Translate this page into:
Subacute left hemispheric subdural hematoma associated with symptomatic contralateral hygroma
*Corresponding author: Boris Gbassara Koulagna, Department of Surgery, Faculty of Health Sciences, University of Nairobi, Nairobi, Kenya. gbassara1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ousmanou Djoubairou B, Gbassara Koulagna B, Agbéko Komlan Doléagbénou A, Djientcheu V. Subacute left hemispheric subdural hematoma associated with symptomatic contralateral hygroma. J Neurosci Rural Pract. doi: 10.25259/JNRP_12_2025
Abstract
Subacute subdural hematoma associated with contralateral post-traumatic hygroma is a rare condition, especially in young patients without coagulopathy or anticoagulant use. This case report presents a 25-year-old female with a history of mild traumatic brain injury leading to left hemispheric subacute subdural hematoma and symptomatic contralateral hygroma. The report discusses the pathophysiology, including potential mechanisms such as bridging vein rupture and impaired brain expansion, risk factors, and management approaches. Surgical intervention for the subdural hematoma and contralateral hygroma resulted in rapid symptomatic relief with favorable clinical outcomes. This case highlights the importance of individualized management strategies and calls for further studies to standardize treatment guidelines for similar presentations.
Keywords
Case report
Post-traumatic hygroma
Subacute subdural hematoma
Traumatic brain injury
Young patient case
INTRODUCTION
Chronic subdural hematoma (CSDH) is a collection of blood encapsulated by neo-membranes in the subdural space.[1] It is commonly observed in elderly patients. Post-traumatic subdural hygroma (PTSH) refers to an accumulation of cerebrospinal fluid in the subdural space due to arachnoid membrane rupture, with a reported prevalence of 4–6% following traumatic brain injury.[2] Several studies have documented the progression of PTSH to CSDH in elderly patients.[2-6] The pathophysiology of this transformation remains debated. One hypothesis suggests that bridging vein bleeding within the hygroma triggers the proliferation of inflammatory cells, leading to fibroblast layer development along the dura mater, perpetuating subdural bleeding.[7] Bilateral post-traumatic hygromas are a significant risk factor for CSDH development. The occurrence of a post-traumatic subacute subdural hematoma in a young patient associated with a symptomatic contralateral hygroma is rare. We discuss the pathophysiology, risk factors, and management strategies in this case.
CASE REPORT
A 25-year-old female patient presented with a history of a sports-related head injury (ball impact), 3 weeks before, resulting in a cranial impact point and transient loss of consciousness. She reported 1 week of headaches and right-sided diplopia. Brain magnetic resonance imaging revealed a peri-cerebral fluid collection in the left hemisphere, exhibiting T1 and T2 hyperintensity and fluid-attenuated inversion recovery (FLAIR) hyperintensity, diffusion hypointensity with moderate apparent diffusion coefficient (ADC) restriction, T2* hypointensity, and no contrast enhancement. The collection measured 15 mm thick, causing cortical sulcal effacement, consistent with a subacute left hemispheric subdural hematoma. In addition, a peri-cerebral fluid collection in the right hemisphere demonstrated T1 hypointensity, FLAIR, and diffusion hypointensity without ADC restriction, T2 hyperintensity, and no contrast enhancement, without hemorrhagic stigmas on T2*. This right-sided collection, measuring 11 mm in thickness and causing cortical sulcal effacement, was consistent with a hygroma [Figure 1]. The surgical intervention involved trephination with two burr holes on the left side, resulting in the evacuation of lysed blood under pressure and irrigation until the fluid cleared. The dura mater opening on the right released cerebrospinal fluid under high pressure, followed by skin. The patient exhibited significant clinical improvement, with the resolution of headaches and diplopia within 72 h. At 1-month follow-up, she reported complete symptom resolution, and a non-contrast brain computed tomography (CT) scan appeared normal [Figure 2].
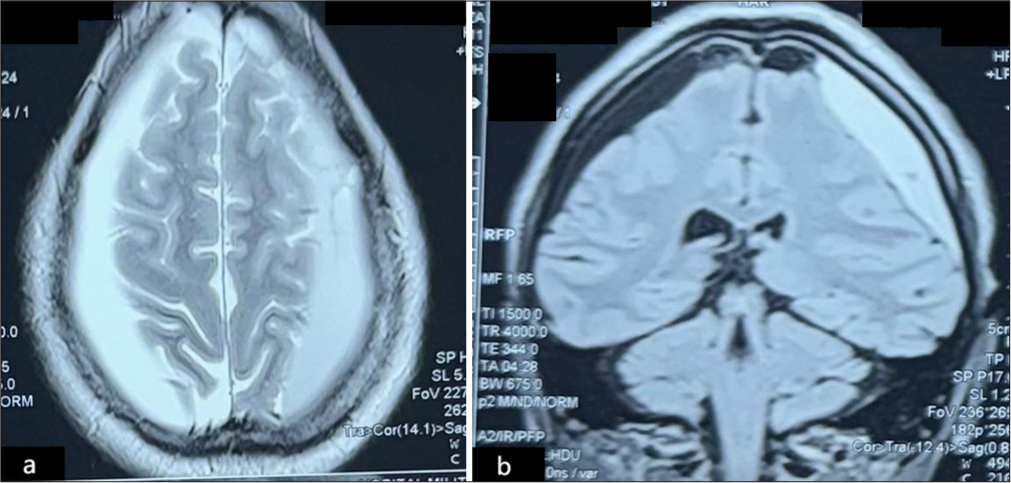
- Initial brain magnetic resonance imaging performed three weeks after trauma. (a) Axial section showing a left subacute subdural hematoma with T2 hyperintensity and mass effect, associated with a right hemispheric hygroma. (b) Coronal section showing the same lesions (left subdural hematoma and right hygroma).
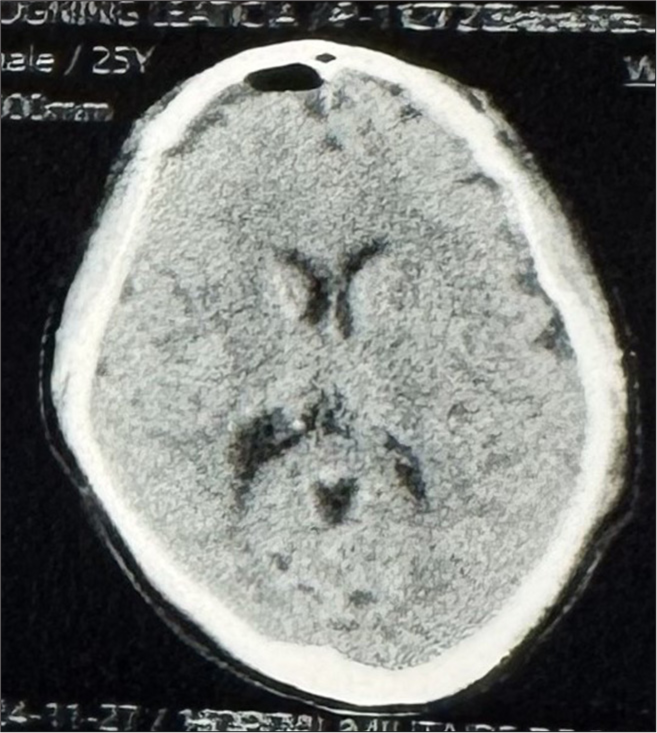
- Non-contrast brain computed tomography scan at 1-month postoperative follow-up showing complete resolution of the subdural collections.
DISCUSSION
Pathophysiology
The traumatic brain injury likely caused an acute left subdural hematoma and contralateral arachnoid membrane rupture, resulting in post-traumatic hemispheric hygroma. Chronicity of the acute hematoma, marked by red blood cell degradation, was observed at the 3-week presentation. The presence of fibrous membranes and fibroblastic layer development along the dura mater perpetuated recurrent bleeding.[7]
An alternative theory suggests bilateral post-traumatic hygroma formation following the traumatic event. Ahn et al. reported bilateral hygroma as a major risk factor for CSDH development.[4] The left bridging vein rupture could have facilitated the transformation of a bilateral hygroma into a left subacute subdural hematoma.
A third hypothesis posits that persistent bilateral subdural hygroma led to impaired brain expansion, favoring CSDH formation. The patient’s symptoms, including headaches and right diplopia, were attributable to elevated intracranial pressure, necessitating surgical intervention.
Another important consideration is the possibility that the patient had two distinct pathologies, a pre-existing, asymptomatic subdural hygroma from an earlier, unreported minor trauma and a left subdural hematoma related to the ball impact. This hygroma may have remained clinically silent until the recent ball impact caused an acute rise in intracranial pressure, leading to the onset of symptoms. This mechanism could explain the delayed manifestation of the contralateral hygroma, reinforcing the need for thorough clinical history-taking in similar cases.
In addition, the nature of the trauma itself should be analyzed. A localized impact from a ball is more likely to cause a focal brain injury rather than a widespread traumatic effect, which is more common in high-impact coup-contrecoup injuries or diffuse axonal injuries seen in severe head trauma. This difference in injury dynamics may have played a role in the asymmetric presentation observed in this case.
Risk factors
Mild-to-moderate traumatic brain injury is a risk factor for CSDH and hygroma formation.[2,4]
Age ≥70 years, particularly in males, is a major risk factor for CSDH and post-traumatic hygroma.[2,4,6] However, our case contrasts these findings, as the patient was a 25-year-old female with no coagulopathy or anticoagulant use history.
Recent studies have identified CT scan imaging-based risk factors for hygroma transformation into CSDH: Hygroma size ≥11 mm and density ≥11 HU.[6]
Management approach
The management of subacute subdural hematoma (clinical or radiological signs of raised intracranial pressure, size ≥10 mm, cortical sulcal effacement, or midline shift ≥5 mm)[7] associated with a small contralateral hygroma (≤10 mm) involves hematoma evacuation (burr holes, endoscopy, twist drill) and conservative treatment of the hygroma. Immediate postoperative imaging and clinical monitoring, followed by a 1-month follow-up, are recommended. The potential postoperative hygroma enlargement due to brain expansion and cortical vein stretching raises the issue of preventive surgery for small contralateral hygroma. Multicenter prospective studies on large cohorts are needed to standardize this management approach.
CONCLUSION
Chronic or subacute subdural hematoma associated with post-traumatic contralateral hygroma is rare. Pathophysiological mechanisms remain controversial, and the average age of occurrence is ≥60 years. However, this association can occur in young individuals without coagulopathy or anticoagulant use. Surgical treatment is indicated in cases of clinical and radiological signs of raised intracranial pressure.
Acknowledgment:
The authors would like to express their gratitude to all individuals and organizations who provided support for the successful completion of this work. We acknowledge the contributions of the surgical and nursing teams involved in the patient’s care and the radiology department for their assistance with imaging and diagnostic evaluations. Special thanks are extended to our colleagues for their constructive feedback and insightful discussions during the preparation of this manuscript.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Treatment of patients with traumatic subdural effusion and concomitant hydrocephalus. J Neurosurg. 2012;116:558-65.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with subdural hygroma following mild traumatic brain injury. Korean J Neurotrauma. 2022;18:230-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic subdural hematoma secondary to traumatic hygroma: Consequence or coexistence? In: Recent advances in neurotraumatology. Tokyo: Springer; 1993. p. :88-90.
- [CrossRef] [Google Scholar]
- Analysis of risk factors for the development of chronic subdural hematoma in patients with traumatic subdural hygroma. J Korean Neurosurg Soc. 2016;59:622-7.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic treatment of chronic subdural hematoma combined with inner subdural hygroma. J Korean Neurosurg Soc. 2023;66:552-61.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic subdural hygroma and chronic subdural hematoma: A systematic review and meta-analysis. J Clin Neurosci. 2023;107:23-33.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic subdural hematoma: Modern management and emerging therapies. Nat Rev Neurol. 2014;10:570-8.
- [CrossRef] [PubMed] [Google Scholar]







