Translate this page into:
Subdural hematoma presenting as trigeminal neuralgia: A case report
Address for correspondence: Dr. Michele Pistacchi, Santorso Hospital, Garziere Street 73, 36014 Santorso VI, Italy. E-mail: michelepistacchi@yahoo.it
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
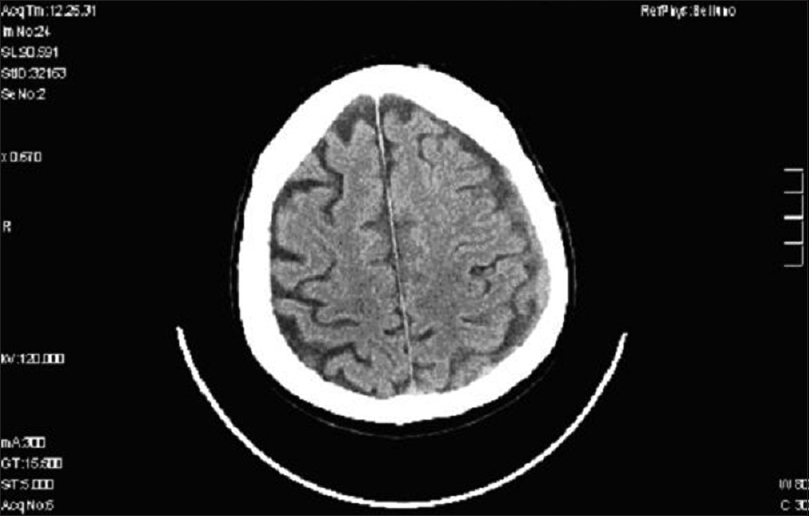
Trigeminal neuralgia, facial pain, and headache represent the most frequent symptoms complained in the emergency room. Physicians are required to solve all the secondary causes of a headache prior to express a correct diagnosis of primary headaches. Here, we report the clinical case of a patient describing symptoms appealing for the first branch of trigeminal neuralgia with little evolution, but the final cause was actually a subdural hematoma. A 69-year-old man with the previous history of hypertension and cardiac arrhythmia was admitted in the emergency department complaining of paroxysmal pain about 20 days characterized by the sensation of electric shocks arising from the left frontal-temporal region with subsequent spread to the ipsilateral maxillary area. These episodes were presented in clusters very painful, several times during the day in almost cases with the same clinical features. He also reported a subjective feeling of imbalance. Rather than avoid contact and touch of the painful area, he applied with the hand an external pressure, an attitude more characteristic of a migraine attack than a classical trigeminal neuralgia. There was no history of trauma nor dental diseases. The patient had never experienced such episodes in the past. Common analgesic with FANS resulted unremarkably. The general and neurological examination, including a detailed cranial nerve test, were completely normal. Brain computed tomography (CT) showed in the left frontal-parietal area the presence of a subdural hematoma whose dimensions were about two centimeters with hyperdense components in the context of recent bleeding, significant flattening of the grooves adjacent cortical, with an initial compressive effect on the ventricular system and minimal midline shift (about 4 mm) to the right [Figure 1]. The patient could not undergo brain magnetic resonance imaging (MRI) because he had a cardiac pacemaker implanted. After neurosurgery evaluation, he was treated with 75 mg/die of oral prednisone for 30 days. The patient benefited from the proposed treatment, and the brain CT performed 1 month later showed the disappearance of the hematoma [Figure 2]. Six months later the patient was asymptomatic and drug-free.

- Noncontrast computed tomography head revealing a hypodense collection of 1.5 cm thickness in the left fronto-temporoparietal region with areas of hyperdensity in the parietal region, suggestive of a predominant chronic subdural hematoma with an acute component. Significant mass effect resulting in compression of the ipsilateral lateral ventricle and midline shift of 4 mm to the right side was noted
- Computed tomography of the brain reveals complete resolution of the left frontoparietal subdural hematoma after 1 month. Computed tomography images shows reexpansion of brain parenchyma without any residual/recurrent subdural hematoma
According to the international classification of a headache, classical trigeminal neuralgia usually starts in the second or third divisions, only in <5% of patients the first division is affected. Between paroxysms, the patient is usually asymptomatic but a dull background pain may persist in some long-standing cases. Following a painful paroxysm, there is usually a refractory period during which pain cannot be triggered. Pain may evoke spasm of the face muscle on the affected side (tic douloureux). The increasing frequency of posterior fossa exploration and MRI has demonstrated that many, possibly most, patients with this condition have compression of the trigeminal root by tortuous or aberrant vessels. Classical trigeminal neuralgia is usually responsive, at least initially, to pharmacotherapy.[1] In symptomatic trigeminal neuralgia pain may be indistinguishable from classical trigeminal neuralgia, but it is caused by a demonstrable structural lesion other than vascular compression. Attacks are usually stereotyped in the individual patient. There may be sensory impairment in the distribution of the appropriate trigeminal division. In most cases, the trigeminal nerve root demyelination involves the proximal part of the root and results from compression by an overlying artery or vein. Other causes of trigeminal neuralgia in which demyelination are involved or implicated include multiple sclerosis and probably compressive space-occupying masses in the posterior region.[2] There is convincing evidence that the idiopathic form develops from focal demyelination at the trigeminal root entry zone with subsequent ephaptic cross-talk between axons,[3] much the most common cause of trigeminal neuralgia is focal compression of the trigeminal nerve root, close to its point of entry into the pons, by an aberrant loop of artery or vein.[1] Most cases are caused by compression of the trigeminal nerve root, usually within a few millimeters of entry into the pons, in a few cases, trigeminal neuralgia is due to a primary demyelinating disorder; other rare causes include infiltration of the nerve root, gasserian ganglion or nerve by a tumor or amyloid and small infarcts or angiomas in the pons or medulla.[4] Causes can also include dolichoectasia of basilar and vertebral arteries[5] venous hemangioma of the mandibular division of the trigeminal nerve,[6] lipomatosis of the trigeminal nerve,[7] Wallenberg's syndrome.[8]
Symptomatic trigeminal neuralgia demonstrates no refractory period after a paroxysm, unlike c lassical trigeminal neuralgia.[1] Various forms of a migraine and neurovascular headaches symptomatic of vascular malformations of the brainstem strengthen the hypothesis of the role of the trigemino-cervical system in the pathophysiology of a migraine.[9] Are also reported rare cases of trigeminal neuropathy secondary to pontine hemorrhage whose clinical phenotype was trigeminal hypoesthesia, precisely as we would expect in a symptomatic neuropathy.[10] Our subject had instead paroxysmal symptoms rather similar to that occurring in classical trigeminal neuralgia even if stereotyped and without pain-free intervals and moreover localized in the first branch of the trigeminal nerve. In literature have reported cases of secondary trigeminal neuralgia involving the second and third branch of the trigeminal nerve due to a lesion in the posterior fossa, but there are no reports of involvement of the first branch of the nerve with a lesion outside the posterior fossa. Subdural hematoma is not in fact a common cause of secondary trigeminal neuralgia. It is certainly intriguing that the patient has complained for the first time neuralgic symptoms in association with this finding. Symptomatology complained was very similar to idiopathic trigeminal neuralgia, the relevant data in retrospect, was the persistent subjective imbalance, with no significant signs in neurological examination and the attitude of slightly pressure on the region involved, as likely to seek relief from the pain, just the opposite characteristic of a common idiopathic trigeminal neuralgia. The nature of paroxysmal pain can be explained by the fact that the bleeding was localized in the rostral portion of the brain, so probably a direct damage of the trigeminal nerve fibers there was not, but rather an irritation of trigeminal fibers, perhaps secondarily activated from meningeal irritation. The lesson we learned is that physicians need to look carefully all the symptoms, even those seemingly meaningless and even without a without a corresponding neurological examination that can address a diagnosis of secondary headache.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgia, and facial pain. The international classification of headache disorders. Cephalalgia. 2004;4(Suppl 1):9-160.
- [Google Scholar]
- Central demyelination of the V th nerve root in trigeminal neuralgia associated with vascular compression. Brain Pathol. 1998;8:1-11.
- [Google Scholar]
- Trigeminal neuralgia: Historical notes and current concepts. Neurologist. 2009;15:87-94.
- [Google Scholar]
- Dolichoectasia of the intracranial arteries. Curr Treat Options Cardiovasc Med. 2011;13:261-7.
- [Google Scholar]
- Venous haemangioma of the mandibular division of the trigeminal nerve. J Laryngol Otol. 2011;28:1-2.
- [Google Scholar]
- Lipomatosis of the trigeminal nerve causing trigeminal neuralgia: Case report and literature review. Skull Base. 2010;20:293-9.
- [Google Scholar]
- Wallenberg's syndrome and symptomatic trigeminal neuralgia. J Headache Pain. 2011;12:377-80.
- [Google Scholar]
- Neurovascular headache and a midbrain vascular malformation: Evidence for a role of the brainstem in chronic migraine. Cephalalgia. 2002;22:107-11.
- [Google Scholar]
- Pontine hemorrhages presenting as trigeminal neuropathy – report of three cases. Neurol Med Chir (Tokyo). 1993;33:234-7.
- [Google Scholar]





