Translate this page into:
Subarachnoid Hemorrhage Due to Ruptured Intracranial Aneurysm Arising from a Vertebral Artery-Bihemispheric Posterior Inferior Cerebellar Artery Bifurcation
Address for correspondence: Dr. Hiroshi Kashimura, Department of Neurosurgery, Iwate Prefectural Chubu Hospital, 17-10 Murasakino, Kitakami, Iwate 024-8507, Japan. E-mail: h-kashimura@pref.iwate.jp
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Although the anatomy of the posterior inferior cerebellar artery (PICA) is highly variable, a solitary PICA supplying both hemispheres of the cerebellum is rare. A 76-year-old woman presented with severe headache and subsequent loss of consciousness and was admitted to our hospital. Initial computed tomography showed subarachnoid hemorrhage. Three-dimensional digital subtraction angiography revealed a saccular aneurysm arising from the right vertebral artery (VA)-PICA bifurcation. The PICA branching from the right VA was enlarged, tortuous, and crossed the midline to supply both cerebellar hemispheres. This right PICA was interpreted as a bihemispheric PICA. Recognizing this variant preoperatively could help prevent complications of surgery. Careful follow-up studies are necessary in cases with bihemispheric PICA to monitor for the development of aneurysm at the junction between the bihemispheric PICA and the VA or the distal portion of the bihemispheric PICA.
Keywords
Aneurysm
bihemispheric posterior inferior cerebellar artery
subarachnoid hemorrhage
variant
INTRODUCTION
The anatomy of the posterior inferior cerebellar artery (PICA) is highly variable. Variant anatomies of the artery include agenesis/hypoplasia, double or duplicated origins, and extracranial or epidural origins.[12] However, a solitary PICA supplying both hemispheres of the cerebellum is rare.[3456] We describe herein a rare case of a ruptured aneurysm arising from the bifurcation of the vertebral artery (VA) and a bihemispheric PICA.
CASE REPORT
A 76-year-old woman presented with severe headache and subsequent loss of consciousness and was admitted to our hospital. No focal neurological abnormality was noted. Initial computed tomography showed subarachnoid hemorrhage, predominantly in the right side of the posterior fossa. Three-dimensional digital subtraction angiography revealed an enlarged, tortuous right PICA that crossed the midline to supply both cerebellar hemispheres and a small saccular aneurysm arising from the right VA-PICA bifurcation [Figure 1a and b]. Right PICA branch proximal to the choroidal point gave rise to ipsilateral vermian branches and hemispheric branches, and a branch distal to the choroidal point gave rise to contralateral vermian branches and hemispheric branches [Figure 1c and d]. Left VA angiography revealed agenesis of the left PICA with no opacification of the corresponding cerebellar territory. The right PICA was interpreted as a bihemispheric PICA.

- (a) Preoperative three-dimensional digital subtraction angiogram, posteroanterior view, showing an enlarged and tortuous right PICA (dotted white arrow) crossing the midline to supply both cerebellar hemispheres (white arrowheads). (b) Three-dimensional digital subtraction angiogram, oblique view, showing a small saccular aneurysm arising from the right VA-PICA bifurcation (red arrow). (c) Three-dimensional digital subtraction angiogram, superoinferior view, showing the arterial course of a cortical branch originating from the right PICA (white arrow). (d) Three-dimensional digital subtraction angiogram, oblique view, showing a large branch distal to the choroidal point (white arrow), which gives rise to the ipsilateral vermian branch (*) and then crosses the midline. The artery crossing the midline gives rise to the contralateral vermian (‡) and hemispheric branches (††). BA: Basilar artery, L: Left, PICA: Posterior inferior cerebellar artery, R: Right, VA: Vertebral artery, †: Right hemispheric branch of the bihemispheric PICA, ††: Left hemispheric branch of the bihemispheric PICA
Far lateral suboccipital craniectomy craniotomy was performed inferiorly to include the foramen magnum. The arch of the C1 vertebra was removed from just beyond the midline on the opposite side. The aneurysm was successfully obliterated by clipping with a slightly curved Yasargil titanium mini clip: No. FT712T [Figure 2]. Complete aneurysm occlusion and patency of the right PICA were confirmed intraoperatively by indocyanine green angiography. The postoperative course was uneventful, and the patient was discharged with no neurological deficits.
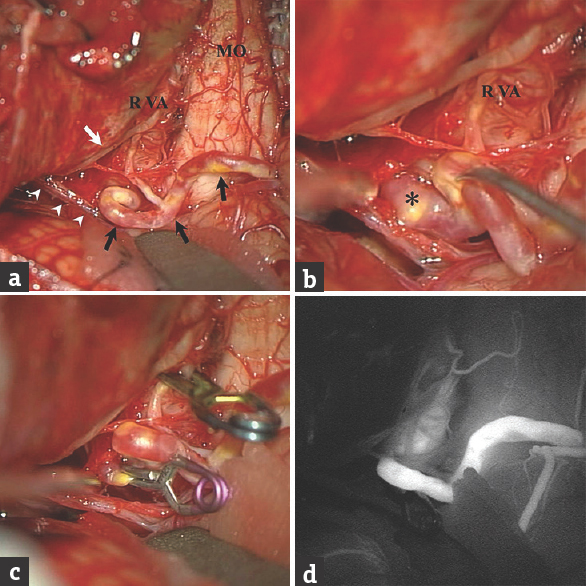
- (a and b) Intraoperative photographs showing an enlarged and tortuous right posterior inferior cerebellar artery (black arrows) and its relationship to the ipsilateral cerebellum, vertebral artery, lower cranial nerves (white arrow: cranial nerve XI; white arrowheads: cranial nerves IX and X), medulla oblongata, and aneurysm (*). (c) The aneurysm is occluded by a slightly curved Yasargil titanium mini clip (No. FT712T) following temporary occlusion of the right vertebral artery by a temporary clip. (d) Intraoperative indocyanine green angiogram showing patency of the right PICA. MO: Medulla oblongata, VA: Vertebral artery, R: Right
DISCUSSION
Although the anatomy of the PICA is highly variable, a bihemispheric PICA is rare.[3456] When one PICA is hypo- or a-plastic, the PICA territory is typically supplied by an enlarged ipsilateral anterior inferior cerebellar artery or superior cerebellar artery.[4] In rare cases, a solitary PICA can supply both hemispheres of the cerebellum as a bihemispheric PICA. This variant is further subcategorized into true bihemispheric PICA, serving the contralateral PICA territory, and the vermian variant, serving only the midline. With the true bihemispheric variant, aplasia of the contralateral PICA should be evident although the contralateral PICA may be present with the vermian variant.[34] Bihemispheric PICA has not been well described in the radiologic literature. Several case reports have identified bilateral cerebellar infarcts that have been ascribed to a bilateral PICA supply.[78] Among previous reports, relatively large series of four and eleven incidental cases were described by Cullen et al. and Carlson et al.[34] The incidences of bihemispheric PICA were reported in those studies as 0.1% and 3.6%, respectively.[34]
Carlson et al. reported that this anomalous artery results in a predisposition toward the formation of aneurysms.[3] Several cases of ruptured aneurysm have been reported arising from a communicating branch between bilateral distal PICAs, as the so-called PICA communicating artery.[910] This terminology may not be accurate as the communication is not a normal anastomosis and in the reported cases there was typically aplasia or hypoplasia of the contralateral PICA suggesting that there was in fact a bihemispheric PICA.[3] In the present case, the anomalous artery was interpreted as a bihemispheric PICA because of the characteristic findings on angiography. The ruptured aneurysm arose from the bifurcation of the VA and the bihemispheric PICA. Only one other report has described an aneurysm located at the origin of a bihemispheric PICA.[5]
The pathogenesis of associated aneurysms has not been fully clarified. Mechanisms contributing to aneurysm formation may involve either increased local hemodynamic forces resulting from the bihemispheric PICA or structural weakness of the arterial wall. Structural anomalies, such as persistent primitive artery, azygos anterior cerebral artery, hyperplastic anterior choroidal artery, and fenestration of the intracranial arteries, show higher rates of aneurysm formation than other vessels. Careful follow-up studies are thus necessary in cases of bihemispheric PICA to monitor for the development of aneurysm at the junction between the bihemispheric PICA and the VA or the distal portion of the bihemispheric PICA. When treating this aneurysm, it is critical to prevent the patency of the bihemispheric PICA. Recognizing and reporting this variant could be helpful in preventing complications of surgery. Although injury to the bihemispheric PICA itself is unlikely to result in clinical deficits, precise knowledge of the vascular anatomy, including such variants, is essential to help minimize complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The lateral spinal artery of the upper cervical spinal cord. Anatomy, normal variations, and angiographic aspects. J Neurosurg. 1985;63:235-41.
- [Google Scholar]
- Double origin of the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2004;25:425-7.
- [Google Scholar]
- The bihemispheric posterior inferior cerebral artery: Anatomic variations and clinical relevance in 11 cases. J Neurointerv Surg. 2013;5:601-4.
- [Google Scholar]
- The bihemispheric posterior inferior cerebellar artery. Neuroradiology. 2005;47:809-12.
- [Google Scholar]
- Posterior inferior cerebellar artery (PICA) aneurysm arising from a bihemispheric PICA. Clin Neuroradiol. 2006;16:190-1.
- [Google Scholar]
- Bihemispheric posterior inferior cerebellar artery occurring with an azygos anterior cerebral artery: Case study. Case Rep Radiol 2014 2014:541081.
- [Google Scholar]
- Bilateral cerebellar infarctions caused by a stenosis of a congenitally unpaired posterior inferior cerebellar artery. J Neuroimaging. 2001;11:435-7.
- [Google Scholar]
- Acute bilateral cerebellar infarction in the territory of the medial branches of posterior inferior cerebellar arteries. Stroke. 1994;25:686-8.
- [Google Scholar]
- Ruptured aneurysm at the cortical segment of the posterior inferior cerebellar artery. J Clin Neurosci. 2006;13:777-81.
- [Google Scholar]






