Translate this page into:
Role of Decompressive Laminectomy without Instrumentation in the Management of Nurick Grade 4 and 5 Cervical Compressive Myelopathy
Address for correspondence: Dr. Dhaval P. Shukla, Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bengaluru - 560 029, Karnataka, India. E-mail: neurodhaval@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Cervical laminectomy is a very well-known posterior decompressive procedure for cervical compressive myelopathy (CCM). Our objective is to evaluate the functional effect of posterior decompressive laminectomy for poor grade CCM.
Methods:
This study was an observational retrospective study carried out on patients with poor-grade CCM who underwent decompressive laminectomy from January 2010 to December 2015. Patients with Nurick Grades 4 and 5 (walking with support or bedbound) were included in the study. Clinical data and radiological information were collected from medical records, and objective scales were applied to compare the surgical outcome between preoperative score and postoperative score.
Results:
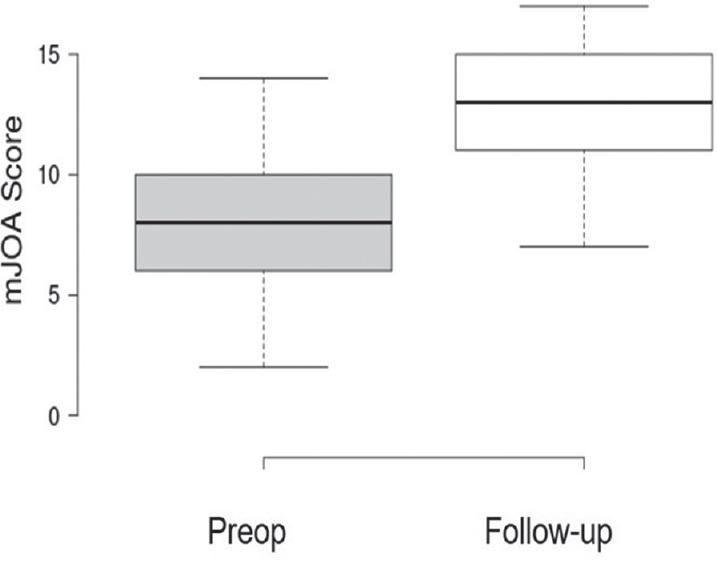
A total of 69 patients who underwent decompressive laminectomy for poor grade CCM were included. The mean age was 54.9 years, and the male-to-female ratio was 5.3:1. Ossified posterior longitudinal ligament comprised 52.6% cases. The follow-up data of at least 6 months’ duration after surgery was available for 57 (82.6%) cases. On comparing with preoperative Nurick grade at follow-up, 40 of the 57 patients (70.2%) were found to have improvement following surgery by at least one grade. The remaining 17 (29.8%) had either remained the same or had deteriorated further. The mean preoperative modified Japanese Orthopedic Association score was 8.4 ± 2.8, and the mean follow-up score was 11.8±0.3 (P = 0.0001). On multivariate analysis, the number of levels of laminectomy, postoperative deterioration, and anesthesia grade were predictors of outcome.
Conclusion:
Decompressive laminectomy for poor grade myelopathy is effective in improving functional outcome.
Keywords
Cervical canal stenosis
cervical myelopathy
decompressive laminectomy
nurick grade
ossified posterior longitudinal ligament
INTRODUCTION
A multilevel laminectomy is an effective and safe decompressive procedure when treating cervical myelopathy. Laminectomy as a single procedure is comparable to anterior procedures and laminoplasty regarding immediate postoperative results.[1] The result of decompression in the low-grade cervical myelopathy is well established.[2] However, there are very few studies in the literature comparing the results of decompression in high-grade cervical compressive myelopathy (CCM).[3] This study was undertaken to assess the outcome of cervical laminectomy without instrumentation in poor grade, i.e., Nurick Grades 4 and 5 (walking with support or bedbound) CCM.
METHODS
Study design
This study was an observational, retrospective study carried out on admitted patients with Nurick Grades 4 and 5 (poor-grade) CCM who underwent decompressive laminectomy in a single neurosurgical center from January 2010 to December 2015.
Inclusion and exclusion criteria
All patients who had undergone decompressive laminectomy for CCM due to degenerative spine disease with Nurick Grades 4 and 5 were included in the study. Patients with myelopathy due to spinal or intraspinal tumors, or arteriovenous malformation, congenital anomalies, and any other causes were excluded from the study. Patients with a follow-up of duration ≤6 months were excluded from the analysis.
Data collection
The data were collected from the medical records section and picture archival communication system of the institute. Clinical data reviewed included demographic parameters, duration of the disease, type of pathology, clinical findings, computed tomography (CT), and magnetic resonance imaging (MRI) findings, diagnosis, preoperative and postoperative Ashworth scoring of spasticity, preoperative and postoperative Nurick Grade, preoperative and postoperative American Spine Injury Association (ASIA) scores and modified Japanese Orthopedic Association (mJOA) grading of the severity of the disease. The bladder/sphincter dysfunction was assessed from history and bedside examination. A formal urodynamic examination was not done. Associated comorbidities and preoperative American Society of Anesthesiologist (ASA) grade were also noted. The radiological assessment of CT and MRI variables of the cervical spine was done to determine the number of levels involved with the highest level, the hyperintense signal on the T2 sagittal sequence, and diameter of the spinal canal. The sagittal alignment was also determined. The instability was determined using flexion/extension lateral radiographs. The intraoperative complications such as a dural tear, hypotension, etc., and postoperative neurological deterioration were noted. On follow-up, time since surgery, Nurick grade and mJOA score of myelopathy and sphincter status were collected. The patients were divided into two groups: one that improved by at least one Nurick grade, and other that did not improve, worsened, or died.
Outcome assessment
The following parameters were assessed:
-
Preoperative, postoperative, and follow-up Nurick grade of myelopathy
-
Preoperative and postoperative ASIA score
-
Preoperative and follow-up mJOA score
-
Preoperative and postoperative Ashworth grading of spasticity
-
Radiological findings of both computed tomography and magnetic resonance imaging and the postoperative outcome
-
Number of levels and the highest level involved and the postoperative outcome
-
Comorbidities and the postoperative outcome
-
Intraoperative complications and the postoperative outcome
-
Postoperative deterioration.
Statistical analysis
The statistical analysis of collected data was done under expert guidance using SPSS (IBM SPSS Statistics for Windows, Version 20.0, IBM Corp., Armonk, NY, USA). The continuous variables were expressed as mean ± standard deviation, ordinal variables as median and 1st interquartile (IQR), and categorical variables as percentages. The variables between the patients who improved, and the patients who did not improve were compared, and the significant difference was determined using appropriate test (t-test for continuous variables, Wilcoxon test for ordinal variables, and Chi-square test for proportions). The individual patient variables were compared using univariate and multivariate analyses for each group.
RESULTS
A total of 134 cases underwent decompressive laminectomy for CCM in a single neurosurgical unit between the period from January 2010 to December 2015. Of these, 69 (51.5%) patients were of poor grade CCM. Only 57 patients out of 69 patients (82.6%) had a follow-up of more than 6 months which met our inclusion criteria and were included in the study.
Demographics and clinical data
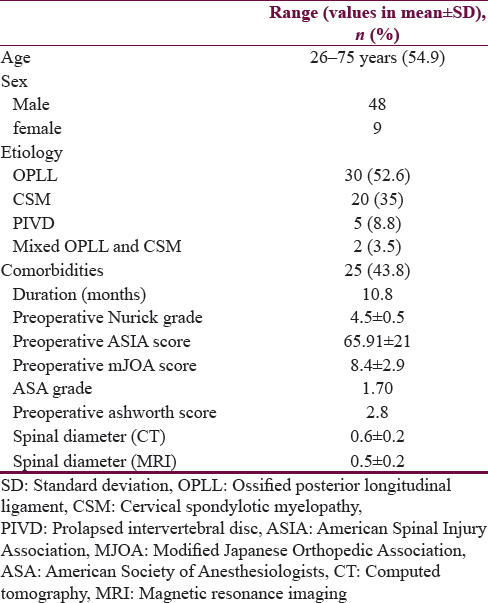
The mean age was 54.9 ± 11.8 years (range 26–75), with a male-to-female ratio was 5.3:1. The most common pathology was ossified posterior longitudinal ligament (OPLL) in 30 (52.6%) followed by cervical spondylotic myelopathy (CSM) in 20 (35%). Other pathologies were prolapsed intervertebral disc in 5 (8.8%) and mixed OPLL and spondylosis in two (3.5%). Seven (12.3%) patients presented when the symptoms developed following trivial trauma. The mean duration of symptoms was 10.8 months. There were 29 (50.9%) patients with Nurick Grade 4 and 28 (49.1%) with Nurick Grade 5. Twenty-five (43.8%) patients other medical conditions such as hypertension, diabetes mellitus, chronic smoking, alcoholism, blindness due to an unrelated cause, hepatitis B virus carrier, abdominal tuberculosis, previous history of ischemic stroke, and traumatic subarachnoid hemorrhage [Table 1].
Imaging
The complete imaging data of four patients were not available. All patients had T2 hyperintense signal changes on MRI. Most of the patients (56.6%) showed two level hyperintense signal changes on MRI. The C3 level was the most common highest level of T2 hyperintense cord signal change. All patients had either maintained cervical lordosis or straightening of cervical spine. None of the patients had cervical kyphosis. There was no cervical spine instability in any case. Imaging studies were available for 50% of the patients at follow-up. There was neither change in curvature nor stability as compared to preoperative.
Surgical details and complications
The patients underwent three to seven levels of laminectomy (median of 5) with the highest level at C1 and lowest level T1. However, the highest level of laminectomy was C3 in 52.6% and C2 in 40.3%. No spinal instrumentation was used. Laminoplasty was not done for any patient.
Complications
Five (8.7%) patients had intraoperative or immediate postoperative complications, which were a dural tear in two; and hypotension, bradycardia, and laryngospasm in one each. The complications were managed competently, and none of the patients had any adverse outcome due to these complications.
Seventeen (29.8%) out of 57 patients had immediate postoperative neurological deterioration defined as new onset weakness of limbs or progression of weakness or new onset urinary retention. Nine out of the 17 patients with neurological deterioration improved in Nurick grade on follow-up. One patient improved by three grades; two patients improved by 2 grades and rest improved by 1 grade.
Mortality
The overall mortality at follow-up was 5/27 (8.8%), 1/29 (3.4%) in Nurick Grade 4, and 4/28 (14.3%) in Nurick Grade 5. One patient who had immediate postoperative deterioration died on postoperative day 2. This patient deteriorated from a preoperative Nurick grades 4–5. Postoperative MRI showed increased T2 hyperintense cord signal changes as compared to preoperative scan suggestive of intraoperative injury. Two patients died about 20 days following surgery. Two patients died more than 1 month after surgery. The exact cause could not be ascertained as the patients had been discharged from the hospital at request. These patients had not improved following surgery and remained bed bound and most probably died due to comorbidities associated with being bed bound such as hypostatic pulmonary infection or pulmonary embolism. All these patients had a higher grade of ASA before surgery with significant comorbidities. Four patients had C2 as the highest level of laminectomy, and each of them underwent at least four levels of laminectomy. All patients with delayed mortality had Nurick grade 5. These five patients who died were included under those not improved or further deteriorated.
Functional outcome
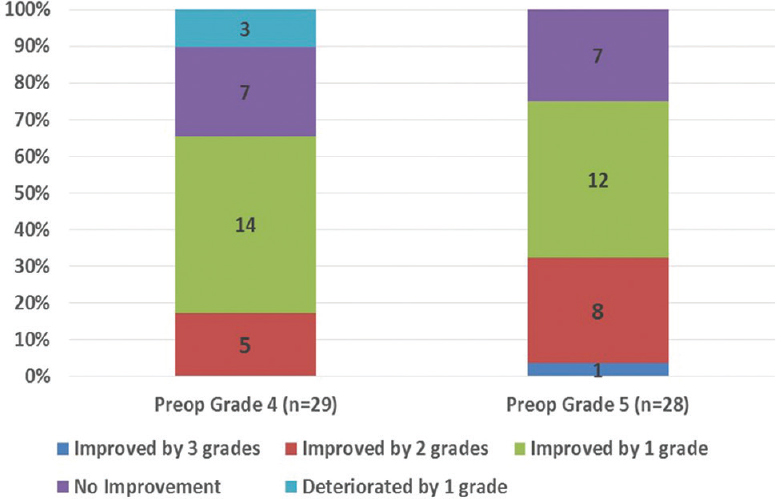
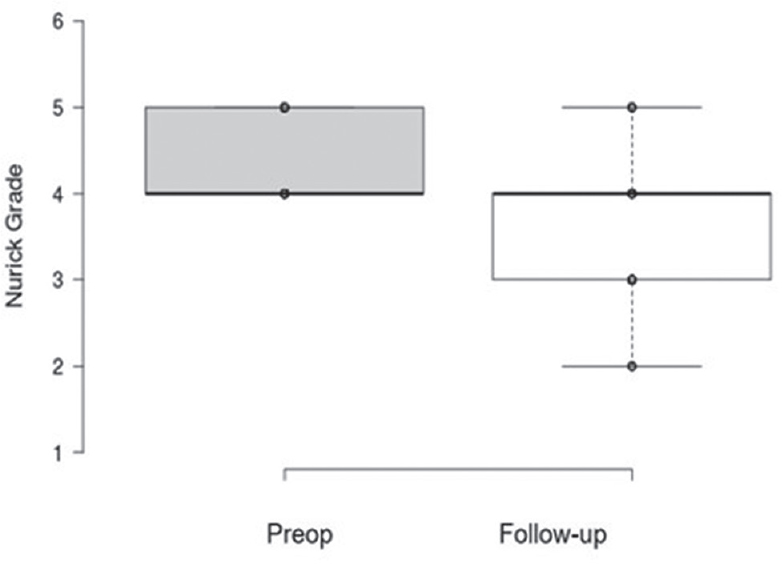
The mean follow-up duration was 19.5 ± 15.4 months (6–66 months). The outcome at follow-up of 57 patients was an improvement by at least one Nurick grade in 40 (70.2%), no improvement in 10 (17.5%), worsening in Nurick grade in two (3.5%), and death (including postoperative mortality) in 5 (8.8%). Out of a total of 29 patients with preoperative Nurick Grades 4, 5 (17.25%) patients improved by two grades, 14 (48.3%) improved by one grade, 7 (24.1%) remained the same, and 3 (10.3%) deteriorated to Grade 5. One of the three patients who deteriorated, expired in the postoperative period. Out of a total of 28 Nurick Grade 5 patients, one (3.6%) patient improved by three grades, 8 (28.6%) improved by two grades, 12 (42.6%) improved by one grade, and 7 (25%) did not improve [Figure 1]. Among the seven patients who did not improve four patients died within 6 months of surgery. Overall, the preoperative and follow-up mean Nurick Grade was 4.5 ± 0.5 and 3.6 ± 0.9. The mean preoperative and follow-up mJOA score were 8.4 ± 2.8 and 11.8 ± 0.3. The differences between preoperative and postoperative Nurick grade, [Figure 2] and preoperative and postoperative mJOA scores were significant (P < 0.001) [Figure 3].
- Improvement in Nurick grade
- Preoperative and follow-up Nurick grade
- Preoperative and follow-up modified Japanese Orthopedic Association score
Urinary bladder/sphincter function
Twenty-nine patients had preoperative neurogenic urinary dysfunction, among them, 12 were on an indwelling urinary catheter. At follow-up, 23 patients (79.3%) improved to normal bladder/sphincter function, and only six patients were on the urinary catheter. The improvement in urinary dysfunction was significant (P < 0.001). However, new onset neurogenic urinary dysfunction after surgery was observed in two out of 28 (7.1%) patients who had normal bladder/sphincter function.
Comparison of patients who improved and who did not improve
The variables which were included in our study were compared between two groups of patients: improved and did not improve or deteriorated to find the variable which had the strength to preoperatively determine the outcome. The univariate analysis showed that none of the preoperative variables had a significant effect on the outcome of the patients following surgery. Only ASA (P = 0.1), the number of levels laminectomy (P = 0.06), postoperative deterioration (P = 0.06) and the highest level of surgery/laminectomy (P = 0.055) even though not statistically significant, had some influence on the follow-up status of the patient [Table 2].
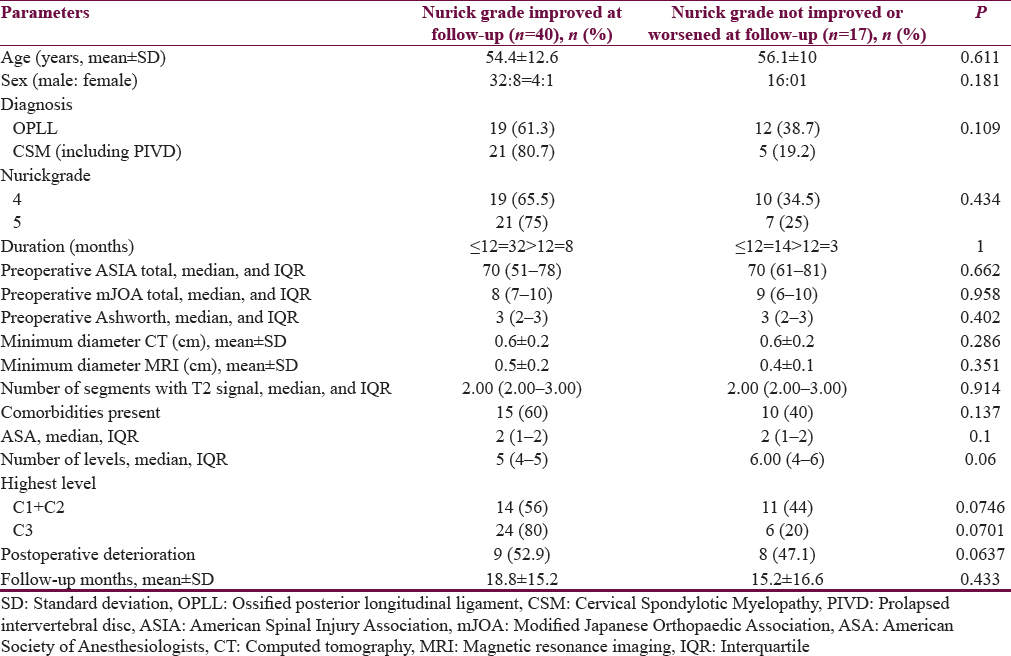
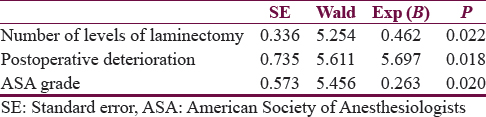
Multivariate analysis was done for the above mentioned four variables even though none of the variables were statistically significant. The result showed that even though individual variable had no significant effect on the outcome, when all of these were considered together using logistic regression analysis, more number of levels of laminectomy (P = 0.022), postoperative deterioration (P = 0.018) and higher ASA grade (P = 0.02) were found to significantly influence the outcome. Data fitted the model well as per Hosmer–Lemeshow test (χ2 = 5.856, P = 0.557), and correctly classified 77.2% of patients who did not improve or worsened after surgery [Table 3].
DISCUSSION
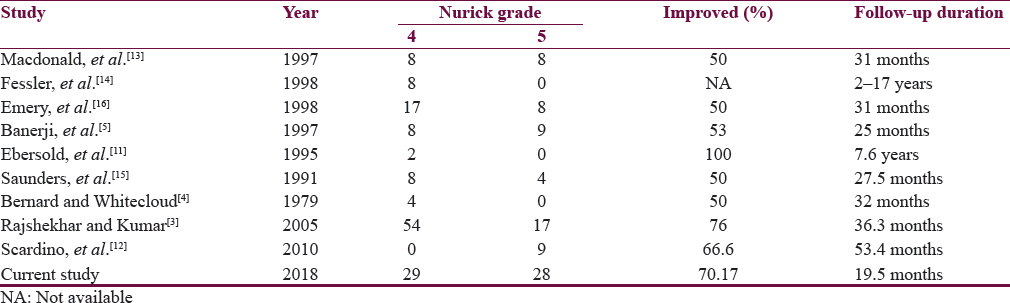
The functional surgical outcome data of cervical myelopathy with Nurick Grades 4 and 5 is sparse in literature. Two decompressive surgical approaches are performed for Nurick Grades 4 and 5 patients either anterior[45] (corpectomy with or without instrumentation) or posterior approach (laminectomy[6] or laminoplasty[7] with or without instrumentation). Hence, there is a mixed data available about the outcome after surgery.[8] Each decompressive approach has its own advantages and disadvantages.[910] In the anterior approach group, the disadvantages are longer surgical time, more blood loss, and 26% incidence of pseudoarthrosis. Radiographic degeneration of adjacent motion segments occurred with a greater frequency after corpectomy (38%) than after posterior procedures. We performed the simplest approach (decompressive laminectomy without instrument) among all the approaches in view of patients with older age group, medical comorbidity, and poor preoperative functional grade. Our aim was to do a short surgery and minimize anesthesia time and improve functional outcome after the surgery. We usually do not perform instrumentation for decompressive laminectomy in the absence of instability. This study is one of the large cohorts of selective Nurick Grades 4 and 5 patients who underwent only posterior decompressive approach (laminectomy without instrumentation). Irrespective of approach the outcome of surgery for poor grade myelopathy is generally perceived as not good. However, the improvement after surgery is reported in 50%–100% cases [Table 4].[3451112131415] In our series, an improvement by at least one Nurick grade was seen in 70.2%, non-improvement in 17.5%, worsening in 3.5%, and death (including postoperative and delayed mortality) in 8.8%. Besides mobility, there was an improvement in bladder/sphincter function in 79.3% of cases. A number of preoperative predictive factors associated with the functional outcome, and morbidity and mortality after surgery for poor grade CCM have been reported and are discussed below.
Age
Emery et al.[16] and Hukuda et al.[2] had found age more than 50 years was associated with poor outcome after surgery. However, a study by Rajshekhar, et al.[3] reported no association with age. Our study also reflects the similar finding.
Etiology of cervical compressive myelopathy
The most common cause of CCM in our group was OPLL (52.6%) which is in contradiction to another study on poor grade CCM published from the same geographical area.[3] There are contradictory reports about the cause of myelopathy and outcome. Ebersold et al.[11] reported better outcome with OPLL and Rajshekhar et al.[3] found with CSM. Our study did not find any correlation of outcome with the etiology of CSM or OPLL.
Duration of symptoms
Rajshekhar et al. mentioned that the duration of myelopathy is associated with worse outcome after surgery.[3] Yamazaki et al.[17] concluded that symptom duration was prognostically significant in elderly and the transverse area of the spinal cord at the level of maximal compression was predictive of outcome in all age groups. However, no correlation of age was found in the present study.
Preoperative impairment and functional status
In our study, the number of patients with Nurick Grades 4 and 5 was almost equal. We also used the ASIA score and mJOA to determine the severity of myelopathy. ASIA score is commonly used for nonprogressive conditions such as vascular pathologies and trauma.[18] This score has not been previously applied in degenerative conditions. We used ASIA score to determine neurological deterioration after surgery. In study by Rajshekhar et al. one of the favorable variables for improvement was preoperative Nurick Grade 5. However, patients with a preoperative Nurick Grade of 4 were more likely to experience a cure in their study.[3] None of the three scoring/grading system had strong correlation with functional outcome in our study. Although preoperative mJOA correlated significantly (P = 0.03) with postoperative Nurick grade, the correlation was weak (rho = −0.293) in our study. Although preoperative neurological status was not a significant factor in determining outcome, preoperative medical comorbidity and higher anesthesia risk as determined by ASA grade had a bearing on outcome in our study.
Magnetic resonance imaging finding
Studies quoted that the number of levels of hyperintense signals on T2W MRI had no influence on the outcome.[1319] However, the presence of T2 hyperintense cord signal changes shows significant cord involvement and prognosticates poor neurologic recovery as compared to patients without cord signal changes.[20] Mastronardi, et al.[21] and Chiles, et al.[22] found a positive association between spinal cord changes and final outcome. Our study did not show a correlation between MRI signal changes and final outcome. However, the number of levels of compression and laminectomy had a significant bearing on outcome in our study.
Perioperative complication, deterioration, and mortality
Various authors quoted different incidences of delayed deterioration after surgery and the incidence range from 5% to 30.8%.[3451112131415] In our cohort, 29.8% of the patients had immediate deterioration (motor power and bladder function) after decompression. However, 52.9% patients improved at follow-up. Our study had perioperative complication rate of 8.7%. Five patients (8.8%) expired after surgery. All these patients had a higher grade of ASA before surgery with significant comorbidities. The details of complications, deterioration, and mortality are not reported in literature. Postoperative neurological deterioration had a significant impact on functional outcome in our study.
The limitation of our study was similar as with any other retrospective study. In addition, we cannot avoid the selection bias as we performed the only the posterior approach to assess the functional outcome of Nurick Grades 4 and 5 patients. We have not analyzed the imaging results of laminectomy as the radiological changes after laminectomy take place years after surgery. The follow-up period was relatively short in our series; hence, it would not be appropriate to comments on radiological changes after laminectomy.
CONCLUSION
All Nurick Grades 4 and 5 CCM patients should be operated early with simple posterior decompression laminectomy to achieve the ultimate benefit of decompression. These patients should be counseled that about one-third of the patients may not improve after surgery and may even worsen. At present, it is possible to predict with only fair degree of accuracy which patient may improve after surgery. Patients with a higher risk for anesthesia, who require long segment laminectomy, and who worsen immediately after surgery are less likely to improve. A larger prospective study with a longer duration of follow-up is necessary for patients with Nurick 4 and 5 cervical myelopathy to establish the prognostic factors related to functional outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
The manuscript has been read and approved by all the authors, that the requirements for authorship as stated earlier in this document have been met, and that each author believes that the manuscript represents honest work.
REFERENCES
- Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg. 1998;89:217-23.
- [Google Scholar]
- Operations for cervical spondylotic myelopathy. A comparison of the results of anterior and posterior procedures. J Bone Joint Surg Br. 1985;67:609-15.
- [Google Scholar]
- Functional outcome after central corpectomy in poor-grade patients with cervical spondylotic myelopathy or ossified posterior longitudinal ligament. Neurosurgery. 2005;56:1279-84.
- [Google Scholar]
- Cervical spondylotic myelopathy and myeloradiculopathy. Anterior decompression and stabilization with autogenous fibula strut graft. Clin Orthop Relat Res. 1987;221:149-60.
- [Google Scholar]
- Corpectomy for multi-level cervical spondylosis and ossification of the posterior longitudinal ligament. Neurosurg Rev. 1997;20:25-31.
- [Google Scholar]
- Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord. 1991;4:286-95.
- [Google Scholar]
- Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: An independent matched cohort analysis. Spine (Phila Pa 1976). 2001;26:1330-6.
- [Google Scholar]
- Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: Results of the AOSpine north america prospective multi-center study. J Bone Joint Surg Am. 2013;95:1651-8.
- [Google Scholar]
- Spinal deformity and instability after multilevel cervical laminectomy. Spine (Phila Pa 1976). 1987;12:6-11.
- [Google Scholar]
- Surgical treatment for cervical spondylitic myelopathy. J Neurosurg. 1995;82:745-51.
- [Google Scholar]
- Is there a benefit to operating on patients (bedridden or in wheelchairs) with advanced stage cervical spondylotic myelopathy? Eur Spine J. 2010;19:699-705.
- [Google Scholar]
- Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990-7.
- [Google Scholar]
- Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery. 1998;43:257-65.
- [Google Scholar]
- Central corpectomy for cervical spondylotic myelopathy: A consecutive series with long-term follow-up evaluation. J Neurosurg. 1991;74:163-70.
- [Google Scholar]
- Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998;80:941-51.
- [Google Scholar]
- Cervical spondylotic myelopathy: Surgical results and factors affecting outcome with special reference to age differences. Neurosurgery. 2003;52:122-6.
- [Google Scholar]
- Severity score system for progressive myelopathy: Development and validation of a new clinical scale. Braz J Med Biol Res. 2012;45:565-72.
- [Google Scholar]
- Clinical and MRI predictors of outcome after surgical intervention for cervical spondylotic myelopathy. J Neuroimaging. 2007;17:315-22.
- [Google Scholar]
- Significance of increased signal intensity on MRI in prognosis after surgical intervention for cervical spondylotic myelopathy. J Clin Neurosci. 2011;18:1080-3.
- [Google Scholar]
- Prognostic relevance of the postoperative evolution of intramedullary spinal cord changes in signal intensity on magnetic resonance imaging after anterior decompression for cervical spondylotic myelopathy. J Neurosurg Spine. 2007;7:615-22.
- [Google Scholar]
- Cervical spondylotic myelopathy: Patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999;44:762-9.
- [Google Scholar]






