Translate this page into:
Study of psychiatric comorbidity in patients with headache using a short structured clinical interview in a rural neurology clinic in Western India
Address for correspondence: Dr. Soaham Dilip Desai, Consultant Neurologist, Room 119, Ramanbhai Gokal Privilege Centre, Shree Krishna Hospital, Karamsad, Anand, Gujarat, India - 388 325. E-mail: drsoahamdesai@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Psychiatric disorders are common in patients attending neurology clinics with headache. Evaluation of psychiatric comorbidity in patients with headache is often missed in the busy neurology clinics.
Aims:
To assess the prevalence of Axis-I DSM-IV psychiatric disorders in patients with primary headache disorders in a rural-based tertiary neurology clinic in Western India.
Settings and Design
: A cross-sectional observation survey was conducting assessing all patients with migraine, tension-type headache and chronic daily headache attending the Neurology Clinic of Shree Krishna Hospital, a rural medical teaching hospital in Karamsad, in Gujarat in Western India.
Materials and Methods:
A total of 101 consecutive consenting adults with headache were interviewed using Mini International Neuropsychiatric Interview (M.I.N.I.), a structured diagnostic clinical interview to assess prevalence of Axis-I DSM-IV psychiatric disorders.
Statistical Analysis:
Descriptive statistics were calculated using SPSS software version 16 and a binomial regression model was used to study the relationship of psychiatric co-morbidity with patient-related factors.
Results:
49 out of 101 (48.5%) patients with headache suffered from depressive disorders (dysthymia or depression or suicidality), 18 out of 101 patients with headache (17.90%) suffered from anxiety related disorders (generalized anxiety disorder or agoraphobia or social phobia or panic disorder).
Conclusions:
Axis-I psychiatric disorders are a significant comorbidity among patients with headache disorders. M.I.N.I. can be used as a short, less time consuming instrument to assess all patients with headache disorders.
Keywords
Anxiety
depression
headache
migraine
tension-type headache
Introduction
Migraine and tension-type headache (TTH) are most common neurological disorders present in the community and in patients attending the outpatient clinics of hospitals. TTH and migraine rank second and third in prevalence among other diseases in the world.[1] Studies in general population and clinical settings have indicated that there is increased risk of affective and anxiety disorder in individuals with migraine and chronic daily headache as compared to those not suffering from migraine.[23] Recognition and treatment of psychiatric co-morbidity in patients with chronic and recurrent headaches is necessary to improve quality of life, prognosis and reduce the risk of chronicity of the disease. Most of the current available studies have assessed patients using either patient-generated scores like Hamilton Anxiety Scale (HAS) and Hamilton Depression Scale (HAD) that are subjective screening instruments or have used detailed evaluation instruments like the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) and Composite International Diagnostic Interview (CIDI), which are extensively time consuming and difficult to use in the routine general practice. Mini International Neuropsychiatric Interview (M.I.N.I.) is a short, less time consuming, valid and reliable structured clinical interview for Axis-I DSM-IV disorders.[45] There is a paucity of literature from Gujarat and India regarding prevalence of psychiatric co-morbidity in patients with migraine, TTH and CDH. Therefore, we conducted this study to assess the prevalence of Axis-I DSM-IV disorders using M.I.N.I. in patients with headache.
Materials and Methods
A cross-sectional, observational study approved by Institutional Ethics Committee of H. M. Patel Centre for Medical Care and Education was conducted at Shree Krishna Hospital, a rural-based medical teaching hospital associated with Pramukhswami Medical College, located in Karamsad in Gujarat State in Western India, over a period of 60 days between April and June 2012. We recruited a total of 101 consecutive consenting adult (age > 18) patients attending neurology clinic with diagnosis of migraine, TTH and CDH after obtaining informed consent. The diagnosis of headache disorders was made according to International Classification of Headache Disorders [ICHD] 2004.[6] CDH is a descriptive term defined as headaches on 15 or more days in a month for at least 3 months.[7]
We used M.I.N.I. English version 5.0.0 to assess the patients for recognizing psychiatric co-morbidity. M.I.N.I. is a structured diagnostic interview for diagnosis of DSM-IV psychiatric disorders. It was originally developed with the aim of efficient and accurate assessment of DSM-IV psychiatric disorders.[4] Descriptive statistics were calculated using SPSS software version 16 and a binomial regression model was used to study the relationship of psychiatric co-morbidity with various patient related factors such as age, gender, type of headache, duration and frequency of headache.
Results
We studied 101 patients (80 females, 21 males). Their age ranged from 18 to 64 years (mean = 35 years). An average headache patient visiting our center was a middle-aged literate Hindu female. Majority of headache patients were either students or homemakers. Duration of headache ranged from 1 to 244 months (mean = 47.64, standard deviation = 49.625) and frequency of headaches per month ranged from 2 to 30 days per month (mean = 13.46, standard deviation = 8.847). Among patients with headache disorders, migraine was present in 50 (49.5%), TTH was seen in 23 (22.8%), CDH in 34 (33.66%), chronic migraine (CM) in 24 (23.76%). Nineteen out of 101 (18.81%) patients had more than one type of headache [Table 1].

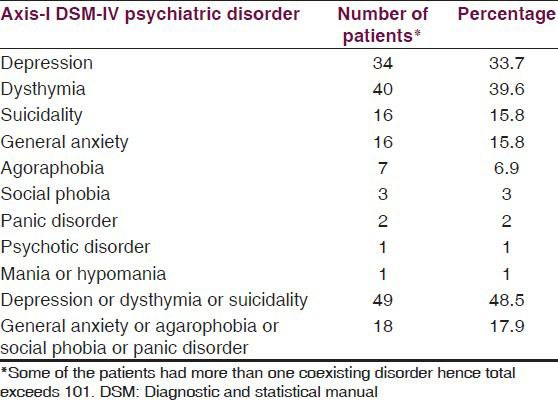
49 out of 101 (48.5%) patients with headache suffered from depressive disorders (dysthymia or depression or suicidality), 18 out of 101 patients with headache (17.90%) suffered from anxiety related disorders (generalized anxiety disorder or agoraphobia or social phobia or panic disorder). No patient in our study suffered from posttraumatic stress disorder or obsessive compulsive disorder [Table 2].
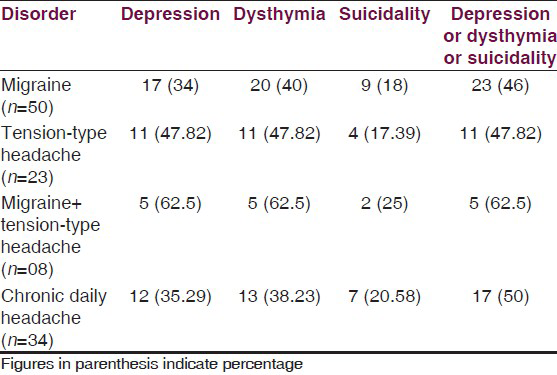
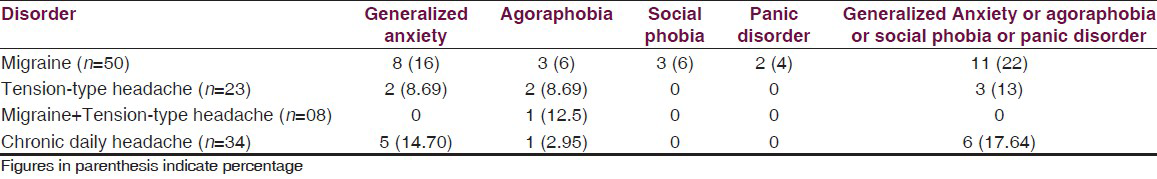
Among the patients, a depressive disorder was present in 46% of patients with migraine, 47.8% of patients with TTH and 62.5% of patients who had both migraine and TTH in combination (see supplementary Table 3). Anxiety-related disorders (either of generalized anxiety, agoraphobia, social anxiety or panic disorder) was present in 22% of patients with migraine, 13% of patients with tension-type headache and 17.6% of patients with chronic daily headache (see supplementary Table 4).
Linear regression findings showed that depression correlated with the headache frequency per month (sig. = 0.33), but not with any other variables. Also, linear regression findings of anxiety did not correlate with any demographic, clinical features and headache types.
Discussion
We used ICHD 2004 to diagnose headache type in this cross-sectional observational study. Although psychiatric comorbidity in patients with headache has been studied for long, a comparison across all the previous investigations is not possible due to different classification and case definition of headaches. For example, before 2004, certain headache types such as chronic migraine, which are frequently known to be comorbid with psychiatric disorders, were not defined by diagnostic criteria.
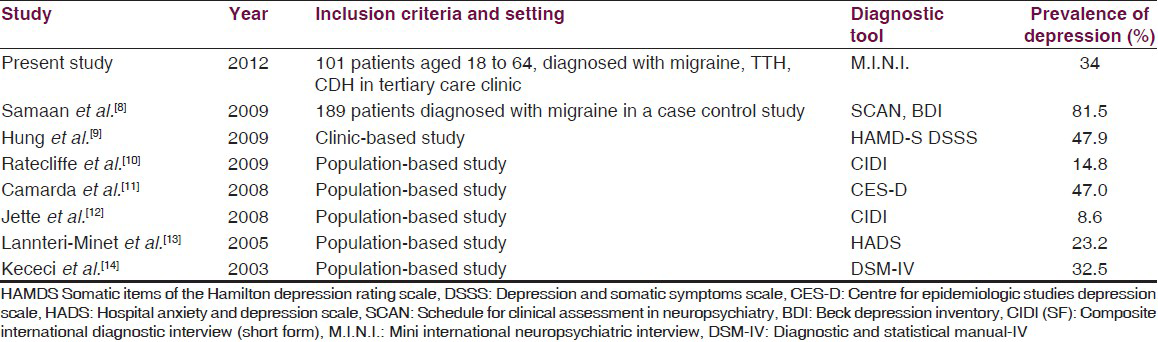
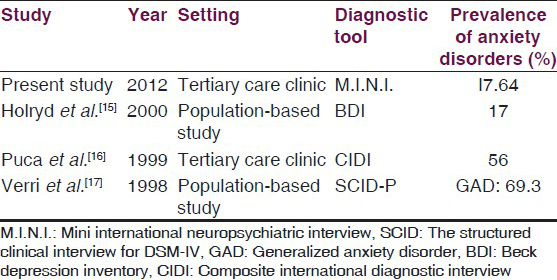
We studied psychiatric comorbidity by using M.I.N.I. in patients with headache visiting our neurology clinic. Researchers from different parts of the world have used other diagnostic tools in clinic and community settings.[891011121314151617] We observed that depression was prevalent in 34% of individuals with migraine in our study. However, the prevalence across different studies has ranged from 8.6% to 81.5% (see supplementary Table 5). Similarly, we observed a prevalence rate of 17.64% for anxiety-related disorders in patients with CDH, while the prevalence across different studies has ranged from 17% to 56% (see supplementary Table 6).
Our results are in concurrence with several previous reports indicating an association between migraine, other headache types and psychiatric disorders. Though our findings are based on a relatively smaller sample from hospital setting, the strength of our study lies in inclusion of well-defined cases of headache by a single neurologist and personal interview of patients for prevalence of DSM-IV psychiatric disorders using M.I.N.I.
Most studies have used other tools like Hamilton depression scale or BDI which are subjective and do not give a diagnosis on Axis-I DSM-IV classification and only judge patients to have “depressive” or “anxious” features on basis of their responses to questions. Scales like CIDI, SCID and SCAN give a detailed diagnosis on DSM-IV classification but are too lengthy for use in the outpatient clinic setting. We demonstrated that M.I.N.I. can be used in the outpatient setting easily and routinely in identifying psychiatric disorders among patients with headache.
Studies on psychiatric comorbidity among headache patients have demonstrated association of psychiatric disorder with chronic pain. Headache patients with long history and high frequency of headaches have higher prevalence of anxiety or depression.[151718192021] In our study we observed a correlation between frequency of headache and depressive disorders, however such a correlation was not found between anxiety disorders. Headaches comorbid with psychiatric disorders decrease the quality of life and result in worse prognosis, chronicity of disease and worse response to treatment. Improvement in mental health among such patients may improve the long-term pharmacotherapy of headache.[321] Among drugs used for prophylactic management of migraine, beta blockers may aggravate depressive symptoms, whereas tricyclic antidepressants are beneficial in patients.[22] Thus, identifying psychiatric comorbidity is also important in selection of therapeutic agent.
Conclusion
The present study has shown a significant prevalence of Axis-I DSM-IV psychiatric disorders in patients with headache reporting to our tertiary care neurology clinic. We found Mini International Neuropsychiatric Interview (M.I.N.I.) was found to be short, less time consuming, valid and reliable structured clinical interview for Axis-I DSM-IV disorders that can be easy to apply in clinic setting.
Source of Support: This study was awarded ICMR-STS (Indian Council of Medical Research Short term Student Research Scholarship),
Conflict of Interest: None declared.
References
- Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2163-96.
- [Google Scholar]
- Migraine and psychiatric comorbidity: A review of clinical findings. J Headache Pain. 2011;12:115-25.
- [Google Scholar]
- Psychiatric co-morbidity in patients with chronic daily headache and migraine: A selective overview including personality traits and suicide risk. J Headache Pain. 2009;10:283-90.
- [Google Scholar]
- Mini International Neuropsychiatric Interview English Version 5.0.0 DSM IV. Available from: http://www.nccpsychiatry.info/File/MINI500.pdf
- [Google Scholar]
- The Diagnostic and Statistical Manual of Mental Disorders DSM-IV TR. In: Text Revision: American Psychiatric Association (4th text edition). 2000.
- [Google Scholar]
- The International Classification of Headache Disorders Vol 24. (2nd ed). 2004. p. :9-160.
- New appendix criteria open for a broader concept of chronic migraine. Cephalagia. 2006;26:742-6.
- [Google Scholar]
- Migraine in recurrent depression: Case-control study. Br J Psychiatry. 2009;194:350-4.
- [Google Scholar]
- Migraine: A missing link between somatic symptoms and major depressive disorder. J Affect Disord. 2009;117:108-15.
- [Google Scholar]
- The relationship between migraine and mental disorders in a population-based sample. Gen Hosp Psychiatry. 2009;31:14-9.
- [Google Scholar]
- Comorbidity between depressive symptoms and migraine: Preliminary data from the Zabút Aging Project. Neurol Sci. 2008;29(Suppl 1):S149-51.
- [Google Scholar]
- Comorbidity of migraine and psychiatric disorders--a national population-based study. Headache. 2008;48:501-16.
- [Google Scholar]
- Migraine and probable migraine--results of FRAMIG 3, a French nationwide survey carried out according to the 2004 HIS classification. Cephalalgia. 2005;25:1146-58.
- [Google Scholar]
- Co-morbidity of migraine and major depression in the Turkish population. Cephalalgia. 2003;23:271-5.
- [Google Scholar]
- Psychiatric comorbidity and psychosocial stress in patients with tension-type headache from headache centers in Italy. The Italian collaborative Group for the study of psychopathological factors in primary headaches. Cephalalgia. 1999;19:159-64.
- [Google Scholar]
- Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000;40:3-16.
- [Google Scholar]
- Psychiatric comorbidity in chronic daily headache. Cephalalgia. 1998;18(Suppl 21):45-9.
- [Google Scholar]
- Depression and anxiety disorders associated with headache frequency. The Nord-Trøndelag Health Study. Eur J Neurol. 2003;10:147-52.
- [Google Scholar]
- Prevalence and risk factors for depression and anxiety among outpatient migraineurs in mainland China. J Headache Pain. 2012;13:303-10.
- [Google Scholar]
- Overview of diagnosis and treatment of migraine. Neurology. 1994;44(10 Suppl 7):S6-16.
- [Google Scholar]






