Translate this page into:
Relationship between Pelvic Alignment and Weight-bearing Asymmetry in Community-dwelling Chronic Stroke Survivors
Address for correspondence: Mr. Karthikbabu S, Department of Physiotherapy, School of Allied Health Sciences, A Constituent College of Manipal University, Manipal Hospital, HAL Airport Road, Bengaluru - 560 017, Karnataka, India. E-mail: karthikbabu78@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Purpose:
Altered pelvic alignment and asymmetrical weight bearing on lower extremities are the most common findings observed in standing and walking after stroke. The purpose of this study was to find the relationship between pelvic alignment and weight-bearing asymmetry (WBA) in community-dwelling chronic stroke survivors.
Materials and Methods:
This cross-sectional study was conducted in tertiary care rehabilitation centers. In standing, the lateral and anterior pelvic tilt angle of chronic stroke survivors was assessed using palpation (PALM™) meter device. The percentage of WBA was measured with two standard weighing scales. Pearson correlation coefficient (r) was used to study the correlation between pelvic tilt and WBA.
Results:
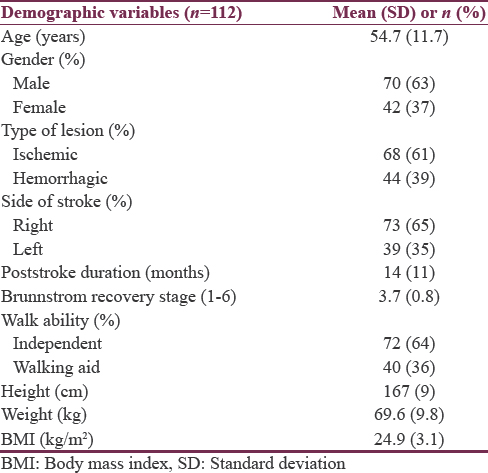
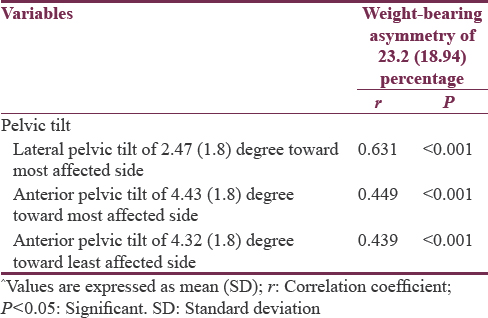
Of 112 study participants, the mean (standard deviation) age was 54.7 (11.7) years and the poststroke duration was 14 (11) months. The lateral pelvic tilt on the most affected side and bilateral anterior pelvic tilt were 2.47 (1.8) and 4.4 (1.8) degree, respectively. The percentage of WBA was 23.2 (18.94). There was a high correlation of lateral pelvic tilt with WBA (r = 0.631; P < 0.001) than anterior pelvic tilt (r = 0.44; P < 0.001).
Conclusion:
Excessive lateral pelvic tilt toward the most affected side in standing may influence the weight-bearing ability of the ipsilateral lower extremity in community-dwelling chronic stroke survivors.
Keywords
Motor recovery
pelvic alignment
stroke
weight-bearing asymmetry
INTRODUCTION
Altered pelvic alignment and asymmetrical weight bearing onto lower limbs are the most common findings observed after stroke.[1] Ability to transfer weight on paralyzed lower extremity is a prerequisite for functional mobility skills such as rising from a chair,[2] reach-outs in standing[3] and walking.[1] Perceptual dysfunction, sensory loss, poor motor recovery of lower extremity, spasticity, muscular weakness, poor trunk control, and altered pelvic alignment could contribute for reduced weight acceptance on the most affected lower limb. Altered pelvic alignment due to poor trunk-pelvis dissociation or reduced hip muscular control acting around pelvis may account for asymmetric weight distribution onto most affected lower limb during gait in people with stroke.[4] It is believed that trunk muscular control at pelvis is the key contributing factor for balance ability, walking, and function after stroke.[56] The trunk muscles attached to pelvis provide core stability which is an essential component for normal postural alignment of the pelvis.[7] External oblique muscle, the largest muscle of abdomen, is responsible for core stability and forward tilting of the pelvis.[8] After stroke, the impairment of lower abdominal activity shall fix the pelvis tilted posteriorly in sitting, thus providing passive stability during upper trunk initiated forward movements.[9]
Furthermore, the pelvis was more oriented toward the most affected side in sitting, and this lateral pelvic tilt was correlated to poor trunk control. People who had excessive lateral pelvic tilt in sitting as measured by palpation (PALM™) meter present with poor dynamic sitting balance and worse lower limb motor recovery.[10] Likewise, photogrammetry method showed a strong relationship between the postural alignment of the pelvis in sitting and seated postural control early after stroke.[11] Although the pelvic instability poststroke is one of the attributes to weight-bearing asymmetry (WBA), how the altered pelvic tilt in standing affects the WBA is understudied. Hence, we attempted to test the pelvic tilt and its relationship to WBA in community-dwelling stroke survivors.
MATERIALS AND METHODS
This cross-sectional study was approved by the Research and Ethics Committee of Manipal University, Manipal. Community-dwelling chronic stroke survivors were recruited from two tertiary care rehabilitation centers and rural settings between June 2011 and May 2015. They were explained about the study procedure, and informed consent was obtained from them seeking their voluntary participation in the study. The inclusion criteria of the study were as follows: People with first-ever stroke, unilateral supratentorial ischemic or hemorrhagic lesion, ability to follow verbal commands, and walk 10 m with or without mobility aids. They were excluded from the study if they had unstable medical conditions, severe sensory impairment, visual field defect, and any other neurological or musculoskeletal disease affecting standing balance.
The pelvic alignment in standing was assessed by palpation meter (PALM™ device),[12] while the WBA[13] was tested using two standard weighing scales. The coin-toss method was used to determine the order of tests in each patient. Four qualified physical therapists administered both the pelvic tilt and WBA test measures. Between two test measures, each patient was seated to get 5 min rest to overcome the learning effects. The PALM™ device has been tested for its intra- and inter-rater reliability in measuring pelvic obliquity in people with stroke. To measure the pelvic alignment, each patient was instructed to stand straight with feet placed 30 cm apart. For measuring lateral pelvic tilt, the therapist stood behind the patient and placed the caliper tips at the highest part of iliac crests. The therapist stood by the side of the patient and placed the caliper tips at anterior superior iliac spine and posterior superior iliac spine to assess forward pelvic tilt. The angle of inclination was read off to the nearest degree from the inclinometer.[14] The actual body weight of patient was recorded using standard weighing scale before testing weight asymmetry. In clinical practice, standing on two standard weighing scales is the feasible and reliable mode of evaluating unequal limb loading on feet after stroke. Two standard weighing machines were validated using metal weights. Two weighing machines were placed next to each other so that each patient stood on weighing scales with feet placed 30 cm wide apart. The patient was instructed to stand as erect as possible and to look straight. The weight on each scale was then recorded to calculate the percentage of WBA. The formula of WBA is = ([weight on most affected leg-weight on least affected leg]/total body weight) ×100.[13]
Statistical analysis
SPSS software version 16.0 (SPSS Inc. Chicago, USA) was used for data analysis. We assessed the demographic characteristics of all study participants using descriptive statistics. Pearson correlation coefficient (r) was used to find the relationship of lateral pelvic tilt and anterior pelvic tilt toward the most and least affected sides with the percentage of WBA in chronic stroke. The “r” is interpreted as very low (<0.20), low (0.20–0.39), moderate (0.40–0.59), high (0.60–0.79), and very high (0.80–1.00), respectively. The significance level was set at P < 0.05 and the P < 0.001 was considered highly statistically significant. The scattergram plotted in Figures 1-3 shows the degree of pelvic tilt and its relation to WBA in chronic stroke.
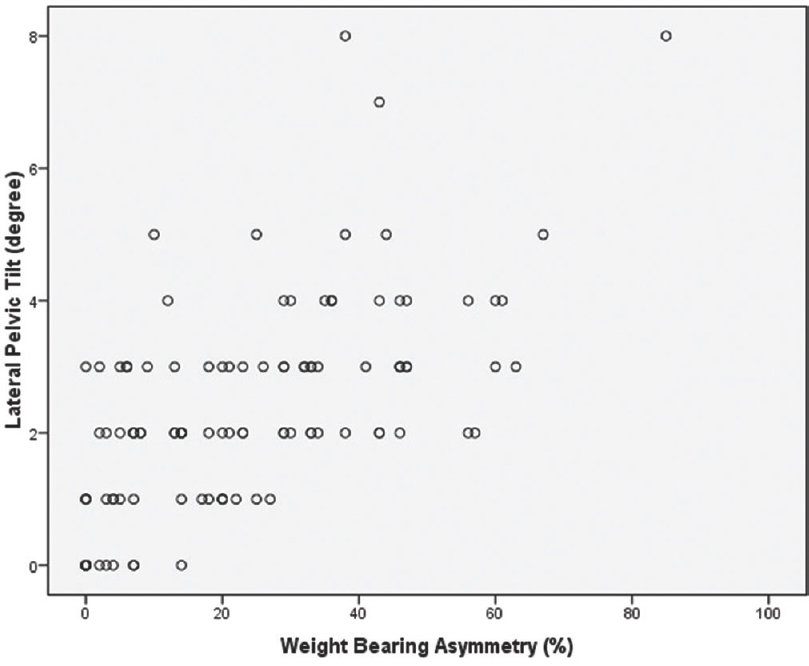
- Correlation between lateral pelvic tilt (degree) and weight-bearing asymmetry (%)
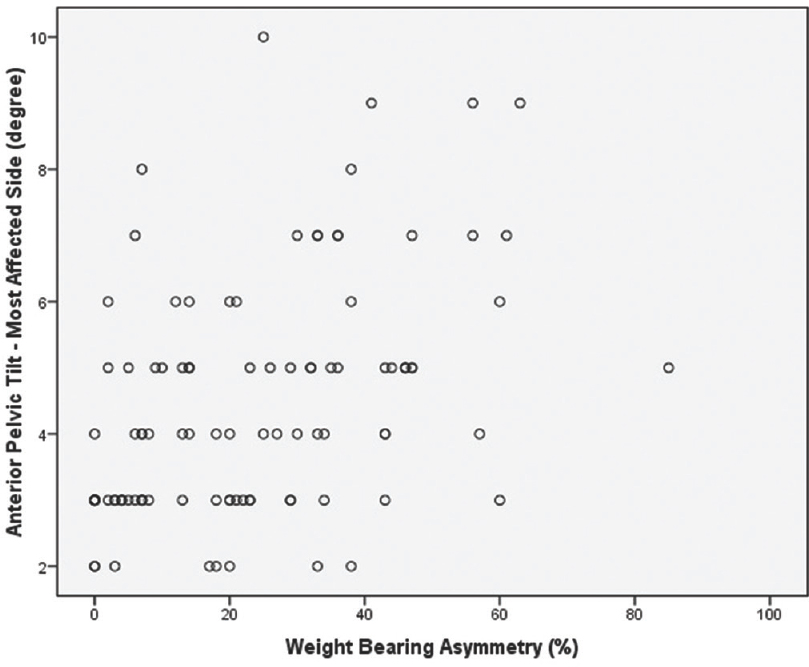
- Correlation between anterior pelvic tilt toward most affected side (degree) and weight-bearing asymmetry (%)
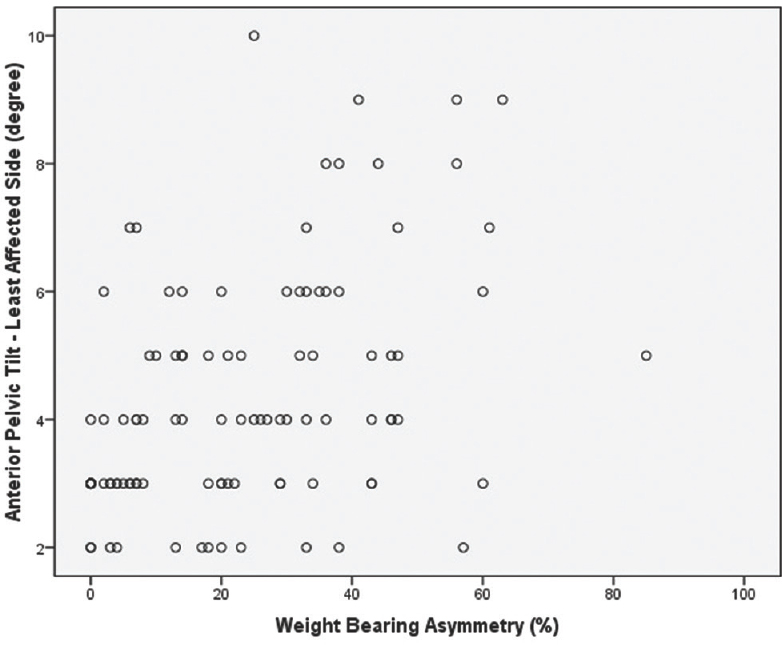
- Correlation between anterior pelvic tilt toward least affected (degree) and weight-bearing asymmetry (%)
RESULTS
One hundred and twelve patients with first-ever stroke were recruited in the study. The study included 70 males (63%) and 42 (37%) females with the mean age of 55 years and 14 months poststroke duration. This study included more number of patients with ischemic stroke (68 participants) than hemorrhagic stroke lesion (44). Thirty-nine patients (35%) had a left-sided stroke and 73 (65%) had a right-sided stroke. The mean lower limb motor recovery stage was 3.7 (0.8) as per Brunnstrom's stroke recovery grading. Seventy-two patients (64%) were walking without any mobility aid, while 40 patients (36%) were using either cane or tripod [Table 1]. On the measurement of pelvic alignment while in standing, it was tilted 2.47 (1.8) degree laterally toward the most affected side and 4.4 (1.8) degree anteriorly on the most and least affected sides. The percentage of WBA was 23.2 (18.94). The lateral pelvic tilt was highly correlated to WBA (r = 0.631; P < 0.001) than anterior pelvic tilt (r = 0.44; P < 0.001) [Table 2 and Figures 1-3].
DISCUSSION
The purpose of the study was to test the relationship between pelvic alignment and percentage of WBA in community-dwelling chronic stroke survivors. The worse lateral pelvic tilt angle on the most affected side was highly correlated to WBA (r = 0.631) compared to anterior pelvic tilt (r = 0.44). We believe that the poor muscular control of trunk and hip could be the reason for altered pelvic alignment in standing. This was supported by the recent work in which the lateral tilt toward the most affected side and anterior pelvic tilt in standing were moderately correlated to trunk control, and these correlations were high in chronic stroke patients with better lower limb motor recovery.[15]
Excessive lateral pelvic tilt on the most affected side could be one of the key factors for WBA in stroke. While in standing, the normal side–side pelvic alignment is controlled by the activity of hip abductors along with trunk control. Kirker et al.[16] stated that the impaired recovery pattern of hip abductor and adductor in standing after stroke is majorly responsible for side to side balance stability. The muscles of the lower trunk and hip working onto pelvis in anterior-posterior direction seem to be vital for activation of hip abductor and trunk side flexor during side-to-side weight shifts. Such muscular coordination is required for dynamic pelvic stability, thus allowing better weight-bearing symmetry after stroke. On measuring the center of pressure displacement during forward trunk bending and reaching in people after stroke, Chern et al.[3] observed less pressure distribution toward most affected side even the task demand was high. Posturography analysis revealed that balance ability after stroke as measured by Berg balance scale was strongly correlated to lateral weight shift ability than anterioposterior weight shifts.[17] A recent cross-sectional study by Pathak et al.[10] found an excessive lateral pelvic tilt in sitting and was related to lateral sitting balance control recovery in stroke. It has always been a focus for physical therapists working with people after stroke to enhance weight transfer ability toward the most affected side. Trunk exercise protocol emphasizing the weight-shift training in patients with chronic stroke also showed beneficial effects on functional balance ability.[18]
In the current study, we observed more anterior pelvic tilt on the most and least affected sides and was moderately correlated to WBA. Since trunk is bilaterally innervated and biomechanically connected to linea alba with its myofascial connections, any unilateral brain lesion typically affects the entire abdominal muscles, in turn, influences the position of both anterior superior iliac spines. Nevertheless, the posterior myofascial connections of gluteus maximus extending to thoracolumbar fascia along with anterior myofascial sequences of the abdominal wall are also important for anterioposterior pelvic stability. Several assessment methods confirmed the involvement of trunk on both sides after stroke.[19] Following stroke, forward leaning posture with anteriorly tilted pelvis is common and this atypical postural alignment was correlated to trunk and balance dysfunction.[20] This suggests that pelvic stability in forward-backward direction is well coordinated by trunk-pelvic and pelvis-hip dissociation. It is interesting to note that pelvis plays a role of the trunk in sitting whereas it is mainly a part of the lower extremity in standing. In sitting, the forward inclination of the trunk in sagittal direction was assisted by hip extensors, whereas the sideways movement of the body was not controlled by leg muscles, but only by trunk muscles. However, people with worse lower trunk control shall fix the pelvic backward and can translate the body weight forward by excessively flexing upper trunk. Furthermore, the weight-bearing center of pressure values on feet as measured by force plates was less in people poststroke compared to age-matched healthy people suggesting that asymmetrical weight bearing is always an issue during many of the functional tasks.[9] People poststroke seem to be relying on anterioposterior balance recovery than lateral balance recovery warranting stroke rehabilitation strategies toward improving lateral pelvic stability and symmetrical weight bearing. The amount of pelvic rotation, a major postural deviation observed in transverse plane poststroke, was not studied in this study due to its methodological limitations.
CONCLUSION
The percentage of WBA is majorly affected by lateral pelvic alignment than anterior-posterior alignment in community-dwelling chronic stroke survivors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to all the study participants.
REFERENCES
- Trunk kinematics in hemiplegic gait and the effect of walking aids. Clin Rehabil. 1999;13:295-300.
- [Google Scholar]
- Muscle strength and weight-bearing symmetry relate to sit-to-stand performance in individuals with stroke. Gait Posture. 2005;22:126-31.
- [Google Scholar]
- Dynamic postural control during trunk bending and reaching in healthy adults and stroke patients. Am J Phys Med Rehabil. 2010;89:186-97.
- [Google Scholar]
- Gait asymmetry in community-ambulating stroke survivors. Arch Phys Med Rehabil. 2008;89:304-10.
- [Google Scholar]
- Impact of trunk control on balance and functional abilities in chronic stroke patients. Egypt J Neurol Psychiatry Neurosurg. 2014;51:327-31.
- [Google Scholar]
- Correlation of trunk impairment with balance in patients with chronic stroke. NeuroRehabilitation. 2013;32:323-5.
- [Google Scholar]
- The Pelvic Girdle. An Integration of Clinical Expertise and Research (3rd ed). Edinburgh: Churchill Livingstone; 2004.
- The effects of core stability strength exercise on muscle activity and trunk impairment scale in stroke patients. J Exerc Rehabil. 2013;9:362-7.
- [Google Scholar]
- Dynamic analysis of trunk flexion after stroke. Arch Phys Med Rehabil. 2004;85:1619-24.
- [Google Scholar]
- The relationship between pelvic alignment and trunk control in stroke subjects: A cross-sectional study. Int J Res Med Sci. 2015;2:1483-7.
- [Google Scholar]
- Relationship between postural alignment in sitting by photogrammetry and seated postural control in post-stroke subjects. NeuroRehabilitation. 2014;35:181-90.
- [Google Scholar]
- Intratester and intertester reliability of the palpation meter (PALM) in measuring pelvic position. J Man Manipulative Ther. 1998;6:130-6.
- [Google Scholar]
- Reliability, agreement, and validity of digital weighing scale with MatScan in limb load measurement. J Rehabil Res Dev. 2014;51:591-8.
- [Google Scholar]
- Intra-rater and inter-rater reliability of the palpation meter (PALM™) device in stroke. Int J Med Health Sci. 2016;5:270-80.
- [Google Scholar]
- Pelvic alignment in standing and its relationship with trunk control and motor recovery of lower limb after stroke. Neurol Clin Neurosci 2016 Published ahead of print
- [Google Scholar]
- Changing patterns of postural hip muscle activity during recovery from stroke. Clin Rehabil. 2000;14:618-26.
- [Google Scholar]
- Posturographic assessment of sitting balance recovery in the subacute phase of stroke. Gait Posture. 2008;28:507-12.
- [Google Scholar]
- Weight-shift training improves trunk control, proprioception, and balance in patients with chronic hemiparetic stroke. Tohoku J Exp Med. 2014;232:195-9.
- [Google Scholar]
- A review on assessment and treatment of the trunk in stroke: A need or luxury. Neural Regen Res. 2012;7:1974-7.
- [Google Scholar]
- Postural alignment is altered in people with chronic stroke and related to motor and functional performance. J Neurol Phys Ther. 2014;38:239-45.
- [Google Scholar]






