Translate this page into:
Removal of cervical spinal tumor with large inferio-lateral extension through anterolateral (interscalene and transforaminal) approach
Address for correspondence: Dr. Forhad Hossain Chowdhury, Department of Neurosurgery, Dhaka Medical College Hospital, Dhaka, Bangladesh. E-mail: forhadchowdhury74@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cervical spinal tumor with large lateral extension is usually removed through posterolateral approach and rarely through anterolateral approach. A young man presented with neck pain and brachialgia. Cervical spinal MRI showed a intraspinal tumor with huge extraforaminal paraspinal extension. We removed the tumor through anterolateral (interscalene and transforaminal) approach. Post operatively patient recovered from his sufferings and returned to normal life. Here we report the case along with operative technical aspects.
Keywords
Anterior-lateral approach
cervical spinal tumor
interscalenic approach
Introduction
Spinal schwannoma and meningioma constitutes the main bulk of spinal extramedullary tumor.[1] This type of schwannoma may be intradural, extradural or hourglass form (intra and extradural).[2] For removal of such tumor standard midline posterior, unilateral posterior, posterolateral, anterior and anterolateral approach has been described.[23456] Here we report removal of a cervical C7 spinal tumor with large inferolateral extension through anterolateral (interscalene and transforaminal) approach along with operative technical aspects.
Case Report
A thirty years old male presented with neck pain and left sided brachialgia. His neck movements were restricted and painful (mild to moderate pain). There was an ill-defined fixed mildly tender mass in left lower posterior triangle of neck. Hoffman's sign was bilaterally positive. But motor, sensory and autonomic functions including reflexes were normal in all limbs. Other general and systemic examination revealed no abnormality. MRI of cervical spine showed a 4 × 6 × 4 cm intradural extramedullary tumor with paraspinal extension through left C6 and 7 intervertebral foramen [Figure 1a–c]. Plain X-ray cervical spine showed large intervertebral foramen between C6 and 7 on left side [Figure 1d and e].
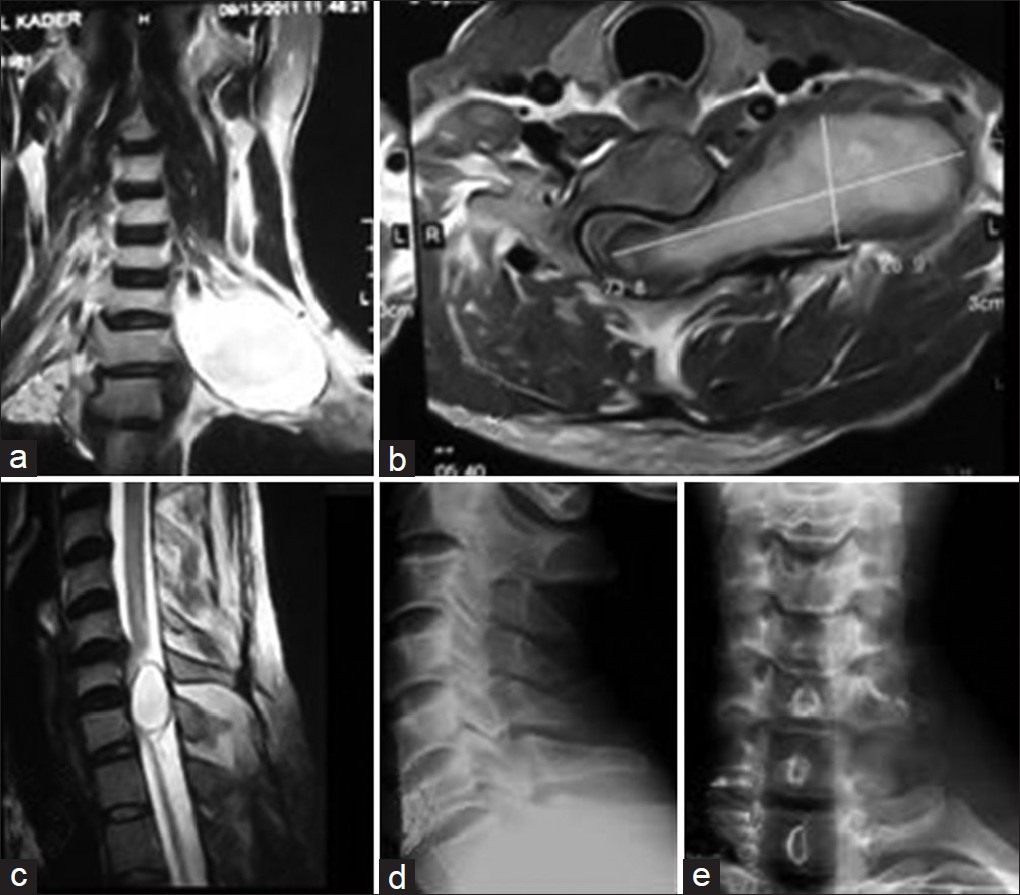
- Preoperative MRI of Cervical spine; a-coronal view, b-axial and c-saggital view showing intradural extramedullary tumor with paraspinal and inferolateral extension through left C6 and 7 intervertebral foramen. Preoperative X-ray of cervical spine; d-lateral view and e-antero-posterior view showing enlarged left C6 and 7 intervertebral foramen
Operation
Approach
Anterolateral (interscalene) approach was used to remove the tumor completely.
Position of the patient
Supine position; with 20 ° elevation of head and neck. Head was turned to right side. Left shoulder was slightly elevated and kept on slight traction toward the leg.
Incision
Under the operating microscope, a 4 cm transverse incision was made 4 cm above the middle third of left clavicle that extended over the posterior part of sternocleidomastoid muscle and anterior part of trapezius [Figure 2].

- Healed incision mark on left antero-lateral neck above the clavicle
Techniques
After cutting of subcutaneous tissue and platysma in the same line of skin incision investing layer of deep cervical fascia was cut along the posterior border of sternocleidomastoid 3 cm up and down to the skin incision line. Tumor was found after deep fascial incision. Sternocleidomastoid muscle was retracted anteriorly to exposure anterior scalenus muscle. On the anterior surface of anterior scalenus muscle phrenic nerve was identified and safeguarded by medial mobilization. Anterior scalenus muscle was cut above its insertion to scalenus tubercle of first rib after taking care not to injure subclavian vessels. Sternocleidomastoid muscle was retracted anteriorly and trapezius muscle was retracted posteriorly and the tumor was dealt. Fascia over the tumor capsule was dissected and tumor debulking was started but it was very hard and minimally vascular. Tumor was debulked by cutting with micro-scissor and sharp BP blade (No. 11). After removal of lateral part of tumor upper and middle trunk of brachial plexus came in view that were safeguarded. Medial part of the tumor was relatively soft and suck able, so removed by suctioning. Intraspinal intradural part was dealt through the C6 and 7 intervertebral foramen which was already capacious. The tumor easily came out through the dural opening along with arachnoid which was peeled off and tumor removed completely [Figure 3a–f]. Any bony work for foraminal enlargement was not needed and spinal stability seemed to be intact. Vertebral artery did not come in view. A portion of arachnoid remained outside the spinal canal through the dural opening with leaking of CSF. The redundant arachnoid was put inside the dura but closure of dural opening was not possible. For prevention of CSF leak, pseudo-meningocele or arachnoid herniation two pieces of thigh fat was put in the dead space. Wound was closed in layers without drain.
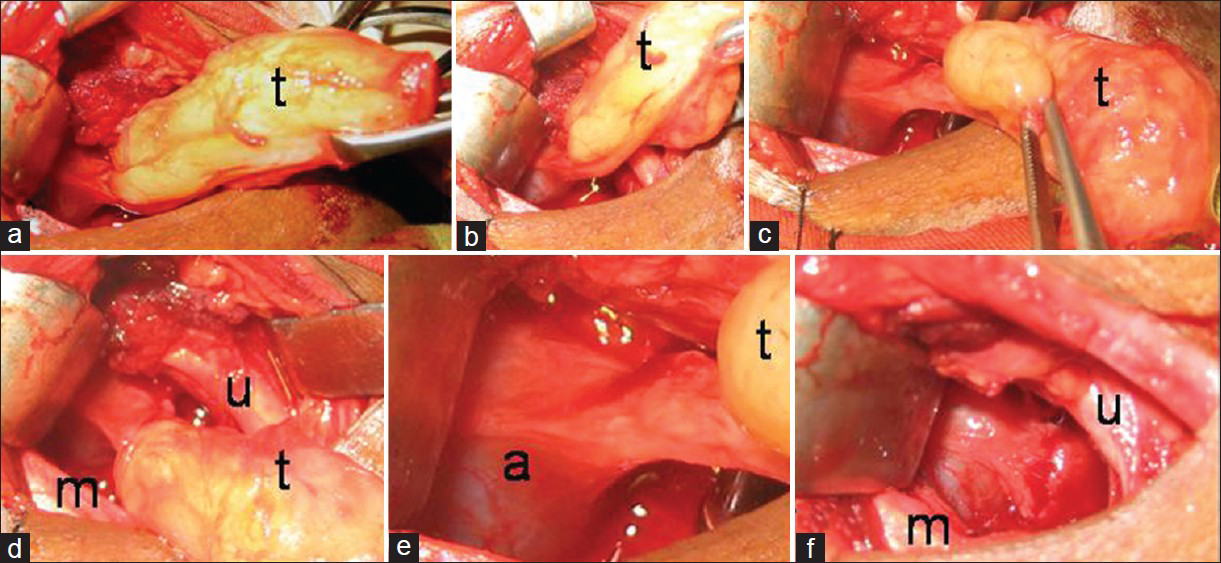
- a, b, c, d, e and f-steps of removal of last (medial part) of tumor along with preservation of surrounding neural structures. t-tumor, m-medial trunk of brachial plexus, u-upper trunk of brachial plexus and a-arachnoid mater
Postoperative period
Post operatively patient recovered uneventfully. Histopathological examination of operative specimen reported schwannoma Antoni A. His neurology after operation was intact. Postoperative MRI at the end of 4 months after operation showed no residual tumor but there was a pseudo-meningocele with grafted fat at the operated site [Figure 4a–d].
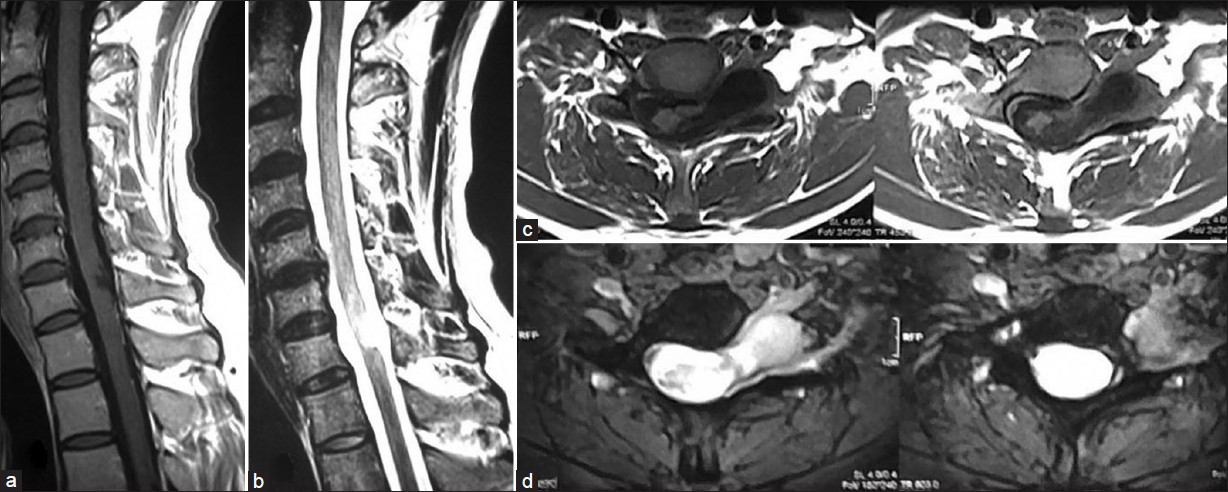
- Post-operative MRI of cervical spine. A-T1W saggital image and B-T2W saggital image showing no residual tumor in spinal canal with intact posterior elements of spinal column. C-T1W axial image and D-T2W axial images showing paraspinal pseudomeningocele with grafted fat and dead space
Discussion
70% spinal schwannoma arises from sensory root, 20% from motor roots and rest from both motor and sensory roots.[7] About 75% schwannomas are intradural, 10% intra-extradural and rest (15%) are extradural.[8] A multiplicity of schwannomas is frequently noted in cases involving NF Type 1. A multiplicity of schwannomas at any spinal level is reported in approximately 4% of cases.[35] Symptoms and signs are usually diagnostic in nature. Unusual symptoms of syncopal attacks, migraine headaches, and unrelated motor and sensory symptoms, however, can lead to misdiagnosis.[910] These tumors are slow growing and usually attain a large size before becoming symptomatic.[9] Dumbbell-shaped tumors located elsewhere in the spine are generally classified as intraspinal, foraminal, and extraforaminal.[2] Asazume et al. classified cervical dumbbell tumors in six types as follows: Type I represents intraspinal intra- and extradural tumors which constrict the dura and do not involve the foramen. Type IIa, lesions are extradural, show foraminal constriction, but are not extraforaminal. Types IIb and IIc tumors are extradural/paravertebral and foraminal/paravertebral, respectively. Type III tumors have both dural and foraminal constrictions: Type IIIa tumors include intra- and extradural foraminal tumors with dural and foraminal constructions and IIIb are intra- and extradural paravertebral. Type IV tumors are extra- and intravertebral and invade the vertebral body; type V lesions are extradural and extralaminal with laminar invasion and type VI tumors show multi-directional bone erosion.[11] PUTH classification for cervical dumbbell tumors includes 7 categories (types 1-7) and 2 foraminal modifiers. Posterior approach is appropriate for PUTH type 1, 2 and 5 tumors, anterior and anterolateral approach is an ideal choice for type 4 and 6 tumors.[12] PUTH Type 7 tumors need combined anterior and posterior approach. Malignant changes of such tumor are marked by infiltration of paraspinal muscles and destruction which is rare.[9]
These tumors are located lateral, anterolateral, or anterior to the spinal cord. Several posterior, posterolateral, lateral, and anterolateral approaches have been described to surgically approach these tumors.[234513] Pecker et al. in 1980 reported interscalene removal of six intervertebral foramen schwannoma; then there is large pause in the literature regarding this approach.[11] Our report is probably the second in the literature describing interscalene transforaminal approach for removal of C7 spinal nerve schwannoma. Standard midline posterior approach is suitable and most appropriate to resect almost all types of schwannomas with transtumoral resection techniques. A similar surgical strategy had been reported by several investigators in the past.[24] The exposure used in the surgery (midline posterior approach) is standard and quick and there is no need for manipulation of any cranial nerves, blood vessels, or joints to affect exposure.[9] Tumor with large paraspinal extension posterolateral is usually used[234] and rarely anterior-lateral approach[6] is used. These tumors are less vascular and most are firm in consistency. Such schwannomas are relatively simple to resect because they have a well-defined arachnoid plane of dissection intradurally and well defined capsule extradurally.[9] In some cases of dumbbell schwannoma, extradural portion is covered with an attenuated dura and that the dural ring is invaginated into the intradural portion. Kim et al. suggested that invagination of the dural ring is the anatomical feature that may be confused with an intradural/extradural tumor during operations for extradural dumbbell tumors; so initial epidural mass removal, extraction of intradural/extradural tumors subsequent to dural opening, and affirmation of presence of intradural tumor remnant could save time during dumbbell tumor surgery.[14] Some authors have suggested proximal control of the VA prior to tumor resection.[3] There is a low risk of VA injury in this surgery. So preoperative angiography or intraoperative proximal or distal control of the VA does not appear to be necessary.[15] After the tumor removal, attention should be made for spinal instability as sometime it may present, if present it should be stabilized.[9] Successful tumor resection results in rapid and sustained neurological recovery.[9] Total tumor resection is advocated by several authors for complete treatment of the disease. The significant chance of early tumor recurrence in a partially excised tumor is known,[16] and every attempt should be made to remove them completely.[9]
In spite of the critical location of these tumors, with an anterior or anterolateral extension to the spinal cord and a relationship with vital neural structures and the VA, surgery for cervical spinal schwannoma is usually very successful. If the anatomy of the tumor in relation to normal structures in the vicinity is appropriately understood, then surgery in these formidable-looking tumors is relatively uncomplicated.[234] In our case we did not face any instability.
In our case, there was huge lateral and down ward extension of tumor in comparison with intraspinal portion and intraspinal part of the tumor was much smaller than the extraspinal part which was very large. Lateral portion of tumor could be palpated through lower part of posterior triangle. Moreover intervertebral foramen was enlarged by the tumor, at the same time we had the option to enlarge the foramen more during operation if it would needed. So we decided to remove the tumor through anterior-lateral interscalene transforaminal approach rather than posterolateral approach. Here posterolateral approach could lead to incomplete tumor removal for huge lateral and inferior paraspinal extension (along with tumor consistency).
Conclusion
Anterolateral interscalene transforaminal approach can be an effective and safe alternative to posterior-lateral approach in lower cervical spinal schwannomas with large paraspinal extension in selected cases.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Neoplasms of the peripheral nerves. In: Wilkins RH, Rengachary SS, eds. Neurosurgery (2nd ed). New York: McGraw-Hill; 1996. p. :3217-23.
- [Google Scholar]
- Surgical management of dumbbell tumors of the cervical spine. Neurosurgery. 1996;38:294-300.
- [Google Scholar]
- Neurinomas of the first two cervical nerve roots: A series of 42 cases. J Neurosurg. 1995;82:917-23.
- [Google Scholar]
- Dumbbell C2 schwannomas involving both sensory and motor rootlets: Report of two cases. Neurosurgery. 2003;53:436-40.
- [Google Scholar]
- Surgery of spinal nerve sheath tumors with special reference to neurofibromatosis. Neurosurgery. 1998;42:279-90.
- [Google Scholar]
- Anterolateral approach without fixation for resection of an intradural schwannoma of the cervical spinal canal: Technical note. Neurosurgery. 2009;65:1178-81.
- [Google Scholar]
- Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559-62.
- [Google Scholar]
- Spinal neurofibromas: A report of 66 cases and a comparison with meningiomas. Neurosurgery. 1986;18:331-4.
- [Google Scholar]
- Retrospective analysis of peripheral nerve sheath tumors of the second cervical nerve root in 60 surgically treated patients. J Neurosurg Spine. 2008;8:129-34.
- [Google Scholar]
- High cervical neurinoma (C1/C2) diagnosed falsely as multiple sclerosis because of trigeminal neuralgia. Arch Psychiatr Nervenkr. 1979;227:33-7.
- [Google Scholar]
- Surgical strategy for cervical dumbbell tumors based on a three-dimensional classification. Spine. 2004;29:E10-4.
- [Google Scholar]
- Results of surgical treatment of cervical dumbbell tumors: Surgical approach and development of an anatomic classification system. Spine. 2009;34:1307-14.
- [Google Scholar]
- Lateral interscalenic approach for tumors of the cervical intervertebral foramina (author's transl) Neurochirurgie. 1980;26:165-70.
- [Google Scholar]
- Surgical consideration of the intraspinal component in extradural dumbbell tumors. Surg Neurol. 2008;70:98-103.
- [Google Scholar]
- Benign spinal nerve sheath tumors: Their occurrence sporadically and in neurofibromatosis types 1 and 2. J Neurosurg. 1991;74:248-53.
- [Google Scholar]
- Cervical neuromas with extradural components: Surgical management in a series of 57 patients. Neurosurgery. 1997;41:813-22.
- [Google Scholar]






