Translate this page into:
Single Parietal Burr-hole Craniostomy with Irrigation and Drainage for Unilateral Chronic Subdural Hematoma in Young Adults <40 Years: A Rationale behind the Procedure
Address for correspondence: Dr. Milesh Nagar, Department of Neurosurgery, Medical College, Thiruvananthapuram - 695 011, Kerala, India. E-mail: millesh.kem@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Chronic subdural hematoma (CSDH) is one of the most common neurosurgical conditions. It is mostly a disease of elderly population with very little data about the young patients. There is also the debate regarding treatment strategies. We decided to determine the overall efficacy of the single burr-hole craniostomy (SBHC) for unilateral CSDH in young adults <40 years.
Subjects and Methods:
We performed a retrospective study of young patients undergoing SBHC for unilateral CSDH between January 2013 and June 2016 at our institution. Medical records were assessed based on patient characteristics in the form of sex of the patient, etiology, presenting symptoms, comorbidities, and signs including Glasgow Coma Scale, computed tomography (CT) brain findings (site and thickness of SDH with midline shift), and intraoperative presence of chronic/subacute component.
Results:
Mean age of the patient was 33.69 years (range 18–40 years), mean thickness of SDH was 15.47 mm, and mean midline shift was 11.26 mm. 61.54% patients were male, trauma being the most common etiology (92.31%) with most common presenting complaint being headache (90.38% patients). 69.23% patients presented within 1 day of onset of symptoms. On CT scan, most of the patients were having SDH thickness between 11 and 20 mm (67.31%) with midline shift of 6–10 mm (53.85%). Right-sided SDH was present in 53.85%. Intraoperatively, 63.46% patients had subacute SDH whereas 34.61% had chronic component. There were total 2 recurrences (3.85%).
Conclusions:
Young adults who present with unilateral CSDH usually have a history of trauma. They have shorter duration of symptoms and present mainly with the features of raised intracranial pressure such as headache and vomiting. SBHC with irrigation and drainage has excellent result for unilateral CSDH in young adults compared to other methods of drainage and should be considered treatment of choice unless contraindicated.
Keywords
Chronic subdural hematoma
irrigation and drainage
single burr-hole craniostomy
young adults
INTRODUCTION
Chronic subdural hematoma (CSDH) is one of the most common neurosurgical conditions with annual incidence of about 15.3 cases per 100, 000 population and is mostly a disease of elderly population. However, incidence of CSDH has been increasing in younger patients due to several clinical disorders that increase the risk of bleeding that include anticoagulant or antiplatelet therapy, hemodialysis, and systemic hematologic disease.[12]
Among neurosurgeons, preferred surgical method is also a matter of debate leading to lack of uniformity about the treatment strategies, such as the role of burr hole (single or double), twist drill, and craniotomy.
There is also disagreement about the use or disuse of drain and irrigation.[34] Although the surgical techniques are simple, recurrences remain one of the main challenges in the treatment.
Several studies reported the difference of clinical presentation and result of CSDH according to age. Hoewever, in most of the studies, number of young patients have been scarce to come to a solid conclusion.[5] More so, even if the number of patients were more, the patients were subjected to various surgical procedures according to the convenience and expertise of the operating surgeons rather than a single method.[6]
Hence, we preferred to study the outcome of single burr-hole craniostomy (SBHC) in young adults <40 years with CSDH which is the preferred method in our institute and being acceptable worldwide to have good outcome comparable to other methods[789] and also to describe characteristics of CSDH in terms of presenting symptoms, etiology, radiological features, intraoperative findings, and associated conditions in for those who underwent SBHC at our institute.
SUBJECTS AND METHODS
We performed retrospective study of patients <40 years with unilateral CSDH who underwent SBHC with irrigation and drainage for evacuation of unilateral CSDH from January 2013 to June 2016 at our institute. During this period, we operated an overall of 455 unilateral CSDH by SBHC out of which only 52 patients were adults younger than 40 years (18–40 years) (11.42%). The patients with CSDH who underwent other surgical treatments, such as twist-drill craniostomy (TDC), double burr-hole craniostomy (DBHC), craniotomy, and evacuation of SDH, were excluded from this study. Patients with thickness of the SDH <5–10 mm associated with up to 5 mm midline shift with Glasgow Coma Scale (GCS) 15/15 and no neurological deficits were closely observed and procedure was performed only on clinical deterioration. Patients with bilateral CSDH were also excluded from the study.
Medical records were analyzed based on patient characteristics in the form of sex of the patient, etiology, presenting symptoms, comorbidities, and signs including GCS, computed tomography (CT) brain findings [Figure 1] (site and thickness of SDH with midline shift), intraoperative presence of chronic/subacute component.
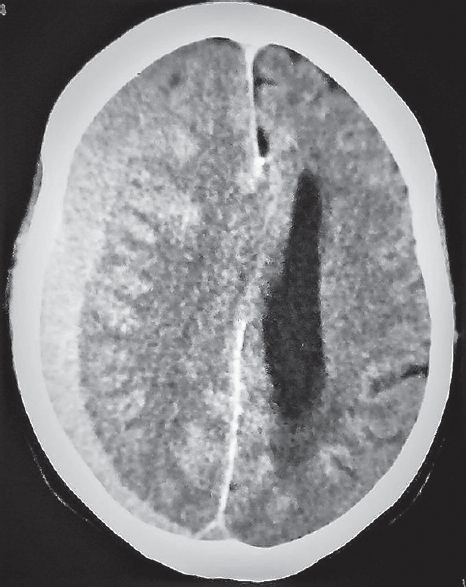
- Preoperative computed tomography brain plain demonstrating isodense collection in right frontoparietal region suggestive of subacute subdural hematoma with mass effect over the right lateral ventricle with midline shift to left
Results were assessed by comparative analysis of patient symptoms and signs including GCS. Postoperative CT [Figure 2] was taken after drain removal and before discharge and thereafter at 1-month follow-up or earlier during the hospital stay if the patient's symptoms persisted. Postoperative CT taken at 1-month follow-up (when the follow-up was 100%) was included in the evaluation criteria of the procedure if the patient improved clinically postoperative. Subsequent follow-up visits gradually declined over time to 78.85% (41 patients). For those patients living far away, who could not visit regularly for subsequent follow-ups, communication was by telephone. Subsequently, CT brain was performed on recurrence of symptoms.
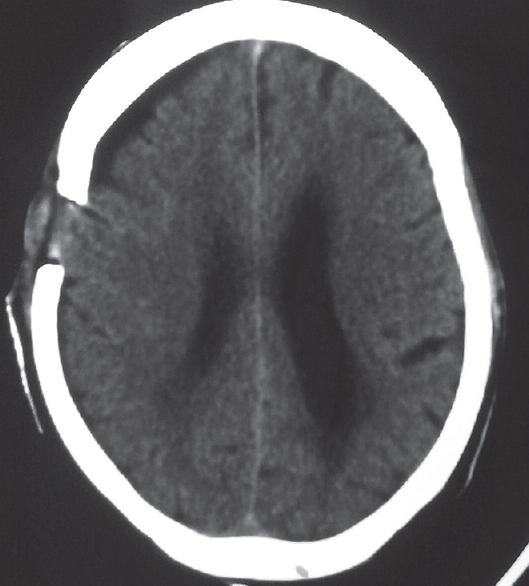
- Postoperative computed tomography brain plain demonstrating single burr hole over the right parietal area with complete evacuation of chronic subdural hematoma and resolution of mass effect and midline shift to left
RESULTS
Need for any redo surgical intervention or mortality due to surgery-related cause was considered to be failure.
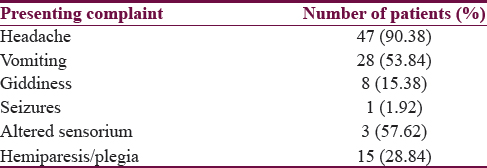
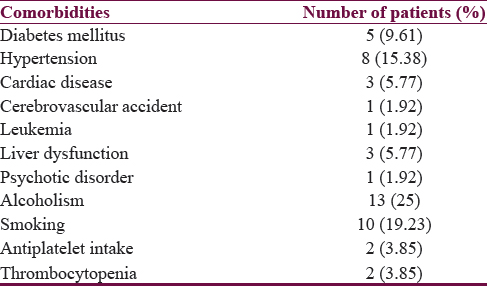
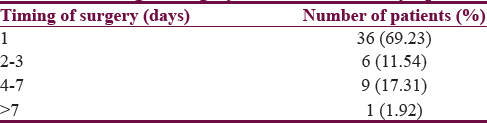
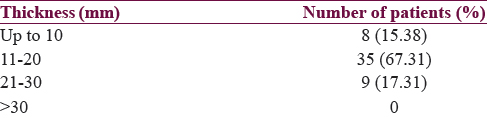
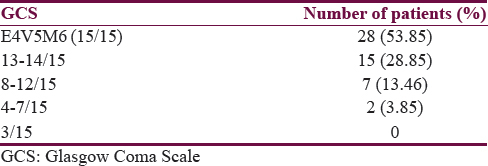
For the 52 patients included in this study, mean age of the patient was 33.69 years (range 18–40 years), mean thickness of CSDH was 15.47 mm, and mean midline shift was 11.26 mm. 61.54% patients were male [Table 1], trauma being the most common etiology (92.31%) [Table 2] with most common presenting complaint being headache (90.38% patients) [Table 3]. 13 (25%) patients were alcoholic and 10 were smokers(19.23%) [Table 4]. 69.23% patients presented within 1 day of onset of symptoms [Table 5]. On CT scan, most of the patients were having SDH thickness between 11 and 20 mm (67.31%) [Table 6] with midline shift of 6–10 mm (53.85%) [Table 7]. Right-sided SDH was present in 53.85% [Table 8]. Intraoperatively, 65.38% patients had subacute SDH whereas 34.62% had chronic component [Table 9].





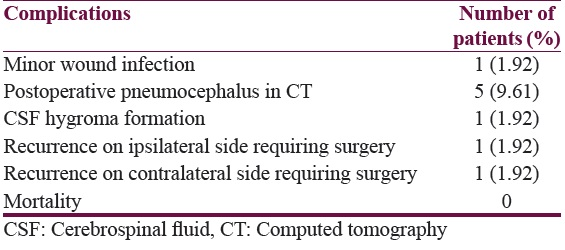
Fifteen of our patients preoperatively had hemiparesis and only two had GCS <8 (both had GCS E1V1M5) [Table 10], respectively. Even in these patients complete neurological recovery took place. There were total 2 recurrences (3.85%), one on the ipsilateral side whereas the other had recurrence on the opposite side. Both were dealt with redo surgery on their respective sides with the one on ipsilateral side required craniotomy due to active bleed [Table 11]. Both these patients also recovered fully neurologically after the second surgery during follow-up.
DISCUSSION
CSDH in young adults <40 years is a rare entity. In younger population compared to elderly population, there is reduced brain–dura mater interface, which prevents cortico-dural vein disruption during acceleration and deceleration during trauma and thus leading to decreased chances of subdural collection in young adults. In our series, patients presented mainly with headache and vomiting which suggest raised intracranial pressure. Altered sensorium, paresis, and seizures were infrequent. Most of the patients presented early probably due to less space for the CSDH to expand before causing symptoms. Lower rate of recurrence, shorter symptom duration, and fewer leading signs such as hemispheric symptoms seen in our study are comparable to that in other similar studies [Table 12].
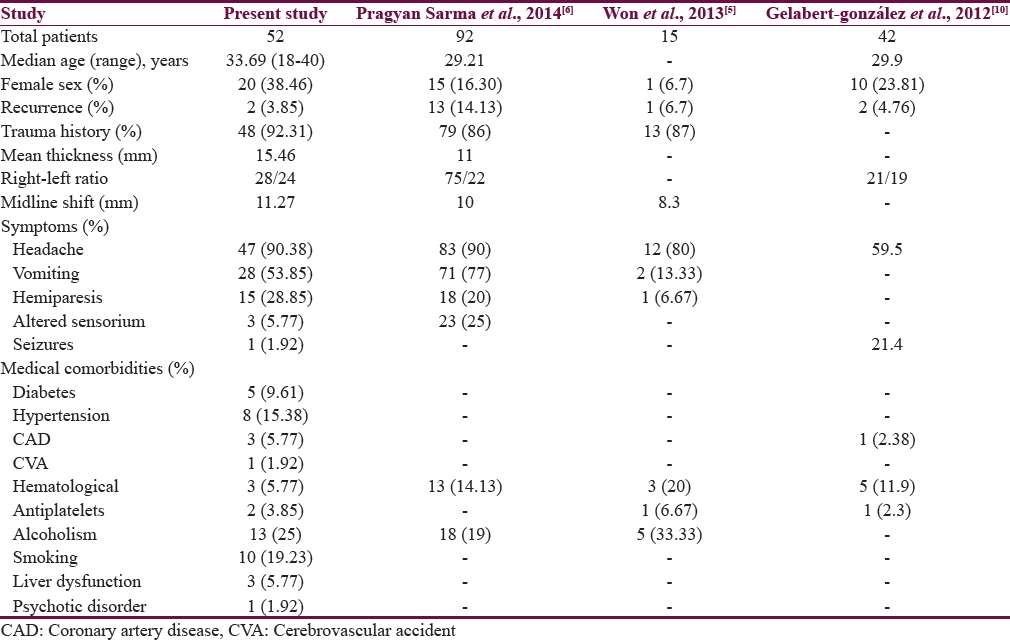
Most of the other studies [Table 12] have either only a few number of subjects in younger age group who underwent surgery for CSDH so as to draw a solid conclusion regarding the outcome. The series of Pragyan Sarma et al had 92 patients with complete records, which is one of the largest series in young patients in literature. However, in this study also, most of the patients underwent DBHC (48 patients) whereas single burr-hole procedure was performed in only 9 patients out of 92. They have also not mentioned in detail regarding recurrence in each of these procedures separately.[6]
Treatment through burr hole with irrigation and closed drainage is the most efficient, simple, and safe choice for surgical drainage of uncomplicated CSDH and is associated with low recurrence and lesser complications.[1112] Choice of single or double burr hole varies from surgeon to surgeon. SBHC with irrigation and closed drainage is sufficient to evacuate CSDH with lower or similar recurrence rate as compared to two burr hole group according to most of the studies.[789]
According to one paper, the treatment of CSDH with single burr hole is associated with a significantly higher postoperative recurrence rate, longer hospitalization length, and higher wound infection rate compared to that by double burr hole.[13] However, it is important to note that the subjects of this study were mostly old age (60 ± 12 years) and out of 97 CSDH, only 34 were treated with single burr-hole procedure; hence, it may not be true for young population which may have different presentations and comorbidities compared to older age. Moreover, the results depend on various other factors such as bleeding tendency, brain atrophy, preoperative GCS, alcohol abuse, bilateral CSDHs, higher hematoma density, postoperative air accumulation, and some technical aspects of surgery and so cannot be applied universally.[14151617]
On the other hand, SBHC is having recurrence rate compared to DBHC and has produced excellent results in our unit, especially in young patients. In young patients, brain expands rapidly during intraoperative period, hence obviating the need of double burr hole in most of the cases compared to the older population.[6] Moreover, most of the young patients present early and with thin CSDH which can be easily drained with single burr hole compared to older patients who have atrophic brain which allow accumulation of thick CSDH before the clinical manifestations set in.[5] Obviously, duration of surgery of CSDH by single burr hole is also less compared to double burr-hole technique as proposed by Lee et al. in 2009.[18]
TDC, on the other hand, takes much less time and can be performed under local anesthesia.[19] It is procedure of choice in high-risk surgical candidates in non-septated CSDH.[20] According to some studies, results of TDC are equivalent to burr-hole craniostomy in terms of recurrence rates, morbidity, and mortality.[2122] One recently published study suggests that TDC should be considered a first-choice treatment option for CSDH, especially in elderly patients, while burr hole should be reserved for more complicated cases.[23] This may be true for elderly patients who usually have large CSDH with atrophic brain but not in case of young adults who have thin SDH with normal brain which tends to rapidly expand on drainage. If performed in young subjects, TDC carries the risk of brain penetration and inadequate drainage. Being a blind procedure, it may also lead to acute epidural hematoma formation due to injury to middle meningeal artery. Many studies have shown high recurrence rate with TDC compared to burr hole procedure.[24]
Hence, we recommend SBHC with irrigation and drainage for unilateral CSDH in young adults.
However, our main problem was lack of long-term personal visit by the patients in clinic. As many as 11 patients (21.15%) did not comply with the advice of long-term personal visits beyond a few months. For those patients, we used telephonic communication. Nevertheless, all the patients who had any complaint attended in person for follow-up. Our patients, due to financial constraints, had no other option but to visit our center because of the lack of any other well-equipped tertiary care center in the locality which provides expert neurosurgery services free-of-cost.
CONCLUSION
Young adults who present with unilateral CSDH usually have a history of trauma. They have shorter duration of symptoms and present mainly with the features of raised intracranial pressure such as headache and vomiting. SBHC with irrigation and drainage has excellent result for unilateral CSDH in young adults compared to other methods of drainage and should be considered treatment of choice unless contraindicated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Chronic subdural hematoma: A review of the literature. Part 1. Ann Acad Med Stetin. 2009;55:47-52.
- [Google Scholar]
- The management of primary chronic subdural haematoma: A questionnaire survey of practice in the United Kingdom and the Republic of Ireland. Br J Neurosurg. 2008;22:529-34.
- [Google Scholar]
- Management of chronic subdural hematoma: A national survey and literature review. Can J Neurol Sci. 2005;32:501-6.
- [Google Scholar]
- Chronic subdural hematoma in young adult: An age comparison study. Korean J Neurotrauma. 2013;9:6-11.
- [Google Scholar]
- Subacute and chronic subdural hematoma in young population less than 40 years. Indian J Neurotrauma. 2014;11:1-4.
- [Google Scholar]
- One vs. two burr hole craniostomy in surgical treatment of chronic subdural hematoma. J Korean Neurosurg Soc. 2009;46:87-92.
- [Google Scholar]
- Single burr hole drainage for chronic subdural haematoma. Nepal Med Coll J. 2008;10:254-7.
- [Google Scholar]
- Single versus double burr hole drainage of chronic subdural hematomas. A study of 267 cases. J Clin Neurosci. 2010;17:428-9.
- [Google Scholar]
- Treatment of chronic subdural hematoma through a burr hole. Cir Cir. 2010;78:203-7.
- [Google Scholar]
- Number of burr holes as independent predictor of postoperative recurrence in chronic subdural haematoma. Br J Neurosurg. 2008;22:279-82.
- [Google Scholar]
- Reduction in the number of repeated operations for the treatment of subacute and chronic subdural hematomas by placement of subdural drains. J Neurosurg. 2003;99:44-6.
- [Google Scholar]
- The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg. 1981;55:390-6.
- [Google Scholar]
- Chronic subdural haematoma: Time to rationalize treatment? Br J Neurosurg. 2004;18:328-32.
- [Google Scholar]
- Chronic subdural hematomas: A comparative study of three types of operative procedures. J Korean Neurosurg Soc. 2009;46:210-4.
- [Google Scholar]
- An improved electronic twist-drill craniostomy procedure with post-operative urokinase instillation in treating chronic subdural hematoma. Clin Neurol Neurosurg. 2015;136:61-5.
- [Google Scholar]
- The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012;35:155-69.
- [Google Scholar]
- Use of twist-drill craniostomy with drain in evacuation of chronic subdural hematomas: Independent predictors of recurrence. Acta Neurochir (Wien). 2011;153:1097-103.
- [Google Scholar]
- Randomized comparative study of burr-hole craniostomy versus twist drill craniostomy; surgical management of unilateral hemispheric chronic subdural hematomas. Zentralbl Neurochir. 2008;69:129-33.
- [Google Scholar]
- Twist-Drill or burr hole craniostomy for draining chronic subdural hematomas: How to choose it for chronic subdural hematoma drainage. Korean J Neurotrauma. 2016;12:107-11.
- [Google Scholar]
- Chronic subdural hematoma – Craniotomy versus burr hole trepanation. Br J Neurosurg. 2009;23:612-6.
- [Google Scholar]






