (1.4%), after V-P shunt in 2 cases (1.4%), hematological disease in 2 cases (1.4%), chronic alcoholism in 3 cases (2.1%), anticoagulant drug use in 8 (5.8%) and antiaggregant drug use in 17 (12.4%). In Table 2, patients are presented based on GCS at admission as follows: 91 patients (66.4%) had GCS of 15-14 points, 31 patients (22.6%) had GCS of 13-9 points and 15 patients (10.9%) had GCS of 8-3 points (table per GCS). The median value of the GCS at admission was 13.5.

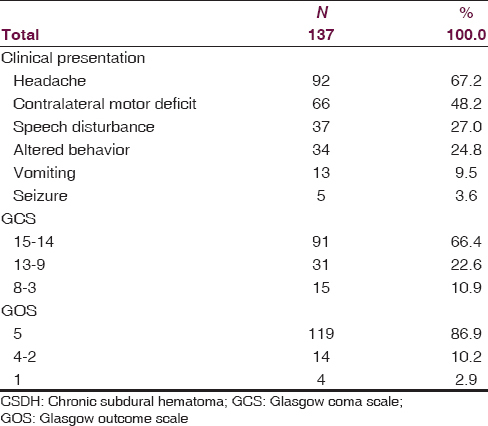
Out of the total number of patients (137), 119 or 86.8% of them had positive outcome (GOS 5), while 14 patients or 10.2% (GOS 4-2) had poor outcome. Mortality was in four patients or 2.9%. In these patients the general outcome at the time of discharge were assessed according to GOS with range 1-5.
In 105 (76.6%) patients, diagnosis of CSDH was confirmed with computed tomography (CT), while in 32 (23.4%) patients with magnetic resonance imaging (MRI). The majority of patients (92 or 67.1%) were operated under local anesthesia (monitored anesthesia care), while the remaining (45 or 32.8%) under general anesthesia [Table 4].
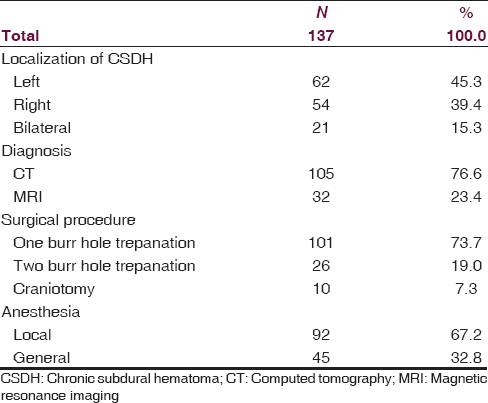
Hematoma localization has been greater on the left side (62 patients or 45.2%) than on the right side (54 patients or 39.4%), while bilateral hematomas were present in 21 patients or 15.3%. Our patients were treated with one versus two burr-hole trepanation, but some of them by craniotomy. Forty-seven patients with the hematoma of the left side were treated with a one burr-hole trepanation, whereas 10 of them were treated with two burr-hole trepanation, and 5 of them with craniotomy. The treatment of hematoma on the right side is made similar to that on the left side: 36 with one burr-hole trepanation, 14 with two burr-hole trepanation and 4 with craniotomy. Of 21 patients with bilateral hematoma, 18 of them are treated with one burr-hole trepanation per side, in 2 cases are made two burr-hole trepanation per side and only 1 patient was treated with bilateral craniotomy [Table 4]. The duration of hospitalization ranged from 2 to 46 days, with a mean of 8.6 days of hospitalization. Duration of treatment in 26 cases (18.9%) was over 10 days, with the maximum days of hospitalization up to 46 days, whereas in 23 cases (16.7%) it was up to 5 days. In 88 cases (64.2%), hospitalization lasted up to 10 days.
Reviewed by the years that have been analyzed, it is seen that distribution of CSDH had the following features: In 2012 the incidence of CSDH was the highest (35 cases or 25.5%), while in 2010 it was the lowest (21 cases or 15.3%).
Distribution of CSDH in years had the following features: 2012 is the year in which the incidence of CSDH was the highest with 35 cases (25.5%), followed by 2009 with 28 cases (20.4%), 2011 with 27 cases (19.8%), 2008 with 26 cases (18.9%), and 2010 with 21 cases (15.4%). Among 137 operated patients, 9 patients (6.5%) were re-operated because of recurrence. Four of these patients were re-operated with craniotomy. We did not register any case of further recurrence (re-recurrence), as well as for other complication such as: Postoperative subdural empyema, meningitis and wound infection. It is worth-mentioning that of the total number of operated patients, four of them (2.9%) died in the early post-operative period.
Discussion
CSDH is relatively common in neurosurgical practice,[2] which is caused by a large number of etiological factors, first of all by the action of various traumatic factors. However, the etiology of CSDH is not completely understood until now.[10] The purpose of this retrospective paper was to present the cases with CSDH which were surgically treated in our clinic (137 patient) during the period of 5 years, from 2008 to 2012. Patients who were treated in our clinic were analyzed in many aspects such as age, gender, etiological factors, clinical features, localization, diagnosis, methods of surgical interventions of CSDH, GCS and GOS, distribution of CSDH over years, concomitant diseases, duration of hospitalization, recurrences and mortality of patients.
According to the data from literature, CSDH is pathologic condition which is mostly present in older people from 50 to 70 years. The average age of our patients (62.85 years) was younger than the average age reported by other authors such as Gelabert-Gonzales et al. (72.7 years)[2] and Gastone et al. (76.4 years).[11] On the contrary, the ratio of male to female which we found in our patients (3.4:1) was higher than ratio which is found by above authors,[211] which was 1.68:1. Also, the higher frequency of CSDH in males compared to females was found by other authors.[121314] As reported in our results, head trauma was the most frequent cause responsible for CSDH in 88 patients or 64.2%, while 49 patients (35.7%) did not have definite history of head trauma, but may be due to some other pathological conditions such as: Arterial hypertension, hematological disease, chronic renal failure, after V-P shunt, chronic alcoholism, patients under anticoagulant and antiaggregant therapy. These associated factors with development of CSDH are presented in Table 3. Our results about the frequency of head trauma (64.2%) as a causative factor for CSDH are similar to those of other authors, which report that head trauma is responsible for CSDH in 35-75% of patients.[141516] Clinically, CSDH is characterized with a lot of symptoms. In our study the dominant symptom was headache (67.1%), whereas seizure was present in only 3.6% of cases [Table 2]. The similarly symptoms and the same frequency were reported also by Gelabert-Gonzαlez et al., Mori and Maeda, and Sousa et al.[21017] Our results are in accordance with the results of Sousa et al.[17] about the finding that headache is more frequent in younger patients. Localization of the CSDH may be unilateral (left or right) or bilateral. We have found that the CSDH is more frequent on the left side (45.3%), compared with the right side (39.4%), while bilateral CSDH have been in lowest percentage (15.3%). Also, other authors have reported the higher frequency of the CSDH on the left side.[1819] Surgical procedures for patients with CSDH were performed with one versus two burr-hole trepanation with a closed drainage system and craniotomy. Some authors agree that the optimal surgical treatment of patients with CSDH can be achieved with one burr-hole trepanation with a closed drainage system.[1220] We have used this surgical procedure in our clinic in 101 patients or in 73.7% of them. Although the opinion of the other authors is different, they think that extended craniotomy enables better exposure of CSDH with solid components.[2122] The data from literature show that regardless of surgical procedures, the operation is accompanied by recurrence rates of 4% to 26%.[21023] The number of recurrence in our series was 6.5% equals those of the other authors.[61220] According to the Robinson,[14] old age considered to be a risk factor for recurrence. Our results are in accordance with this conclusion, because the average age (71.44 years) of our 9 re-operated patients has been higher than the average age (62.25 years) of non-re-operated patients. In the present study, recurrence of CSDH was found at 1 to 12 weeks (mean 4.5 weeks) after the first operation. We did not register any case of further recurrence (re-recurrence). However, in some studies, it is not demonstrated the relationship between recurrence rate and age.[13] Furthermore, acquired or inherited disorders of homeostasis represent a very important clinical factor, which are responsible for the CSDH and consequently for recurrence and mortality rate. In the present study, we have found five cases with iatrogenic CSDH, who have been under uncontrolled treatment with oral anticoagulants (four cases) and antiaggregants (one case). Four patients (2.9%) of our series have died in the early post-operative period, in comparison to 2.7% mortality reported in the literature.[1020] However, according to some authors, mortality varies from 0% to 13%.[24]
Conclusions
One of the most frequent neurosurgical problems is the CSDH, which unfortunately can lead to the death of the patients. For this reason, there are a lot of retrospective studies, which describe the basic characteristics of the CSDH such as: The incidence, etiology and pathogenesis, clinical symptoms, diagnostic and surgical procedures, success of treatment, recurrence and mortality. In the present study, the most common etiological factor was the head trauma, whereas the headache was the most frequent symptom in younger patients. The majority of patients with CSDH were over the age of 50. Diagnosis and localization of the CSDH were done with CT or MRI, while in the majority of the patients, the operative treatment was performed with burr-hole trepanation with closed drainage system, which according to some authors is a simple, safe and efficient method. We expect even better results if we use subdural catheter instead of infant feeding tub. However, the kind of surgical method is still controversial, and a standard method does not exist. In our experience, there are several factors (concomitant disease, diabetes, arterial hypertension, etc.), which act negatively on operating outcome. Despite any cases of perioperative deaths, we can say that the CSDH is considered curable disease.
Acknowledgements
We thank the arshive and all the staff of the Clinic of Neurosurgery for their technical support.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Recurrence factors for chronic subdural hematomas after burr-hole cranioctomy and closed system drainage. Neurol Res. 1999;21:277-80.
- [Google Scholar]
- Chronic subdural hematoma: Surgical treatment and outcome in 1000 cases. Clin Nurol Neurosurg. 2005;107:223-9.
- [Google Scholar]
- Chronic and subacute subdural hematoma. An epidemiological study in a captive population. Rev Neurol. 2001;32:821-4.
- [Google Scholar]
- Treatment of chronic subdural hematoma through a burr hole. Cir Cir. 2010;78:203-7.
- [Google Scholar]
- Chronic subdural hematoma: The role for craniotomy reevaluated. Neurosurgery. 1993;33:67-72.
- [Google Scholar]
- Modified twist drill technique in the management of chronic subdural hematoma. Turk Neurosurg. 2013;23:50-4.
- [Google Scholar]
- Treatment of chronic subdural hematoma with burr-hole craniostomy and closed drainage. Br J Neurosurg. 1995;9:619-27.
- [Google Scholar]
- Treatment of chronic subdural hematoma by burr-hole craniotomy in adults: Influence of some factors on postoperative recurrence. Acta Neurochir (Wien). 2005;147:1249-57.
- [Google Scholar]
- Surgical treatment of chronic subdural hematoma in 500 consecutive cases: Clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med chir (Tokyo). 2001;41:371-81.
- [Google Scholar]
- Chronic subdural hematoma: Results of a homogeneous series of 159 patients operated on by residents. Neurol India. 2004;52:475-7.
- [Google Scholar]
- Chronic subdural hematoma: Surgical treatment and outcome in 104 patients. Surg Neurol. 1997;48:220-5.
- [Google Scholar]
- Factors in the natural history of chronic subdural hematomas that influence their post-operative recurrence. J Neurosurg. 2001;95:256-62.
- [Google Scholar]
- Chronic subdural hematoma: Surgical management in 133 patients. J Neurosurg. 1984;61:263-8.
- [Google Scholar]
- Epidemiological characteristics of 778 patients who underwent surgical drainage of chronic subdural hematomas in Brasilia, Brazil. BMC Surgery. 2013;13:5.
- [Google Scholar]
- Chronic subdural hematomas and the elderly: Surgical results from series of 125 cases: Old “horses” are not to be shot! Surg Neurol Int. 2012;3:150.
- [Google Scholar]
- Chronic subdural hematomas are more common on the left on the right. J Clin Neurosci. 2009;16:642-4.
- [Google Scholar]
- Chronic subdural hematoma treated by burr holes and closed system drainage: Personal experience in 131 patients. Br J Neurosurg. 1991;5:461-5.
- [Google Scholar]
- Chronic subdural hematoma: Its pathology, its relation to pachymeningitis hemorrhagica, and its surgical treatment. Arch Surg. 1925;11:329-93.
- [Google Scholar]
- The role of craniectomy in the treatment chronic subdural hematomas. J Neurosurg. 1980;52:776-81.
- [Google Scholar]
- Demographics and prevalent risk factors of chronic subdural hematoma: Result of a large single-center cohort study. Neurosurg Rev. 2004;27:263-6.
- [Google Scholar]
- The management of primary chronic subdural hematoma: A questionnaire survey of practice in the United Kingdom and the Republic of Ireland. Br J Neurosurg. 2008;22:529-34.
- [Google Scholar]






