Translate this page into:
Successful Endovascular Neurosurgical Practice in Resource-poor Exclusive Rural Neuro-hospital Setup
Address for correspondence: Dr. Kamble Jayaprakash Harsha, Department of Endovascular Neurosurgery, Indo American Hospital and Brain and Spine Centre, Chemmanakary, Vaikom - 686 143, Kerala, India. E-mail: kjharsha@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
The aim of this study to evaluate the feasibility of establishing endovascular neurosurgery in remote resource-poor neuro-hospital setup and evaluate its outcome.
Materials and Methods:
Retrospective analysis of diagnostic and therapeutic endovascular neurosurgical procedures performed during September 2013–June 2016.
Results:
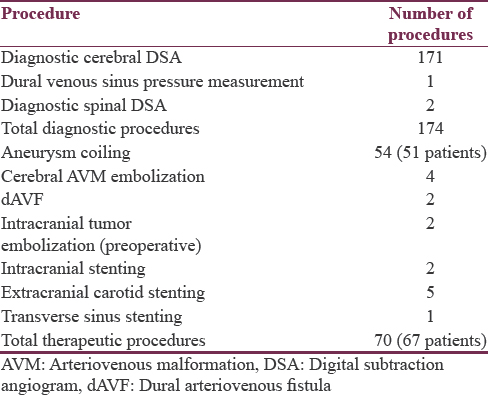
A total of 174 diagnostic cerebral and spinal digital subtraction angiograms and 70 major endovascular neurosurgeries were performed during the period. The endovascular neurosurgical procedures included 54 aneurysms coiled, 4 cerebral arteriovenous malformation embolization, 2 dural arteriovenous fistulas embolization, 2 cerebral tumor embolizations, 2 intracranial stentings, 5 extracranial carotid stentings, 1 transverse sinus stenting. No complications were seen during diagnostic procedures. Operation related morbidity of 1.4% and mortality of 1.4% seen, with a procedural success rate of 97.2%.
Conclusion:
Endovascular neurosurgery is feasible in resource-poor remote rural exclusive neuro-hospital setup with procedural success rate and outcomes comparable to existing literature.
Keywords
Aneurysm coiling
digital subtraction angiogram
endovascular neurosurgery
rural hospital
INTRODUCTION
Endovascular neurosurgical specialty is a fast upcoming clinical field, having different names – neurointerventional surgery, interventional neuroradiology, and interventional neurology. Considering limited structured courses available in India, number of doctors trained in this field is far less than the existing demand. Furthermore, the infrastructure needed for the specialty is limited to big hospitals. Hence, most of the experts in the field are available only in major cities of India.[1] While few suburban centers with adequate resources are emerging.[2] Availability of these facilities in rural setup is, to the best of our knowledge, not available. Establishing the department is also hindered by nonavailability of good quality cath laboratory in the rural setup, availability of trained cath laboratory technicians and nurses. The other disadvantage being immediate nonavailability of hardware required for emergency procedures like hyperacute stroke management. The article summarizes the feasibility of establishing an endovascular neurosurgical setup in remote rural exclusively neuro-hospital, where resource availability was limited, still achieving results comparable to existing literature results.
MATERIALS AND METHODS
The hospital medical records were reviewed retrospectively, to obtain data of patients undergoing major endovascular neurosurgical procedures from August 2013 to May 2016. Patient demographics such as age, sex, initial Glasgow coma scale, computed tomography (CT)/digital subtraction angiogram (DSA)/magnetic resonance imaging and magnetic resonance angiogram (MRA) findings were obtained. Follow-up data were also collected and modified Rankin score (mRS) at the end of follow-up period was derived.
Preoperative evaluation
All cases were evaluated clinically for fitness for procedures in current hospital setup, along with anesthetists. Basic blood investigations, chest X-ray, and electrocardiography were performed. All patients were managed in neurosurgical Intensive Care Unit (ICU), ward as per the requirements both during pre- and post-operative period. Due to limited availability of expertise in devices and monitoring of pediatric cases, both diagnostic and endovascular neurosurgical procedures were not accepted in patients aged below 12 years. Similarly, large dural arteriovenous fistulas (dAVFs) and arteriovenous malformations (AVMs) requiring prolonged X-ray tube exposure or biplane images were also rejected during presurgical screening. Few cases requiring flow diverter deployment were also rejected fearing inferior quality images and limited heat capacity of the X-ray tube. Hyperacute stroke treatment though was feasible with available setup; no cases were performed due to less number of patients reaching within window period/economic constraints from most of the patients.
Postoperative management
All subarachnoid hemorrhage (SAH) patients were managed in ICU and ward for 14–20 days as per the standard guidelines.[3] All coiled patients received dexamethasone postoperatively for about 4 weeks.[4] Considering the nonavailability of transcranial Doppler for monitoring of post-SAH vasospasm development, patients with SAH were monitored clinically for development of symptomatic vasospasm, if clinically suspected, then only were subjected for MRA. All immobile patients received deep vein thrombosis (DVT) prophylaxis (either lower molecular weight heparin or DVT compression pump or compression stockings or combination). The compression ultrasound was performed only if DVT was suspected clinically. Minor postoperative problems such as hypo/hypernatremia, hypokalemia, respiratory tract infection, and urinary tract infection, were managed as per the standard guidelines.
Image acquisition
Shimadzu surgical mobile C-arm WHA-200 opescope pleno imaging system upgraded with DSA software was used for diagnostic cerebral DSA and subsequent endovascular neurosurgical procedures. The machine also had roadmapping software necessary for coiling. The machine has one live monitor and one reference monitor, manually rotatable X-ray tube assembly. Diagnostic cerebral angiograms and endovascular neurosurgical procedures were planned at an interval of at least 2 h to allow cooling of X-ray tube. Standard anteroposterior and lateral views along with additional multiple oblique views were obtained for aneurysms till proper working projection for aneurysm coiling obtained.
Follow-up imaging
Patients were encouraged to undergo DSA/MRA during follow-up to assess residual/recurrence of the disease. As the hospital was equipped with 6 slice CT scan without dedicated CT angiographic softwares, MRAs were used for follow-up of all patients, DSA being offered if repeat coiling was considered. MRAs were obtained using 16 channel matrix coil on a 1.5T clinical scanner (Essenza, Siemens, Erlangen, Germany). Three-dimensional (3D) time-of-flight MRA was obtained with TR of 26 ms, TE of 7.15 ms, matrix of 512 × 512, followed by maximum intensity projection thick slab reconstruction. Residual/recurrence of neck and dome were noted in both reconstructed and source images.
RESULTS
The procedures performed are divided into diagnostic and therapeutic procedures, summarized in Table 1.
Diagnostic digital subtraction angiogram
A total of 174 diagnostic DSAs were performed during the study. Lack of 3D rotational angiographic technique in the machine was compensated by acquiring multiple angle images. At times, continuous injection of contrast with constant fluoroscopic changing of angle was performed to separate parent vessel from the neck of an aneurysm. Limited image magnification capacity was overcome by decreasing tube-head distance. No diagnostic DSA-related complications were seen.
Aneurysms coiling
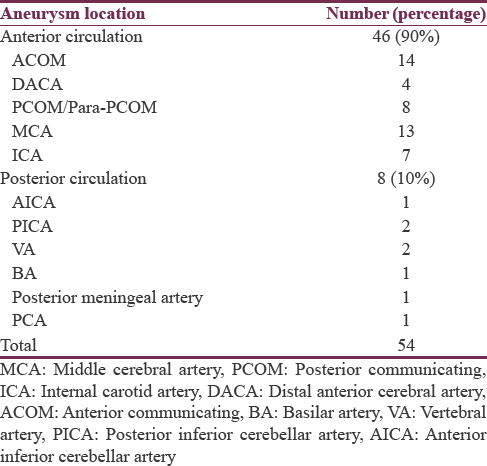
Only 30% of all aneurysmal SAH patients were willing to undergo endovascular coiling due to financial constraints. This is in accordance with practice in the rest of the country, where surgical clipping is prevailing and preferred treatment of choice.[1] Our center is one of high-volume center, with 60–80 new SAH cases/year being referred for treatment.[3] A total of 51 patients (male:female = 23:28), with mean age of 54 years (range 20–75 years) underwent coiling of 54 aneurysms during the study. Fifty aneurysms were ruptured, while four were unruptured. The location and number of aneurysms in a particular location are depicted in Table 2. One patient was harboring 4 aneurysms, two of which were coiled, one was clipped and one was wrapped. Two patients were harboring two or more aneurysms, of which ruptured aneurysm was coiled, and other aneurysm/s were followed up. One patient with a headache without SAH, diagnosed to have mirror ophthalmic segment internal carotid artery (ICA) aneurysms, underwent coiling of both aneurysms in same sitting [Figure 1]. Two patients underwent elective stent-assisted coiling, while two patients needed unexpected intraprocedural stent deployment to prevent coil prolapse.
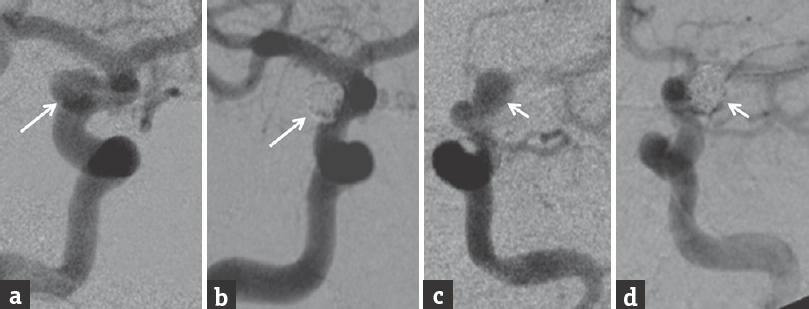
- Initial digital subtraction angiogram anteroposterior view of right (a) and left (c) internal carotid artery angiogram showing saccular aneurysm (b and d) postcoiling digital subtraction angiogram showing complete obliteration of aneurysms
Clinical follow-up of variable period from 1 to 27 months was available in 48 patients. Thirty-seven patients had follow-up mRS of zero; three patients had mRS of two, seven patients with preprocedure mRS of 3–5 showed variable improvement, however, final follow-up mRS remained 3–5. One patient developed stroke due to coiling and parent artery occlusion, and one procedure-related mortality was attributed to intraprocedure re-rupture of aneurysm. Two procedure-unrelated mortalities, one patient, died during postoperative period due to suspected myocardial infarction, other patient had severe vasospasm and middle cerebral artery (MCA) territory acute infarct at the time admission, progressed to malignant infarct and died.
Imaging follow-up was available in 46 patients; one patient had significant basilar top aneurysm dome recurrence due to coil compaction, however, denied further repeat coiling. Three patients had small aneurysm neck/dome recurrence, were managed conservatively, uneventful clinically till the end of the follow-up period.
Arteriovenous malformation and dural arteriovenous fistulas embolizations
One patient with Cognard Type IV and another patient with Cognard Type IIb dAVF underwent complete occlusion of the fistula by embolization. Four patients with cerebral AVM underwent embolization. One patient with left motor cortex AVM (Spetzler Martin Grade II) underwent complete occlusion of nidus in the first sitting; his 6 months follow-up DSA did not show residual/recurrence, his neurological status (mRS 3) remained unchanged during follow-up. The second patient with left motor cortex AVM (Spetzler Martin Grade II) underwent 80% embolization of nidus, however, denied further embolization sessions due to financial issues. The third patient with corpus callosal and cingulate gyrus AVM (Spetzler martin Grade IV) [Table 2], underwent partial embolization, developed intraventricular hemorrhage during postoperative period and succumbed. The fourth patient had right occipital-parietal AVM (Spetzler Martin Grade IV), underwent partial glue embolization of deep feeders, followed by surgical excision of the lesion, postoperative DSA showed complete obliteration of AVM.
Tumor embolizations
One hemangioblastoma and one esthesioneuroblastoma tumors were partrially embolized using polyvinyl alcohol particles, without procedure-related complications. However, considering poor resolution of the machine to identify dangerous ICA-external carotid artery anastamosis, further intracranial tumor embolizations were avoided.
Intracranial stentings
Two patients with right cavernous ICA critical stenosis with stroke, who were refractory to medical management underwent, self-expandable nitinol stenting followed by balloon dilatation. Postprocedure period mild improvement in clinical symptoms were noted, no recurrence of transient ischemic attack symptoms were seen, which persisted during 1-year follow-up.
Extracranial carotid stenting
Five patients underwent extracranial carotid artery stenting using either proximal (two patients) or distal protection device (three patients). All five patients had 50%–80% stenosis in DSA and recent minor stroke. Two patients had contralateral ICA occlusion. One patient in whom, proximal protection device was used, developed small watershed territory infarct, resulting in dropping of mRS by one score, who recovered back to his previous mRS during subsequent 6 months follow-up. No other intra/peri-operative complications were noted. Rest of four patients had 6 months to 1 year clinical and Doppler follow-up without significant recurrent stenosis/recurrence of clinical symptoms.
Transverse sinus stenting
One patient had medically refractory headache and fundoscopy documented papilledema, having one transverse sinus hypoplastic and other dominant transverse sinus stenosis (80%), underwent venous sinus stenting, followed by antiplatelets. Her 1 year clinical and imaging follow-up showed recurrence of stenosis and clinical symptoms, antiplatelets were replaced with anticoagulants, following which her symptoms disappeared.
Hyperacute stroke endovascular treatment
Considering the rural setup and low awareness among patients to reach within 6 h of onset of stroke,[5] only few patients reached the hospital within the window period. Although some patients reaching within window period underwent intravenous thrombolysis using rTPA, none of patients underwent intra-arterial (IA) interventions (IA thrombolysis/mechanical aspiration/mechanical thrombectomy) due to financial constraints.
Postoperative complications
All patients were observed in ICU for variable period. None had puncture site complications. One patient with SAH developed clinically symptomatic vasospasm, improved completely with augmented HHH therapy. One patient had neurogenic cardiomyopathy (Takotsubo cardiomyopathy), bystanders denied immediate coiling due to high perioperative mortality, was managed conservatively for 2 weeks, during which her cardiac status improved and underwent uneventful coiling. One patient anterior communicating aneurysm and SAH with body mass index of >40, had developed obesity hypoventilation syndrome (Pickwickian syndrome) during postoperative period, was managed conservatively with successful recovery at the end 2 weeks. One female patient with left MCA bifurcation aneurysm and SAH (mRS 5), developed massive pulmonary thromboembolism, was managed medically with successful complete recovery, had mRS 2 at the end of 1-year follow-up. One patient with ruptured MCA bifurcation aneurysm had developed Brugada syndrome on the 14th postoperative day, had an episode of syncope and cardiac arrest, revived successfully with cardiopulmonary resuscitation, remained asymptomatic at the end of 1-month clinical follow-up. Although clinically asymptomatic/minimally symptomatic vasospasm was common (50%–60%), none required either endovascular interventions for vasospasm nor developed clinically significant persistent delayed ischemic neurological deficit.
DISCUSSION
India harbors 17.5% of the world population, of which 68% of the population lives in rural areas. While most superspeciality of hospital are centered around urban areas, our institute is unique in that it is located in rural area and attracts patients from rural dominant mid-Kerala [Figure 2]. The rural-based tertiary neuro-hospital is located in close access to four rural dominant districts of mid-Kerala, namely Kottayam with population density of 895 persons/km2 (population 1.97 million, rural - 71.3%, Urban - 28.7%), Alappuzha with population density of 1504 persons/km2 (population - 2.12 million, rural 46%, urban 54%), Idukki with population density of 255 persons/km2 (population - 1.1 million, rural - 95%, Urban - 5%), and Pathanamthitta with population density of 452 persons/km2 (population - 1.19 million, rural - 89%, Urban - 11%). The hospital is the first of its kind in Kerala intent to provide quality exclusive neurology and neurosurgical care to rural and suburban population. The hospital being a charitable institute, limited resource settings were initially deemed to be unfit for advanced neuroendovascular operations.
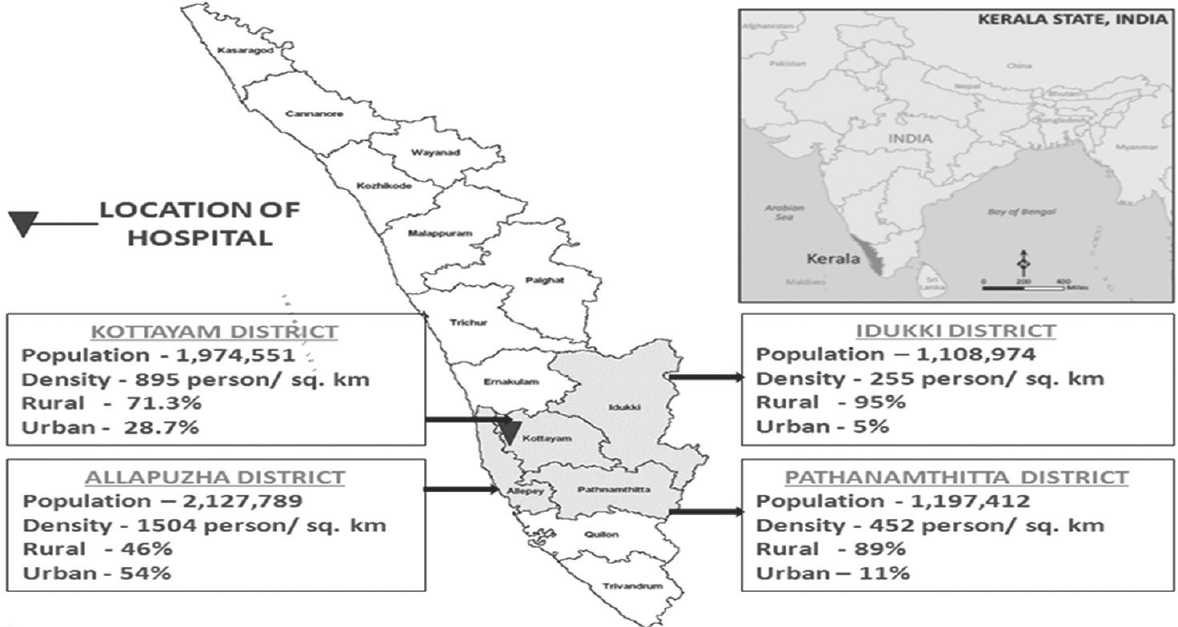
- Geographic location of Indo-American Hospital and the population it caters to
Initial 2–3 months were spent in training of operation theater nursing staff, paramedical staff and radiology technician about neuroendovascular operations and their role in the successful outcome of surgery. Considering low heat dissipating capacity of machine, fluoroscopic and DSA time were kept to a minimum as possible. Despite this, during the end of two large aneurysm coiling procedures, coiling was interrupted for a short period due to excessive heating of X-ray tube. Limited resources also demanded extreme clinical expertise in pre- and post-operative period clinical management of patients. As most of the patients were from low and mid economic strata, patients accepting, advanced neuroendovascular operations were <30%, though trend showed patients opting more and more for endovascular treatments. Despite several limitations, procedural success rate of 97.2%, procedure-related mortality rate of 1.4% and procedure-related morbidity of 1.4% results were achieved, which are comparable to literature.[6] Follow-up clinical outcomes were also comparable to literature.[7]
With appropriate expertise in both clinical and technical fields in the subject, it is feasible to establish endovascular neurointerventional setup in rural exclusive neuro-hospital setup. This single center rural experience in neuroendovascular interventions is, to the best of our knowledge, first of its kind in India. Our single center experience has proved that global trend of increasing utility of endovascular treatments is not only limited to urban and suburban setup, but it is also feasible in rural setup as well.[8]
CONCLUSION
While endovascular neurosurgical facilities are mostly limited to major urban setup in large hospitals of India, it is feasible to offer good service in this field even in remote rural basic hospital setup, with outcomes comparable to existing literature. Nevertheless, clinical expertise is essential to manage patients during pre- and post-operative period for successful final clinical outcome in resource-poor setup, irrespective of procedural success.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Dr. Raghavendra S, Dr. Mohammed Iqbal Jaser, Consultant Anaesthetists, Indo American Hospital Brain and spine centre, Chemmanakary, Vaikom, Kerala.
REFERENCES
- Cerebral aneurysm treatment in India: Results of a national survey regarding practice patterns in India. Neurol India. 2016;64(Suppl S1):62-9.
- [Google Scholar]
- Endovascular neurointervention success and complication rates in the first year of independent practice in a suburban hospital setup. J Neurosci Rural Pract. 2014;5:11-7.
- [Google Scholar]
- Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43:1711-37.
- [Google Scholar]
- Corticosteroids for aneurysmal subarachnoid haemorrhage and primary intracerebral haemorrhage. Cochrane Database Syst Rev. 2005;3:CD004583.
- [Google Scholar]
- Poor awareness of stroke – A hospital-based study from South India: An urgent need for awareness programs. J Stroke Cerebrovasc Dis. 2014;23:2091-8.
- [Google Scholar]
- Morbidity and mortality of patients with endovascularly treated intracerebral aneurysms: Does physician specialty matter? J Neurosurg. 2016;124:13-7.
- [Google Scholar]
- Case-fatality rates and functional outcome after subarachnoid hemorrhage: A systematic review. Stroke. 1997;28:660-4.
- [Google Scholar]
- Global differences in the present and future management of cerebral aneurysms. World Neurosurg. 2013;80:717-22.
- [Google Scholar]






