Translate this page into:
Sociodemographic, Rationale Drug Use of Antiepileptic Drugs among Pediatric Patients with Epilepsy: A Prospective Study at a Tertiary Care Hospital
S. Dwajani, PhD Department of Pharmacology, Central Research Laboratory, Rajarajeswari Medical College and Hospital Bengaluru 560 074, Karnataka India dwajani@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Drug utilization studies are important and considered as a potential tool for the evaluation of health care systems. The goal of drug utilization research studies should be to assess whether drug therapy is rational or not.
Objective The main aim of this article is to analyze the different types of epilepsy and their drug utilization pattern in children with epilepsy at the Department of Pediatrics and evaluate the extent of older and newer antiepileptic drugs (AEDs), either as monotherapy or polytherapy in pediatric age groups.
Materials and Methods To look into the sociodemographic profile of children with epilepsy, the type of epilepsy was diagnosed along with drug utilization pattern in children attending both outpatient and inpatient department of pediatrics. Demographic details were collected according to modified Kuppuswamy scale. Disease characteristics such as type of epilepsy, onset, duration, time since last attack, family history, comorbid conditions, monotherapy/polytherapy, dose, and duration of treatment were noted. Investigations such as electroencephalography, magnetic resonance imaging, and computed tomographic scan if any were recorded.
Results In this pilot study, we have 100 patients, younger than 18 years, with confirmed cases of epilepsy, receiving AEDs either monotherapy or polytherapy. Male predominance was 56%, and 60% were from rural areas and 40% were from urban areas. As per the modified Kuppuswamy scale, we analyzed socioeconomic class of these 100 patients and found that 40% belong to lower-middle-class family. Nearly 51% were diagnosed with generalized tonic clonic seizures, 30% were with febrile seizures, while focal, partial, absence, and myoclonic seizures, and hot water epilepsy were less in percentage. Almost 83% received monotherapy, while only 17% received polytherapy. Among monotherapy, 51.80% received older AEDs and 48.20% received newer drugs.
Conclusion Although epilepsy can be controlled and managed effectively with older AEDs, an experience in management with newer AEDs is required to offer an additional advantage to patients to have better safety profile.
Keywords
antiepileptic drugs
epilepsy monotherapy
polytherapy
Introduction
Drug utilization studies are important and considered a potential tool for evaluation and assessment of health care systems. They are powerful exploratory tools to ascertain the role of the drugs in our society.1 Drug utilization study is an essential part of pharmacoepidemiology and is defined as “marketing, distribution, prescription and use of drugs in society with specific emphasis on resulting medical, social and economic consequences.”2 The ultimate goal of drug utilization research is to assess whether drug therapy is rational or not.3
It is important to develop a twin concept of therapeutic formulation and essential drugs list, which is considered to be the main reason for studying drug utilization.4 Hence, it becomes important in establishing a selected list of drugs, which needs to be guided to an important extent not just by epidemiological statistics and scientific considerations toward efficacy and safety, but also by the present pattern of treatment. Therefore, the mainstay in the management of epilepsy is antiepileptic drugs (AEDs). The comparison between the conventional and newer drugs with regard to their beneficial effects is still under debate. Treatment of epilepsy in children or adults is either by monotherapy or by combination of AEDs. Treatment with AEDs should be aimed and focused in such a way that controlling seizures with lesser side effects, possibly with monotherapy, allows the child to contribute actively to the society with cost-effective treatment. Childhood epilepsy remains a challenge to treat; despite an increase in the number of AEDs, children continue to have seizures.2
Hence, we decided to look into the sociodemographic profile of these children with epilepsy and type of epilepsy diagnosed along with drug utilization pattern in children attending both outpatient and inpatient departments of pediatrics. We like to consider this as a pilot study, as our further goal is to form a registry for pediatric epilepsy cases.
Materials and Methods
The study was conducted in a tertiary care hospital in Bengaluru, Karnataka, India, after obtaining ethical committee clearance. This was a prospective, observational study, in which the data were recorded in a register, and was considered as pilot study with an aim to continue as registry in large number of populations. In this pilot study, we have 100 patients, who attended outpatient and inpatient departments of pediatrics. Children younger than 18 years, with confirmed cases of epilepsy, receiving AEDs either monotherapy or polytherapy, were enrolled in the study only after obtaining consent from the parents or the legal guardians.
Data were entered in a register where demographic details were collected according to the modified Kuppuswamy scale. Disease characteristics such as type of epilepsy, onset and duration, time since last attack, frequency, family history of epilepsy, and comorbid conditions were also recorded. Treatment details such as monotherapy/polytherapy, dose, and duration of treatment were noted. Investigations such as electroencephalography (EEG), magnetic resonance imaging, and computed tomographic scan if any were recorded.
Results
A total of 100 patients were included in the pilot study. There was a male predominance (male children 56%, female children 44%). The majority of patients were in the age group of 1 to 5 years (42%), with male preponderance (61.90%), followed by 6 to 10 years (29%) of age (Fig. 1).

-
Fig. 1 Distribution of patients according to age. PWE, patient with epilepsy.
Fig. 1 Distribution of patients according to age. PWE, patient with epilepsy.
Among the 100 patients, 60% were from rural background and 40% were from urban background, while majority had completed their high school (31%) and 33% were under the category of clerk or were shop owners. As per the modified Kuppuswamy scale,5 we analyzed the socioeconomic class of these 100 patients, and we found that 40% belong to lower-middle-class family (Table 1).
|
Sociodemographic data |
Percentage |
|---|---|
|
Abbreviation: PUC, pre-university course. |
|
|
Education of head of the family |
|
|
Illiterate |
23 |
|
Primary school |
6 |
|
Middle school |
10 |
|
High school |
31 |
|
Intermediate school |
12 |
|
Graduate and PUC |
17 |
|
Professional and honor |
1 |
|
Occupation of head of the family |
|
|
Unemployed |
0 |
|
Unskilled |
23 |
|
Semiskilled |
7 |
|
Skilled |
32 |
|
Clerical, shop owner |
33 |
|
Semiprofessional |
5 |
|
Profession |
0 |
|
Socioeconomic class as per the modified Kuppuswamy scale5 |
|
|
Upper class |
0 |
|
Upper middle class |
22 |
|
Lower middle class |
40 |
|
Upper lower class |
38 |
|
Lower class |
0 |
On assessing the family history of seizures, 42% of patients reported with positive cases of epilepsy on treatment/being treated, within their near/dear family members. With regard to the initiation of treatment, 56% of patients began treatment with AEDs immediately within 3 months of attack (Table 2). That is, the patient was brought to the hospital soon after the attack.
|
Time duration |
Percentage |
|---|---|
|
With 3 mo of the attack |
56 |
|
4 mo–1 y of attack |
20 |
|
1–2 y of attack |
3 |
|
2–3 y of attack |
4 |
|
>3 y |
17 |
EEG was done as a diagnostic tool in all the 100 patients, where 40% patients had abnormal EEG findings. Among these 100 pediatric patients, majority (51%) were diagnosed with generalized tonic clonic seizures (GTCS) followed by febrile seizures (30%); focal seizures; partial, absence, and myoclonic seizures; and hot water epilepsy, which were less in percentage. Other types of seizures include hypoglycemic seizures (n = 1) and abdominal seizures (n = 1) (Fig. 2).

-
Fig. 2 Type of seizures in pediatric patients with epilepsy. CPS, complex partial seizure; GTCS, generalized tonic clonic seizures; PWE, patient with epilepsy.
Fig. 2 Type of seizures in pediatric patients with epilepsy. CPS, complex partial seizure; GTCS, generalized tonic clonic seizures; PWE, patient with epilepsy.
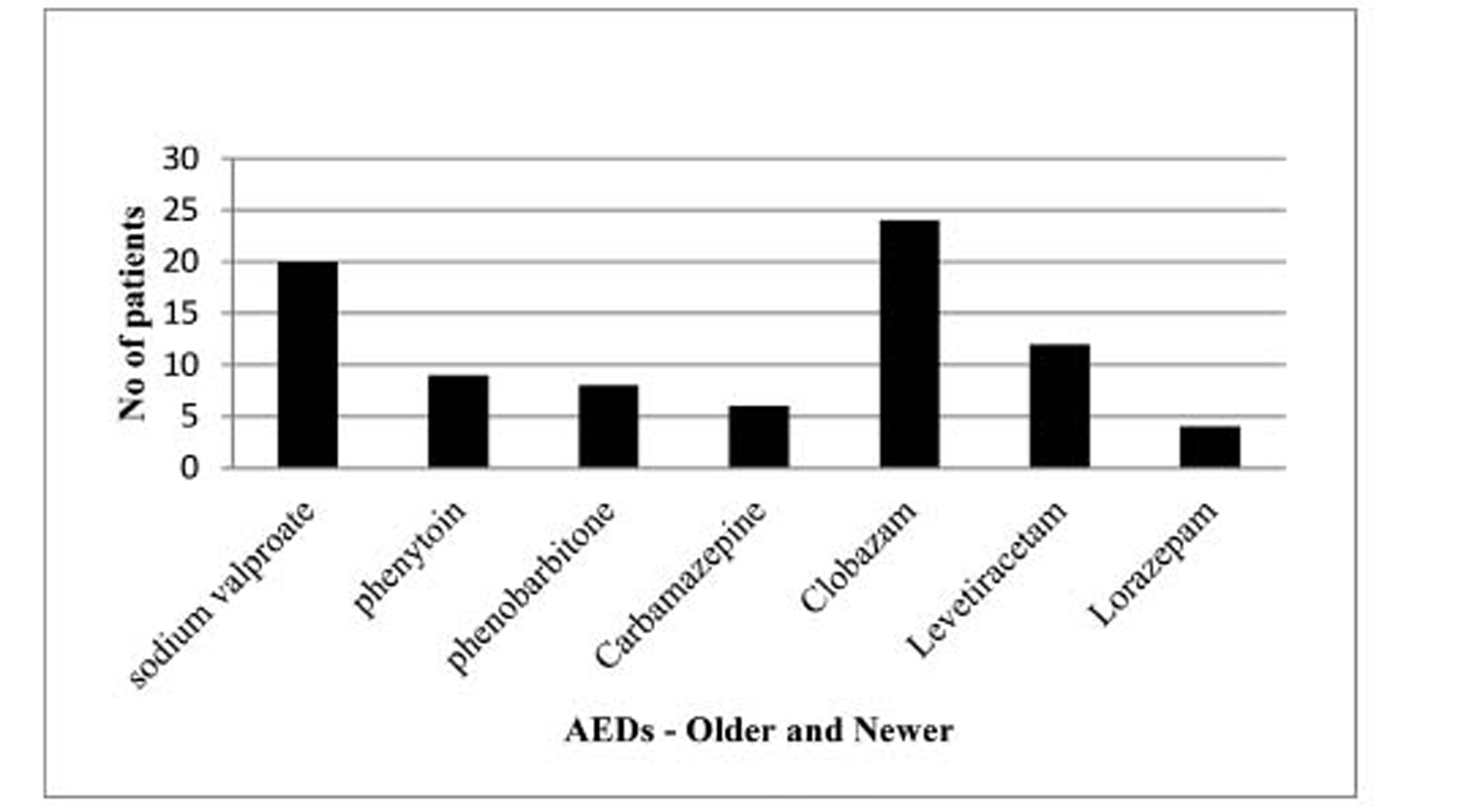
With regard to the treatment with AEDs, the majority of the patients (83%) received monotherapy, while only 17% received polytherapy. Among patients who received monotherapy, 51.80% received older AEDs and 48.20% received newer drugs (Fig. 3). Among polytherapy, all patients received two drug combinations with older or with older + newer AEDs (Table 3).
-
Fig. 3 Treatment pattern of antiepileptic drugs in pediatric patients with epilepsy receiving monotherapy. AEDs, antiepileptic drugs; PWE, patient with epilepsy.
Fig. 3 Treatment pattern of antiepileptic drugs in pediatric patients with epilepsy receiving monotherapy. AEDs, antiepileptic drugs; PWE, patient with epilepsy.
|
Polytherapy AED combination received (n = 17) |
n(%) |
|---|---|
|
Abbreviation: AED, antiepileptic drug. |
|
|
Phenobarbitone + clobazam |
2 (11.76) |
|
Sodium valproate + levetiracetam |
2 (11.76) |
|
Phenobarbitone + levetiracetam |
3 (17.64) |
|
Phenytoin + levetiracetam |
1 (5.88) |
|
Sodium valproate + topiramate |
1 (5.88) |
|
Phenytoin + clobazam |
2 (11.76) |
|
Phenobarbitone + clobazam |
1 (5.88) |
|
Sodium valproate + clobazam |
3 (17.64) |
|
Levetiracetam + clobazam |
2 (11.76) |
Discussion
Childhood epilepsy results in potential impeding on education, social relation, and development of sense of being worthless. Diagnosis with prompt and appropriate treatment with AEDs will optimize the seizures. Drug therapy with AEDs is the mainstay of epilepsy treatment. The major goal in treatment with AEDs is to minimize the frequency of seizures and to reduce the side effects. This becomes important because pediatric patients differ anatomically and physiologically from normal healthy adults with regard to weight and surface area. The physiological systems in pediatric patients are in growing phase, which contribute to change in pharmacokinetic and pharmacodynamic effects.4
In our study, a majority of patients receiving AEDs were male and belonged to age group between 1 and 5 years, which is similar to the study done by Bhatt et al3 as well as Maity and Gangadhar.4 As per the modified Kuppuswamy scale, we found that 40% belong to lower-middle-class family and had started the treatment immediately after an attack. This could be because of the education, better financial status, and knowledge about epilepsy among parents of children with epilepsy, while 17% of patients were treated only after 3 years of the first attack which could be due to social stigma, lower financial background, and myths and misconceptions among the parents of children with epilepsy. Socioeconomic status, mainly the income, plays a very important role in the quality of life among patients with epilepsy as reported by Nagarathnam et al.6
Positive family history of seizures was found in 46% of patients. It has been reported in the previous study that epilepsy is a hereditary disorder; family history and genetic predisposition lead to an increased risk of seizure in children.7 The majority (i.e., 56%) of patients had no specific cause for seizure, which was similar to the study by Hanssens et al8 conducted in 2002. EEG was done in all the 100 pediatric patients, with epilepsy considered as the diagnostic tool. As per the American Academy of Neurology guidelines for epilepsy, EEG is recommended as a part of routine neurodiagnostic evaluation for the diagnosis of epilepsy.9
An International League Against Epilepsy classification of epilepsy and epileptic syndromes is useful for the diagnosis and management of epilepsy. The majority (51%) had GTCS, followed by 30% of focal seizures. In this study and in other study conducted at Oman by Hanssens et al,8 it was summarized that GTCS was the major type of epilepsy, while in contradiction, two different studies conducted in Malaysia and Sweden by Hasan10 and Larsson,11 respectively, showed that focal seizures were in majority, which could be due to racial, ethnic, or genetic difference of various regions. With regard to the treatment of epilepsy, sodium valproate monotherapy was the most common AED prescribed (24.09%), which is similar to the study from the United Kingdom (22%) conducted by Moran et al.12 In comparison to other studies, carbamazepine was the most common drug followed by sodium valproate,13 14 15 16 while in a study conducted in European and Asian countries, sodium valproate was the least prescribed AED.16 17 As per the National Institute of Clinical Excellence (NICE) guidelines, it has been advised that either sodium valproate or carbamazepine should be considered as the first line of therapy for epilepsy. If in case there is no control with one drug, alternative monotherapy with other AEDs should be tried before considering polytherapy. In the recent trends, shifting of prescription pattern to these older drugs, that is, sodium valproate and carbamazepine from phenobarbitone and phenytoin, could be due to better safety profile.
The newer AEDs are not being recommended as first-line drugs owing to limited clinical experience and cost, while the use of these drugs is reserved for such epileptic patients who do not respond to older AEDs. The NICE guidelines report that the role of newer AEDs as first-line monotherapy will come into action only when randomized clinical trials can prove their efficacy role in comparison to older AEDs. In our study, levetiracetam was the most commonly used AED in contrast to lamotrigine and oxcarbazepine being prescribed commonly in a study conducted by Maity and Gangadhar4 and Bhatt et al,3 respectively. Clobazam was the second widely used drug among newer AEDs for febrile seizure reported in 30% of cases in our study. Comparing to a study conducted by Gupta,18 it was reported that children younger than 12 months, diagnosed with febrile seizures, may have 50% chances of recurrent febrile seizures, which is considered as the most common type of seizure among children. The present study has indicated that monotherapy is the modality of treatment, which is used frequently in all types of seizures. Monotherapy is preferred over polytherapy because of low-cost, better safety profile with lesser side effects and undesirable drug interactions. This also helps in improving medication compliance and adherence because of simplified drug administration. Only in those patients in whom single drug therapy does not control seizures effectively, polytherapy may be necessary as better treatment goal. Monotherapy is considered as gold standard for treatment of epilepsy, which is effective in 44 to 79% of patients,19 20 21 and this study proves in accordance with it.
Conclusion
A national-based study and guidelines will help us to bring more rational approach for AED therapy. Very few studies have been conducted on childhood epilepsies and are compared with different treatment options or to prove certain guidance concerning treatment strategies. Although epilepsy can be controlled and managed effectively with older AEDs, an experience in management with newer AEDS is required to offer an additional advantage to patients to have better safety profile. Hence, this study helps in evaluating the existing drug use pattern and rationality of prescription, while most of the prescription was as per the NICE guidelines. Our study had a limitation of smaller sample size, as this was considered to be a pilot study. Further to this, a registry study is being conducted at our hospital, with larger sample size for better assessment of rational drug prescribing.
Conflict of Interest
None declared.
Funding None.
References
- Drug utilization pattern of antiseizure drugs and their adverse effects in the pediatric population, in a tertiary care hospital attached to medical college. Int J Basic Clin Pharmacol. 2014;3:336-343.
- [Google Scholar]
- Drug utilization in pediatric neurology outpatient department: a prospective study at a tertiary care teaching hospital. J Basic Clin Pharm. 2014;5(3):68-73.
- [Google Scholar]
- Trends in utilization of antiepileptic drugs among pediatric patients in a tertiary care hospital. Curr Neurobiol. 2011;2:117-123.
- [Google Scholar]
- Socio-economic status scales updated for 2017. Int J Res Med Sci. 2017;5:3264-3267.
- [Google Scholar]
- Assessment of quality of life in epilepsy in Andhra Pradesh. Neurol Asia. 2014;19:249-255.
- [Google Scholar]
- Seizures in childhood. (18). 2007. p. :2457-2473. In eds Nelson Textbook of Pediatrics th edition
- [Google Scholar]
- Drug utilization pattern of anti-epileptic drugs: a phar-macoepidemiologic study in Oman. J Clin Pharm Ther. 2002;27(5):357-364.
- [Google Scholar]
- Quality Standards Subcommittee of the American Academy of Neurology; American Epilepsy Society. Practice parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69(21):1996-2007.
- [Google Scholar]
- Antiepileptic drug utilisation and seizure outcome among paediatric patients in a Malaysian public hospital. Singapore Med J. 2010;51(1):21-27.
- [Google Scholar]
- A population based study of epilepsy in children from a Swedish county. Eur J Paediatr Neurol. 2006;10(3):107-113.
- [Google Scholar]
- Epilepsy in the United Kingdom: seizure frequency and severity, anti-epileptic drug utilization and impact on life in 1652 people with epilepsy. Seizure. 2004;13(6):425-433.
- [Google Scholar]
- Epidemiological study of the frequency of prescribing antiepileptic drugs. Folia Med (Plovdiv). 1992;34:8-13. 3/4
- [Google Scholar]
- West of Scotland Epilepsy Research Group. An audit of treated epilepsy in Glasgow. Seizure. 1996;5(1):41-46.
- [Google Scholar]
- Prevalence of epilepsy in rural Iceland: a population-based study. Epilepsia. 1999;40(11):1529-1534.
- [Google Scholar]
- Utilization pattern of drugs in epilepsy and factors influencing reactions to commonly prescribed drugsa study in South Indian patients. Indian J Pharmacol. 1993;25:83-87.
- [Google Scholar]
- Use of antiepileptic drugs in Estonia: an epidemiologic study of adult epilepsy. Eur J Neurol. 2006;13(5):465-470.
- [Google Scholar]
- Febrile seizures an overview and use of clobazam as intermittent therapy. . 2002;5:113-118. Pediatr Today
- [Google Scholar]
- Drug utilization pattern of antiepileptic drugs and traditional Chinese medicines in a general hospital in Taiwan a pharmaco epidemio logic study. J Clin Pharm Ther. 2000;25(2):125-129.
- [Google Scholar]






