Translate this page into:
Study of Sleep Disorders among Young Children Using Hindi Translated and Validated Version of Pediatric Sleep Questionnaire
Address for correspondence: Dr. Ravi Gupta, Department of Psychiatry and Sleep Clinic, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Jolly Grant, Dehradun - 248 016, Uttarakhand, India. E-mail: sleepdoc.ravi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The objective of this study is to assess the prevalence of sleep disorders among children aging between 4 and 9 years using Hindi version of Pediatric Sleep Questionnaire (PSQ).
Methods:
This study had two parts first, translation and validation of PSQ into Hindi language, and second, assessment of the prevalence of sleep disorders using PSQ Hindi version. Hindi PSQ was distributed in randomly chosen primary schools in a semi-urban area. The children were requested to get them filled by their parents. When the questionnaires were returned, responses were analyzed.
Results:
Most of the items of the Hindi version had perfect agreement with original questionnaire in a bilingual population (κ =1). Totally, 435 children were included in the field study having average age of 6.3 years. Obstructive sleep apnea was reported in 7.5% children; symptoms suggestive of restless legs syndrome were reported by 2%–3%; teeth grinding by 13.9% and sleep talking by 22.6% children.
Conclusion:
PSQ Hindi version is a validated tool to screen for sleep disorders among children. Sleep disorders are fairly prevalent among young children in India.
Keywords
Child
obstructive sleep apnea
restless legs syndrome
sleep-wake disorders
INTRODUCTION
Sleep disorders are not uncommon among school children, and it has been found the primary school children suffer from various sleep disorders, for example, difficulty falling asleep, restless sleep, teeth grinding, and daytime sleepiness.[1] Cultural and geographical differences have been observed in the prevalence of sleep disorders, sleep schedule, and the reasons that lead to daytime sleepiness among children.[1] Although the sleep disorders are common, still it has been found that many a times, parents remain oblivious of their child's sleep problems.[2] It has been reported that children from the Asian countries sleepless as compared to Western countries.[13] Sleep deprivation has also been reported among children, especially with relation to the homework schedule.[45] Diagnosis of sleep disorders and sleep deprivation is important in children as they have been found to be associated with daytime napping, cardiovascular morbidity, attention deficit hyperactivity disorder (ADHD), and obesity.[678]
Indian data using the sleep questionnaires suggests that around 13% of toddlers have sleep problems, most common being the night awakenings.[9] Another study reported that among 3–10 years old children, 43% had some kind of sleep disorder.[10] The most common disorder has been the nocturnal enuresis followed by sleep talking and bruxism.
A number of questionnaires have been developed to assess sleep disorders in children. These include Children Report of Sleep Habits (CRSH),[2] Children's Sleep Habits Questionnaire (CSHQ),[11] and Pediatric Sleep Questionnaire (PSQ).[12] Among these, CRSH is the self-reporting questionnaire, while the latter two are to be responded by the parents. A review of various sleep questionnaires has reported that PSQ-sleep disordered breathing subscale is a validated tool and possess' all psychometric properties. Of all the questionnaires, CSHQ has already been translated in Hindi.[13] However, CSHQ does not provide any diagnosis. Hence, the objective of this study was to assess sleep disorders among children falling in the age group of 4–9 years, especially the obstructive sleep apnea (OSA) using Hindi translation of PSQ.
METHODS
This study was done after obtaining permission from the Institutional Ethics Committee. It had two parts first, the translation of PSQ in Hindi and second, assessment of sleep disorders in children using the Hindi version.
Translation of Pediatric Sleep Questionnaire
This questionnaire was developed by Chervin et al.[14] It has 69 items that address various issues related to child's sleep that range from sleep onset difficulty, insomnia, restless legs syndrome (RLS), snoring, excessive daytime sleepiness, parasomnias, and daytime behavioral symptoms of hyperactivity and inattention. Most of the items are to be scored on three points-yes/no or do not know by the parents.
One of its subscales for sleep related breathing disorder (SRBD) has been validated for the diagnosis of sleep apnea.[12] The 22-item SRBD subscale has been found to correctly classify 85% cases with sensitivity of 85% and specificity of 87%. This scale has been translated into many languages including Malay, Spanish, Portuguese, and Turkish.[15161718]
The translation of the questionnaire was done according to the standard guidelines. After obtaining the permission from the author of original instrument, original English version was procured (V0). Then, two bilingual translators translated it into Hindi independently (V1 and V2). Both the Hindi versions were compared with each other, and a common Hindi version was reached (V3). This was back-translated into English by two independent English translators (V4 and V5). A common English version was framed after discussion regarding the terminologies (V6). This was compared with the original version (V0) for the gross inconsistencies by the team if any. Wherever gross technical inconsistencies were found, appropriate changes were made in V3, and another Hindi version V7 was reached. This was tested in a small set of parents (n = 7) who had children falling between 3 and 12 years for the ease of understanding. They were asked to provide information regarding sleep of their children and also to report any difficulty in understanding the questionnaire. If they suggested any difficulty in understanding any item/word, it was discussed with them, and necessary changes in terminology were made, wherever required. This leads to a Hindi version that was then considered as a final version-V8.
Finalized Hindi version (V8) was tested in a small set of bilingual parents (22 in number). First, they were asked to provide information regarding sleep of their child according to final Hindi version (V8). After 5 days, they were given the original English version of the questionnaire. Responses from both the versions were correlated for the concordance.
Assessment of prevalence of sleep disorders
This study was conducted in the primary schools of the semi-urban area. List of schools located in the area was prepared, and from this list, schools were selected randomly. One of the authors reached the school authorities and explained them the rationale of the study. After obtaining permission from the competent authority, they were delivered the validated Hindi version of PSQ. This was distributed in the classes starting from lower kindergarten to Class IV, i.e., the children falling in the age group of 4–9 years. They were asked to get it filled by their parents.
With each questionnaire, a page for obtaining parent's informed consent was attached that was to be signed by the parents. Parents were given 5 days to return the completed questionnaire. Completed questionnaires were collected from school and data were analyzed.
Anthropometric measurements were obtained from the school records.
Statistical analysis
Statistical analysis was done using SPSS version 22.0 (Released 2013. IBM SPSS Statistics for Windows, version 22.0. IBM Corp., Armonk, NY, USA). For the validation of the PSQ, kappa was calculated for each item comparing the agreement between English and Hindi version. For the data gathered from the school children, descriptive statistics was calculated.
RESULTS
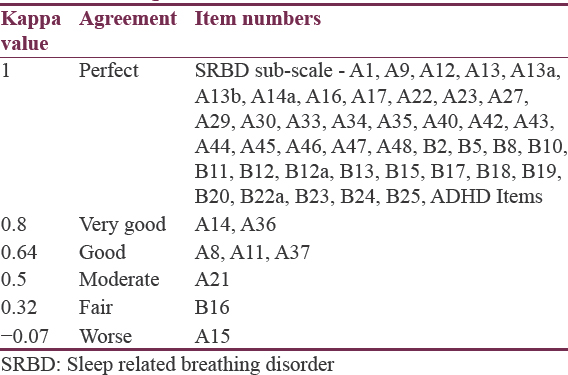
Translation process of the scale in Hindi was made difficult by various cultural issues. In Hindi, we did not have expression for some of the phrases mentioned in original English version. For example, original version mentions “growing pains” in item numbers A13a and A13b. Since this did not have adequate translation in Hindi, after the consensus, another term which is given in original instrument “unexplained leg pains” was used, and it was translated as “akaaran dard.” Other terminologies where the alternate terminologies were used are depicted in Table 1. The kappa suggested a perfect agreement for most of the items of the scale [Table 2]. Item A15 had worst agreement, and hence, it was revised in the Hindi translation after consultation with participants.

A total of 560 forms were distributed; out of which, 482 were returned (response rate = 86%). Out of these 482 forms, 47 forms had missing responses on 5 or more items, hence, they were excluded from the study. Thus, in the final analysis, 435 forms were included in the study.
The average age of subjects included in this study was 6.36 ± 1.61 years. This sample was dominated by girls (60.64%). Mean sleep latency in this group was 11.69 ± 9.14 min. None of the forms that were returned disclosed any medical condition among any of the participants.
4.14% children had difficult bedtime routine. Difficulty in falling asleep was reported in 1.93% children. Two or more awakenings in the night were reported in 3.01% children, and 1.94% had difficulty in falling asleep again. Early morning awakening was reported in 3.43% children. 6.38% children complained of nonrefreshing sleep, and napping was reported in 30.34% children. 30.34% children consumed caffeine during the day. Frequent change in bedtime was reported in 5.49% and a frequent change in wake time was observed by parents of 4.95% children. Table 3 depicts prevalence of various sleep disorders and their symptoms.
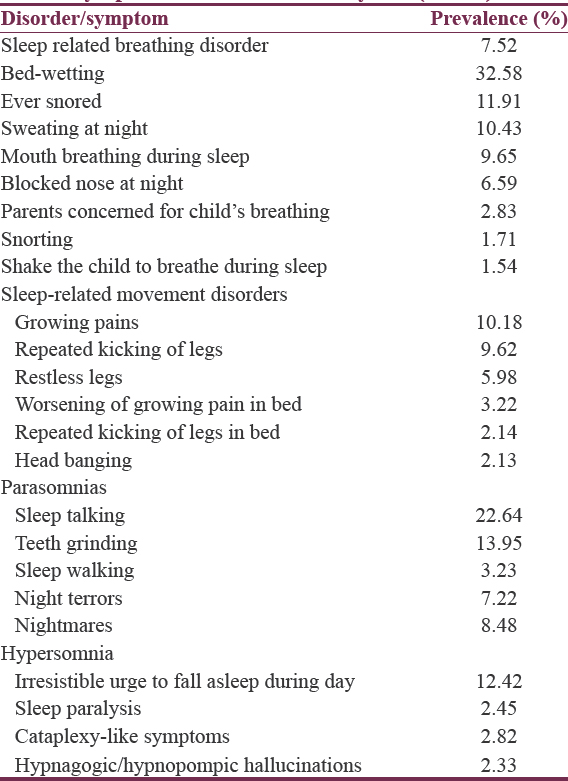
DISCUSSION
This study suggested that sleep disorders are not uncommon in young school children. SRBD was reported in approximately 8% children, and at least, one out of three children was wetting the bed. “Restless legs” and “growing pains” were reported in 6% and 10% children, respectively. Among parasomnias, teeth grinding was most common, reported in 14% children. Hypersomnia and caffeine consumption was also common among young children. Thus, this study underlines the need for focusing our attention to the sleep of children.
Earlier studies have reported that sleep disorders are not uncommon among school children. At the age of 4 years, 19% children have been found to suffer from sleep disorders with insomnia being the most prevalent of all, reported in 17% of the subjects.[19] Another study has reported that insomnia and nightmares were the most prevalent sleep disorder among children who have just joined the school, having reported by 15% and 14% study sample.[20] An Indian study involving children falling between 1 and 3 years suggested that 81% had 1–3 awakenings at night and 13% were suffering from various sleep disorders.[9] Our results are more or less comparable with the data from other studies except the snoring, which has been reported by small group in the present study. Earlier it has been found that around 39% children snore with 4% having habitual snoring.[21] That study reported that habitual snoring was associated with restless sleep, witnessed pauses in breath during sleep and mouth breathing, and hyperactivity during the daytime.[21] Furthermore, sleep disorders and poor sleep have been found to impair academic performance and to produce symptoms similar to ADHD.[212223] Thus, sleep-related symptoms should not be ignored among children.
We found that sleep-related parents of 8% children reported SRBD-OSA. Adenotonsillar hypertrophy and obesity are the important predictors of OSA among children, and most of the time they are coexistent.[24] In addition to mimicking ADHD, OSA has been found to have multiple metabolic and cardiovascular complications among children. Studies have reported that OSA among children leads to lipid peroxidation;[25] increment of proinflammatory markers in body, for example, interleukin 6, interleukin 18, plasminogen activating factor, high-sensitivity-C reactive protein;[2627] insulin resistance;[28] endothelial dysfunction;[29] and an increase in blood pressure.[30] However, resolution of OSA by adenotonsillectomy or any other method has been reported to improve all consequences of OSA among children including ADHD and systemic inflammation.[26293031] Considering the high prevalence of OSA in this study among Indian children and multiple adverse consequences which are reversible, there is a need for improving the awareness among pediatricians regarding sleep disorders.
Worsening of growing pains at night was reported by parents of 3.22% subjects with repeated kicking in bed by 2.14%. Earlier studies have suggested a RLS has a prevalence of approximately 2% in Chinese children[32] and 3% among Turkish children and adolescents;[33] figures that are close to the prevalence found in this study. However, it should be noted that we did not assess the RLS by face-to-face interview. RLS among children is frequently associated with iron deficiency.[34] In addition, a number of children in this study had growing pains, and growing pains may be initial presentation of RLS among children.[35] Considering the impact of RLS on the daytime performance of children, sleep quality at night and considering the prevalence of iron deficiency in India, it would be worthwhile to assess the children for RLS.[36]
This study had few methodological limitations – first, sample size was small; second, this was a questionnaire-based study, and third, sleep and sleep disorders were not examined using objective measures. However, the strengths of the study lie in the fact that a Hindi translated version of a valid instrument was used that had earlier been found to have good correlation with objective measures.[12] In future, further studies with improved methodology are required to assess the extent of the problem among children and to analyze the effect of sleep disorder on scholastic performance, behavior, and health.
CONCLUSION
This study shows that a significant proportion of children aging between 4 and 9 years suffer from sleep disorders such as SRBD and RLS.
Financial support and sponsorship
We are thankful to Swami Rama Himalayan University extending the financial support for the data collection.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Authors are thankful to University of Michigan Office of technology transfer and Dr. Chervin for allowing us to translate the PSQ in Hindi.
REFERENCES
- Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115(1 Suppl):241-9.
- [Google Scholar]
- The Children's Report of Sleep Patterns (CRSP): A self-report measure of sleep for school-aged children. J Clin Sleep Med. 2013;9:235-45.
- [Google Scholar]
- Sleep behaviour in a sample of preschool children in Singapore. Ann Acad Med Singapore. 2012;41:99-104.
- [Google Scholar]
- Sleep problems among school age children in Chengdu. Sichuan Da Xue Xue Bao Yi Xue Ban. 2008;39:1014-7.
- [Google Scholar]
- Homework schedule: An important factor associated with shorter sleep duration among Chinese school-aged children. Behav Sleep Med. 2014;12:389-97.
- [Google Scholar]
- Sleep duration and overweight in European children: Is the association modified by geographic region? Sleep. 2011;34:885-90.
- [Google Scholar]
- Effects of adenoidectomy/adenotonsillectomy on ADHD symptoms and behavioral problems in children. Int J Pediatr Otorhinolaryngol. 2015;79:1030-3.
- [Google Scholar]
- Obstructive sleep apnea syndrome in children as a risk of cardiovascular pathology development. Vestn Ross Akad Med Nauk. 2015;1:32-40.
- [Google Scholar]
- Sleep habits and sleep problems in healthy preschoolers. Indian J Pediatr. 2015;82:606-11.
- [Google Scholar]
- Patterns and problems of sleep in school going children. Indian Pediatr. 2006;43:35-8.
- [Google Scholar]
- The Children's Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043-51.
- [Google Scholar]
- Pediatric Sleep Questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21-32.
- [Google Scholar]
- Children Sleep Habits Questionnaire (CSHQ): Psychometric validation in Indian school children. Indian J Sleep Med. 2008;3:102-6.
- [Google Scholar]
- Pediatric Sleep Questionnaire: Prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg. 2007;133:216-22.
- [Google Scholar]
- Cross-cultural adaptation and reliability of Pediatric Sleep Questionnaire in assessment of sleep-disordered breathing in the Malay speaking population. World J Pediatr. 2012;8:38-42.
- [Google Scholar]
- Reliability and validity of the Turkish version of the Pediatric Sleep Questionnaire: A tool for prediction of sleep related breathing disorder. Tuberk Toraks. 2011;59:236-41.
- [Google Scholar]
- Spanish version of the Pediatric Sleep Questionnaire (PSQ). A useful instrument in investigation of sleep disturbances in childhood. Reliability analysis. An Pediatr (Barc). 2007;66:121-8.
- [Google Scholar]
- Translation and cross-cultural adaptation of the Pediatric Sleep Questionnaire into Portuguese language. Int J Pediatr Otorhinolaryngol. 2015;79:175-8.
- [Google Scholar]
- Sleep disorders in preschoolers: Prevalence and comorbidity with psychiatric symptoms. J Dev Behav Pediatr. 2013;34:633-41.
- [Google Scholar]
- Prevalence and stress factors of sleep disorders in children starting school. Prax Kinderpsychol Kinderpsychiatr. 2004;53:3-18.
- [Google Scholar]
- Habitual snoring in primary school children: Prevalence and association with sleep-related disorders and school performance. Med Princ Pract. 2009;18:458-65.
- [Google Scholar]
- Sleep-related breathing disorder is associated with hyperactivity in preschoolers. Singapore Med J. 2014;55:257-60.
- [Google Scholar]
- Obstructive sleep apnea mimics attention deficit disorder. J Atten Disord. 2016;20:41-2.
- [Google Scholar]
- The relation between childhood obesity and adenotonsillar hypertrophy. Eur Arch Otorhinolaryngol. 2016;273:505-9.
- [Google Scholar]
- Oxidative stress in children with obstructive sleep apnea syndrome. J Clin Sleep Med. 2014;10:677-81.
- [Google Scholar]
- Effects of adenotonsillectomy on plasma inflammatory biomarkers in obese children with obstructive sleep apnea: A community-based study. Int J Obes (Lond). 2015;39:1094-100.
- [Google Scholar]
- C-reactive protein and carotid intima-media thickness in children with sleep disordered breathing. J Clin Sleep Med. 2013;9:493-8.
- [Google Scholar]
- Metabolic alterations in children with obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2014;78:854-9.
- [Google Scholar]
- Endothelial function in children with OSA and the effects of adenotonsillectomy. Chest. 2015;147:132-9.
- [Google Scholar]
- Long-term changes in blood pressure control in elementary school-aged children with sleep-disordered breathing. Sleep Med. 2014;15:83-90.
- [Google Scholar]
- Attention deficit hyperactivity disorder and sleep disordered breathing in pediatric populations: A meta-analysis. Sleep Med Rev. 2014;18:349-56.
- [Google Scholar]
- An epidemiologic study of restless legs syndrome among Chinese children and adolescents. Neurol Sci. 2015;36:971-6.
- [Google Scholar]
- A prevalence study of restless legs syndrome in Turkish children and adolescents. Sleep Med. 2011;12:315-21.
- [Google Scholar]
- Low body stores of iron and restless legs syndrome: A correctable cause of insomnia in adolescents and teenagers. Sleep Med. 2002;3:127-32.
- [Google Scholar]
- Early manifestations of restless legs syndrome in childhood and adolescence. Sleep Med. 2008;9:770-81.
- [Google Scholar]
- Association between low serum ferritin and restless legs syndrome in patients with attention deficit hyperactivity disorder. Tohoku J Exp Med. 2007;213:269-76.
- [Google Scholar]






