Translate this page into:
Psychiatric Comorbidity in Children with Epilepsy: A Cross-sectional 5 Years Rural Prevalence Study
Address for correspondence: Dr. Ambrish Sanjay Dharmadhikari, Room No. 305, RMO Quarter, HBTMC & Dr. R. N. Cooper Municipal General Hospital, Mumbai, Maharashtra, India. E-mail: ambrish30@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Epilepsy is one of the most common chronic neurological disorders. In children, it has long debilitating course and is associated with comorbidities including psychiatric comorbidity. To tackle this burden of comorbidities, we must know the extent of problem. Hence, there is a need for estimation of prevalence of psychiatry disorder in children with epilepsy.
Aim:
The present study was aimed at measuring the prevalence of various psychiatry disorders among children suffering from epilepsy.
Settings and Design:
Cross-sectional chart review.
Methodology:
We reviewed case record files of all patients with a diagnosis of epilepsy in the age group of 9–17 years. Chart review was done for 5 years, May 1, 2007, to April 30, 2012. A total of 718 patients record were included in the study after satisfying inclusion criteria and excluding nonepilepsy diagnosis.
Statistical Analysis:
Statistics was done using Statistical Package for Social Sciences (SPSS 18.0). Descriptive statistics were used to calculate the result, Chi-square and Mann–Whitney U-test used wherever applicable.
Results:
The prevalence of childhood psychiatric disorder among children with epilepsy found to be 31.2%. We also found that having a partial component (73.21%, n = 164) in seizure has more chances of psychopathology in comparison to generalized seizure (8.1%, n = 18). Among them, those having a partial component with generalization (66.96%, n = 150) had a greater prevalence of psychopathology. Mental retardation was most common psychiatric disorder among psychopathology followed by manic/depressive illness (unipolar) followed by unspecified nonorganic psychosis.
Conclusion:
From our study, we demonstrate the significant mental health needs of children with epilepsy. The evident high prevalence of psychiatry disorder emphasizes the need for psychopathology assessment and treatment as a part of any comprehensive epilepsy clinic.
Keywords
Children
epilepsy
prevalence
psychiatry comorbidity
INTRODUCTION
Epilepsy is one of the most common chronic neurological disorders. Epilepsy is defined by the International League Against Epilepsy[1] as a chronic neurological condition, characterized by recurrent seizures.[2] Fifty million people have epilepsy worldwide of which 33 million are children. Importantly, 80% of the affected population resides in developing world.[34] Epilepsy is commonly associated with behavioral changes[5] and is the single largest neurological problem facing developing countries today. While assessing psychopathology, studies mainly used dimensional measures[678] to describe problem which pose problem for clinician for treatment approach. Very few studies[9] used categorical measure for assessing psychopathology which led to better understanding of problem and management.
In developing countries like India due to large burden of patient population on epileptologist, the associated problems are neglected leading to incomplete treatment and increased morbidity.[4] Hence, there is a need for estimation of prevalence of psychopathology in children with epilepsy, to define the problem and describe unmet needs of children with epilepsy. Till date, studies in India used dimensional measure[10] for identifying psychopathology. To the best of our knowledge, this is the first study in India estimating the prevalence of psychopathology in children with epilepsy using categorical measure.
METHODOLOGY
The present study was conducted at the Epilepsy Clinic of Central Institute of Psychiatry, Kanke between July 2012 and January 2013. Epilepsy clinic caters to rural population of Jharkhand. On any given day, the new patient is interviewed thoroughly by taking detailed history and examination. Focus is always kept on both neurological and psychological aspects. Diagnosis is made by two independent psychiatrist. For diagnosis of Epilepsy International League Against Epilepsy classificatory system is used. While classifying psychiatry diagnosis International Classification of Disorder-10[11] is used. All collected data are collected on institute designed case record file, and it is stored for future follow-up.
In this study, we reviewed case record files of all patients diagnosed of epilepsy within age group of 9–17 years. Chart review was done for 5 years, May 1, 2007, to April 30, 2012. A total of 841 case record files satisfying inclusion and exclusion criteria were included for review. Out of which 123 were excluded from study considering diagnosis other than epilepsy such as dissociative convulsion (n = 115), vasovagal syncope (n = 5), or migraine (n = 3). A total of 718 case record files were carefully examined, and finding was recorded in predesigned sociodemographic and clinical data sheets. Statistics was done using SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc. Descriptive statistics were used to calculate result, Chi-square, and Mann–Whitney U-test used wherever applicable.
RESULTS
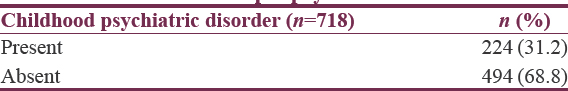
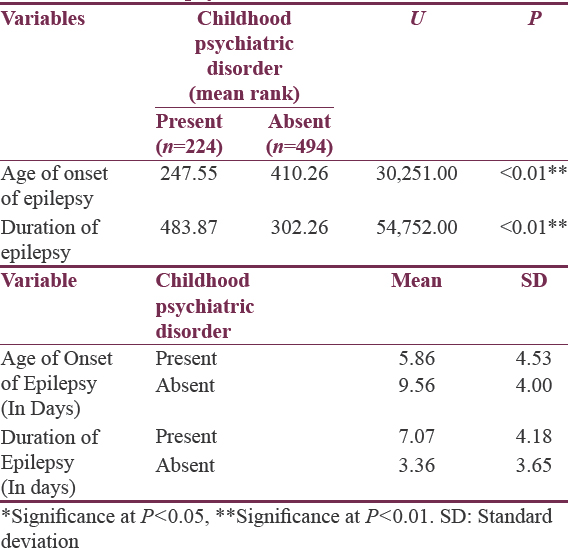
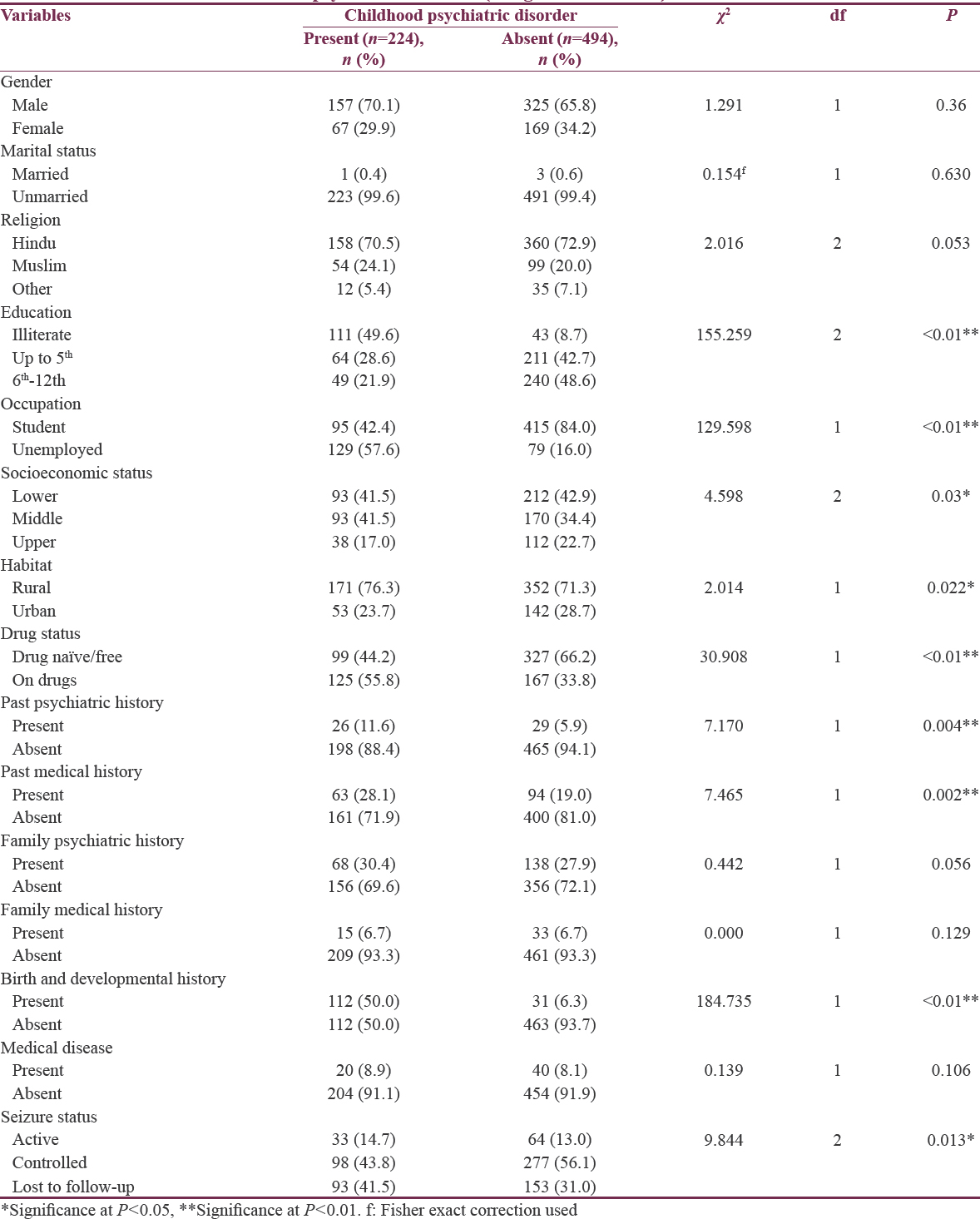
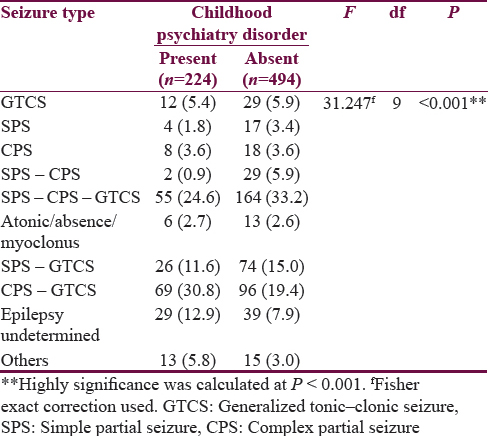
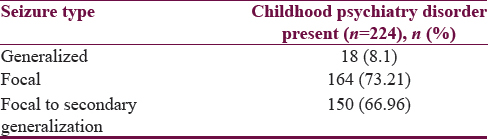
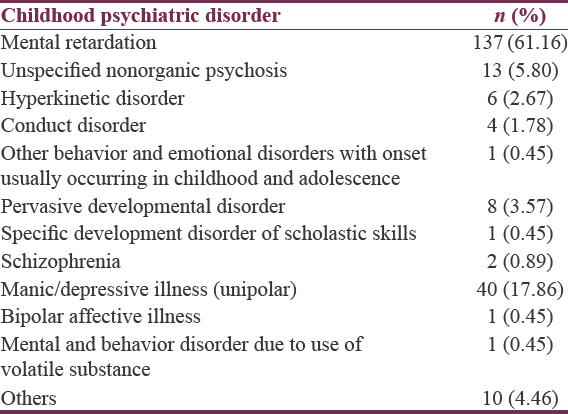
Table 1 shows the prevalence of childhood psychiatric disorder among children with epilepsy found to be 31.2%. Table 2 shows similar mean age of children in both groups of with or without psychopathology. While there is earlier age of onset of epilepsy in children with epilepsy having psychopathology than children with epilepsy without psychopathology. Children with epilepsy having psychopathology had a longer duration of epilepsy than children with epilepsy without psychopathology. Table 3 shows significant differences in education and occupation between children with epilepsy with and without epilepsy, majority of children were found to be illiterate leading to unemployment. Furthermore, a significant difference was present in socioeconomic status and habitat, which suggested the majority of children, belonged to lower socioeconomic strata, and also from the rural area. There was a significant difference in drug status of children with epilepsy with psychopathology and without psychopathology. The majority of children with epilepsy with psychopathology were on drugs, in contrast majority of children with epilepsy without psychopathology were drug-free. There was a significant difference in past psychiatric history and past medical history of children with epilepsy when compared to children with epilepsy without psychopathology. Signifying majority of children with epilepsy with psychopathology had positive past psychiatric and medical history. There was a significant difference in birth and developmental history, suggesting majority of children with epilepsy with psychopathology had significant birth and developmental history. In addition, significant difference noted among children with epilepsy with psychopathology and children with epilepsy without psychopathology about seizure status. Table 4a shows the prevalence of psychiatric disorder among seizure type, showing children with epilepsy with psychopathology, had complex partial seizure (CPS) to secondary generalization as most common seizure type followed by Simple partial seizure (SPS) to CPS to secondary generalization followed by epilepsy undetermined followed by SPS to secondary generalization, and SPS to CPS being most uncommon type. Table 4b shows that having a partial component (73.21%, n = 164) in seizure has more chances of psychopathology in comparison to generalized seizure (8.1%, n = 18). Among them, those having a partial component with generalization (66.96%, n = 150) had a greater prevalence of psychopathology. Table 5 shows distribution of psychopathology among different psychiatric disorder, signifying, mental retardation was most common psychiatric disorder among psychopathology followed by manic/depressive illness (unipolar) followed by unspecified nonorganic psychosis followed by pervasive developmental disorder followed by hyperkinetic disorder followed by conduct disorder followed by schizophrenia [Figure 1].
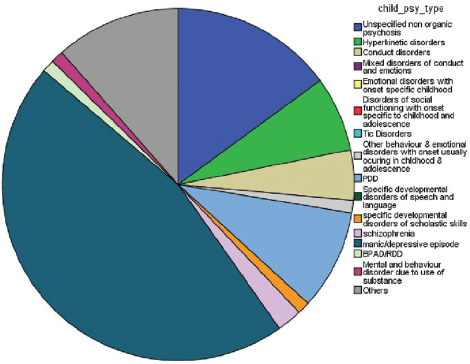
- Distribution of different psychiatric disorder (excluding mental retardation) among children with psychopathology (n = 87)
DISCUSSION
Sample characteristics
In our study, the advantage of a categorical measure is its ability to allow determination of a specific diagnosis that can be used to guide treatment where a dimensional measure fails to specify a diagnosis. There is no study so far which has used a retrospective design, and there are very few studies which have utilized only categorical measures of psychopathology. Caplan et al.[12] used structured diagnostic interviews and 60 children with complex partial epilepsy and 40 children with generalized epilepsy were included in their study. Similarly, Thome-Souza et al.[13] evaluated 55 children with epilepsy using a structured interview and Jones et al.[14] identified 53 children aged 8–18 years with recent onset epilepsy to characterize the spectrum of comorbid psychiatric disorder using the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV).[15] Three studies have combined dimensional and categorical measures of behavior in children with epilepsy. Caplan et al.[16] evaluated 101 children with complex partial epilepsy using both the Child Behavior Checklist (CBCL) and a structured interview for categorical diagnosis; Davies et al.[9] in a nationwide epidemiological study identified 67 children with epilepsy to assess the rates of psychiatric disorder in children aged 5–15 years and lastly Dunn et al.[17] evaluated 173 children in the age range of 9–14 years with epilepsy using the Child/Adolescent Symptom Inventory in addition to categorical measures. Thus, the sample size selected for our study was adequate and larger in comparison to previous studies recording the prevalence of epilepsy using categorical measures. We studied prevalence in hospital setting, which caters to needs of rural areas of Jharkhand state. The availability of well-maintained case record files at institute was reason for choice of hospital-based prevalence than community prevalence.
Clinical correlates
Our data revealed that the children with comorbid psychiatry illness had a significantly earlier onset of epilepsy and epilepsy lasting for a longer duration in comparison to children without psychopathology (P < 0.001) [Table 2]. Comorbidity not only add up burden to illness but also increase uncontrolled epilepsy duration, leading to increased morbidity and disability affected life years. A study by Datta et al.[10] reported period of uncontrolled seizure duration lasting for >3 years. It is worthwhile to consider that recurrent seizures have high chances of developing comorbidity.[181920] Psychiatry and medical history is a strong predictor of the development of epilepsy in children, especially febrile convulsions in early part of life and head injury.[2122] Our sample reported 7% had psychiatric history and 29% had family psychiatry history, against 21% and 7% reported past medical and medical family history, respectively. The majority of those who had positive history reported febrile convulsion and head injury. Making them leading causative factors for epilepsy in later life.
Prevalence
The prevalence psychiatry comorbidity in children with epilepsy was found to be 31.2% [Table 1]. A similar finding was seen by Davies et al.[9] where DSM-IV-based psychiatric diagnoses were present in 37% of children with epilepsy. A recent meta-analysis of 46 studies in 2434 children with epilepsy measuring psychiatric comorbidity using the CBCL[8] has found comorbidity in range of 16%–77%.[678]
Epilepsy type
Comorbidity of psychiatry disorder in epilepsy is not uniform, but it varies with its different types of epilepsy. In our sample, most common seizure type in epilepsy associated with psychiatric comorbidity was CPS leading to a secondary generalization (generalized tonic–clonic seizures [GTCS]) (30.8%, n = 69). Against SPS to CPS (0.9% n = 2) was the most uncommon type of epilepsy to be associated with psychiatric comorbidity. While SPS to CPS to GTCS (24.6%, n = 55) and GTCS (8.1% n = 18) was in middle of causation list. It also was noted that having a partial component (73.21%, n = 164) in seizure had more chances of psychopathology in comparison to generalized seizure (8.1%, n = 18). Patients having a partial component with generalization (66.96%, n = 150) had a higher occurrence of psychiatric comorbidity. Many authors supported this claim in the past.[12132324]
Comorbidity
Affective illness was reported in 17.86% of children with epilepsy. This picture was also seen in various studies conducted during the past 10 years in community or university-affiliated settings, where depression and anxiety were found in 16%–31% of children and adolescents with epilepsy.[19242526] Similarly, studies using structured psychiatric interview like K-SADS, DSM-IV-based mood and anxiety disorder diagnoses have reported a prevalence of 25%–36.4% in children and adolescents with epilepsy.[13192425]
Psychosis as a comorbidity in children with epilepsy was reported higher when seen in children with CPS, prevalence reported to be 10%.[12] However, this might be inflated rates as other types of seizure were not included in study. Our study which includes all types of seizure had 6.69% of children with epilepsy with psychosis as comorbidity [Table 5].
Hyperkinetic disorder (attention deficit hyperactivity disorder [ADHD] in DSM-5) was diagnosed in 2.67% of children with epilepsy [Table 5]. Other studies using clinical samples and DSM-IV based criteria for ADHD have found symptoms of ADHD in 14%–38% of children with epilepsy.[1213252728] The probable reason for the mismatch is that in the majority of these studies, reporting of ADHD disorder was based on a dimensional measure which may not fulfill all criteria as per DSM-IV or DSM-5. In contrast, we used strict criteria to fulfill diagnosis. Patients with subsyndromal symptoms were not included in the study.
The prevalence Autism spectrum disorder was found to be 3.57% [Table 5]. A population-based epidemiological study reported pervasive developmental disorders in 16% of children with complicated epilepsy (additional neurological deficits) and 0% in children with uncomplicated epilepsy.[9] Considering that our sample constituted both complicated and uncomplicated epilepsy, which explains the difference in prevalence rate. In addition, in a clinic-based survey of children with epilepsy, ASD was found in only 9% of the population,[13] which again sways pendulum in our reported prevalence.
Intellectual disability was found to be comorbid in 21.2% children with epilepsy in total population. A similar picture was also seen in epidemiological studies which demonstrate significantly higher rates of comorbidity in children with epilepsy and mental retardation than in children with epilepsy having an average IQ.[929]
The prevalence of specific development disorder of scholastic skills was found to be 0.45%. This is very less when compared to a population-based study which documented reading disorders in 18.6%, writing disorders in 17.6%, and mathematics disorder in 14.7% children with epilepsy.[30] Illiteracy, lower socioeconomic strata, lack of awareness are major reason for discrepancy. Another reason could be due to sample constitution; our sample had one-fifth of children with intellectual disability.
CONCLUSION
The goal of a comprehensive epilepsy clinic should be to provide assessment and treatment not only for seizures but also for the psychiatric problems experienced by the child with epilepsy. This study demonstrates the significant mental health needs of children with epilepsy. The high prevalence of problems emphasizes the need for psychopathology assessment and treatment as a part of any comprehensive epilepsy clinic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Incidence of childhood and adolescence epilepsy: A community-based prospective study in the province of Ferrara and in Copparo, Italy, 1996-2005. Eur J Neurol. 2012;19:312-6.
- [Google Scholar]
- Comparison of key informant and survey methods for ascertainment of childhood epilepsy in West Bengal, India. Int J Epidemiol. 1998;27:672-6.
- [Google Scholar]
- Impact of epilepsy in adolescence: A UK controlled study. Epilepsy Behav. 2005;6:556-62.
- [Google Scholar]
- Psychosocial problems and seizure-related factors in children with epilepsy. Dev Med Child Neurol. 2006;48:213-9.
- [Google Scholar]
- Family predictors of psychopathology in children with epilepsy. Epilepsia. 2006;47:601-14.
- [Google Scholar]
- A population survey of mental health problems in children with epilepsy. Dev Med Child Neurol. 2003;45:292-5.
- [Google Scholar]
- Behaviour problems in children and adolescents with seizure disorder: Associations and risk factors. Seizure. 2005;14:190-7.
- [Google Scholar]
- The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- Psychopathology in pediatric complex partial and primary generalized epilepsy. Dev Med Child Neurol. 1998;40:805-11.
- [Google Scholar]
- Which factors may play a pivotal role on determining the type of psychiatric disorder in children and adolescents with epilepsy? Epilepsy Behav. 2004;5:988-94.
- [Google Scholar]
- Clinical assessment of Axis I psychiatric morbidity in chronic epilepsy: A multicenter investigation. J Neuropsychiatry Clin Neurosci. 2005;17:172-9.
- [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders (DSM). Washington, DC: American Psychiatric Association; 1994. p. :143-7.
- Psychopathology and pediatric complex partial seizures: Seizure-related, cognitive, and linguistic variables. Epilepsia. 2004;45:1273-81.
- [Google Scholar]
- Teacher assessment of behaviour in children with new-onset seizures. Seizure. 2002;11:169-75.
- [Google Scholar]
- Psychosocial adjustment of children with chronic epilepsy and their families. Dev Med Child Neurol. 1991;33:201-15.
- [Google Scholar]
- Symptoms of depression and anxiety in pediatric epilepsy patients. Epilepsia. 1998;39:595-9.
- [Google Scholar]
- Recurrent seizures and behavior problems in children with first recognized seizures: A prospective study. Epilepsia. 2002;43:1564-73.
- [Google Scholar]
- National general practice study of epilepsy: Recurrence after a first seizure. Lancet. 1990;336:1271-4.
- [Google Scholar]
- Long-term risk of developing epilepsy after febrile seizures: A prospective cohort study. Neurology. 2012;78:1166-70.
- [Google Scholar]
- Behavior problems in children before first recognized seizures. Pediatrics. 2001;107:115-22.
- [Google Scholar]
- Behavior and mental health problems in children with epilepsy and low IQ. Dev Med Child Neurol. 2003;45:683-92.
- [Google Scholar]
- Components of attention in children with complex partial seizures with and without ADHD. Epilepsia. 1999;40:211-5.
- [Google Scholar]
- Behavioral disorders in pediatric epilepsy: Unmet psychiatric need. Epilepsia. 2003;44:591-7.
- [Google Scholar]
- Psychiatric disorders in children and adolescents with mental retardation and active epilepsy. Arch Neurol. 1996;53:904-12.
- [Google Scholar]
- Learning disability: Occurrence and long-term consequences in childhood-onset epilepsy. Epilepsy Behav. 2004;5:937-44.
- [Google Scholar]






