Translate this page into:
Primary Myxoid Liposarcoma of the Upper Thoracic Spine in an Elderly Patient
Address for correspondence: Dr. Aristedis Rovlias, Department of Neurosurgery, Asclepeion General Hospital of Voula, 1 Vasileos Pavlou Street, 16 673, Voula, Athens, Greece. E-mail: arovlias@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Liposarcoma, one of the most common soft-tissue sarcomas, originates from primitive mesenchymal cells, and its diagnostic criteria have been well established. Myxoid liposarcoma is the second most common histological subtype, occurring more frequently during the fourth and fifth decades of life. There are only a few sporadic published cases of spinal liposarcomas, whatever primary or metastatic. We describe an unusual case of primary myxoid liposarcoma of the thoracic spine in a 79-year-old male, presented with a 2-month history of intractable dorsal pain and progressive weakness of lower limbs. Surgical treatment was performed with wide tumor resection, spinal cord decompression, and posterior instrumentation complemented by radiotherapy. Only one other case has been reported with this spinal localization in the literature. Despite its rarity, myxoid liposarcoma should be considered in the differential diagnosis of primary tumors of the thoracic spine.
Keywords
Liposarcoma
myxoid liposarcoma
primary spinal tumors
thoracic spine
INTRODUCTION
Liposarcoma, one of the most common soft-tissue sarcoma in adults, originates from primitive mesenchymal cells, rather than mature adipose tissue.[1] The most common sites of liposarcoma are thigh and femur. Myxoid liposarcoma is the second most common histological type, occurring more frequently between 40 and 60 years of age.[123] Primary or secondary spinal involvement is very rare, and only sporadic case reports have been published.[14567]
The aim of this study is to present an extremely rare case of primary myxoid liposarcoma of the thoracic spine in an elderly patient.
CASE REPORT
A 79-year-old male presented to the emergency department complaining of aggravating weakness of lower limbs and dorsal pain of 2 months duration. On admission, he was unable to stand and walk. Neurological examination revealed a 2/5 spastic paraparesis with a fifth thoracic sensory level. From his medical history, he was taking clopidogrel for chronic ischemic heart disease.
A computed tomography (CT) scan of the thoracic spine revealed a mixed-type extensive lytic lesion with radiolucent component and marginal sclerotic bone reaction on the T5 body vertebrae including right pedicle, lamina, and transverse processes with extraosseous extension to the adjacent paravertebral and epidural space [Figure 1a and b]. Further assessment by magnetic resonance imaging demonstrated an invasive inhomogeneous low-signal intensity on T1-weighted images and high-signal intensity on T2-weighted images infiltrative mass with diffuse heterogeneous gadolinium enhancement, spreading to the right paraspinal and epidural space with significant compression and displacement of the spinal cord at the aforementioned levels [Figure 2a and b]. Preoperative physical, laboratory, and imaging examination, including thorax CT scan, abdominal-pelvic CT scan, and bone scan, showed no evidence of tumor in other organs and confirmed the primary origin of the spinal tumor.
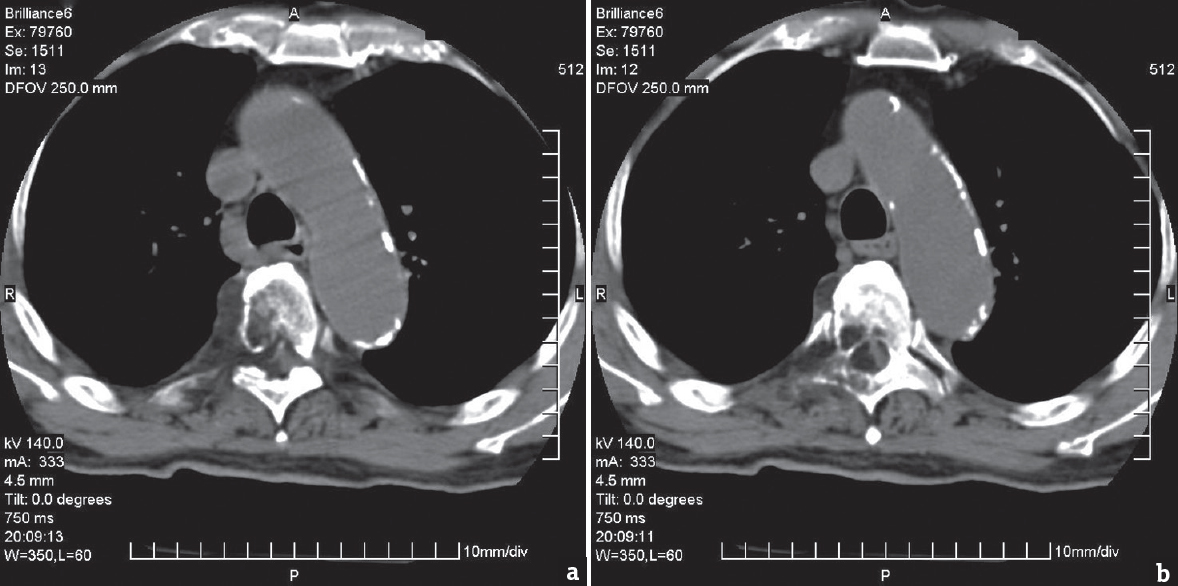
- A computed tomography scan axial imaging of the thoracic spine (a and b) demonstrated a mixed-type lesion with radiolucent component and marginal sclerotic bone in the right T5 vertebral body, pedicle, lamina, and transverse processes, with extension into the ipsilateral epidural and paravertebral space. Density measurements confirmed the fatty component of the tumor
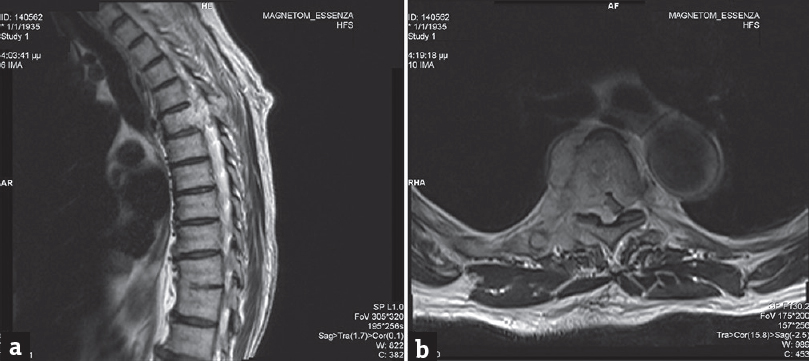
- Magnetic resonance imaging axial T2-weighted image (a) revealed a high-signal intensity lesion involving the right body and the posterior elements of T5 vertebra, with epidural and paravertebral involvement. Magnetic resonance imaging sagittal T2-weighted image (b) demonstrated the epidural extension of the lesion and spinal cord compression
Tumor resection was performed through a posterior approach. The patient underwent fourth and fifth wide thoracic laminectomy, with consecutive piecemeal subtotal excision of a yellowish-brown tumor as far as possible with the aid of the operating microscope. However, complete tumor resection was not possible due to the extensive invasion. The operative procedure was completed by a T3 to T7 posterior instrumentation.
Histopathological examination revealed a malignant mesenchymatic tumor with small round cells, stromal myxoid degeneration, focal hypercellularity and necrosis, and hypervascularity [Figure 3]. Immunohistochemical studies indicated a positive reaction for vimentin, S-100 protein, and CD34 staining. The Ki-67/MIBI proliferation index was 6.4%. Pathology was compatible with myxoid liposarcoma determined as grade II according to the French Federation of Cancer Centers Sarcoma Group grading system.
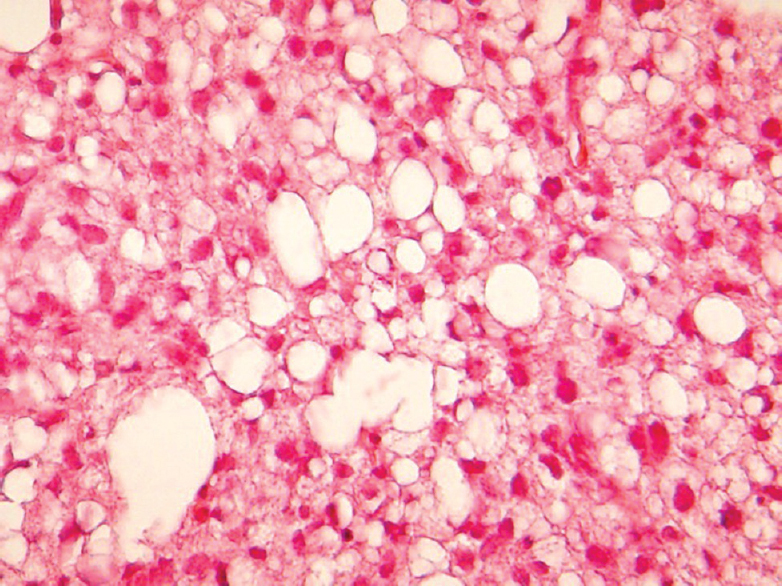
- Microscopic view of tumoral tissue shows a mixture of nonlipogenic mesenchymal cells and lipoblasts in a myxoid stroma (H and E, ×200)
The postoperative course was uneventful, with no functional neurological improvement, except a significant dorsal pain relief. One month later, the patient underwent palliative radiation therapy (45 Gy) and was referred to a rehabilitation center. At 7-month follow-up, the patient suffered gradual physical deterioration and died.
DISCUSSION
Liposarcoma is the most common soft-tissue tumor and accounts for approximately 20% of all mesenchymal malignancies.[2457]
Pleomorphic liposarcoma, the rarest form of liposarcoma, accounting for 5% of all liposarcomas, is an aggressive tumor and appears more often in the sixth and seventh decades of life.[8910] Myxoid liposarcoma is the second most common histological type, accounting for 30%–40% of cases, and occurring more frequently in younger patients between 40 and 60 years of age.[2] The most frequent sites of myxoid liposarcomas are buttocks, retroperitoneum, trunk, and proximal limb girdle, but primary spinal involvement is a rare entity.
Primary tumors of the spine are relatively infrequent lesions compared with metastatic disease, multiple myeloma, and lymphoma.[127] There are only a few sporadic published cases of spinal liposarcomas, whatever primary or metastatic. Their presentation is variable with an insidious clinical course until the presentation of neurological signs due to spinal cord compression.
One difficulty when discussing spinal liposarcoma is to decide which cases represent primary growths and which are metastatic. The criteria for this differentiation require a histologically proven liposarcoma arising within bone and at the same time having ruled out a metastatic lesion. The final diagnosis is based on the histopathological findings according to the criteria established by the WHO, and immunohistochemical analysis always needs to be performed to establish a certain diagnosis.[158]
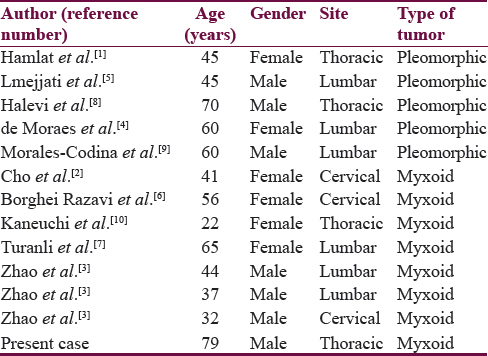
Our case report represents a true primary myxoid liposarcoma aroused within a thoracic vertebra with a proven negative metastatic workup in a 79-year-old patient, based on the histological features consistent with this diagnosis. A search of the literature revealed only seven cases of primary myxoid and five cases of primary pleomorphic liposarcoma of the spine. Among these seven cases, myxoid liposarcoma subtype showed an average of 42.4 years old [Table 1]. To the best of our knowledge, the present case is the second one of primary myxoid liposarcoma of the thoracic spine and the first reported case in the literature of primary myxoid liposarcoma of the spine in such elderly patient.
The epidemiological and pathological features of spinal liposarcomas are not clear because no large case series report treatment strategies and outcomes with long-term follow-up.[2] Although it is clear that complete surgical resection is the gold standard procedure for all spinal tumors,[7] in our patient, it was difficult to resect the tumor with an adequate margin through a posterior only approach due to its wide spreading. Thus, adjuvant palliative radiotherapy was performed for residual tumor remaining to prevent disease progression since myxoid liposarcomas have been regarded as radiosensitive tumors due to their specific vascularization.[1]
CONCLUSION
Primary myxoid liposarcoma of the spine is a very rare disease, with only seven cases reported till now in the literature. The thoracic spine is an unusual location for liposarcoma, even as metastasis and our report is the first case of primary myxoid liposarcoma detected on the thoracic spine in such advanced age. This study suggests that, in cases of suspected primary spinal tumors, myxoid liposarcoma should be considered in the differential diagnosis even in elderly patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Primary liposarcoma of the thoracic spine: Case report. Eur Spine J. 2005;14:613-8.
- [Google Scholar]
- Intradural involvement of multicentric myxoid liposarcoma. J Korean Neurosurg Soc. 2010;48:276-80.
- [Google Scholar]
- Surgical management of spinal liposarcoma: A case series of 7 patients and literature review. Eur Spine J. 2016;25:4088-93.
- [Google Scholar]
- Primary liposarcoma of the lumbar spine: Case report. Rev Bras Ortop. 2015;47:124-9.
- [Google Scholar]
- Primary epidural liposarcoma of the cervical spine: Technical case report and review of the literature. Interdiscip Neurosurg. 2015;2:1-5.
- [Google Scholar]
- Primary pleomorphic liposarcoma of the thoracic epidural space: Case report. Spine J. 2015;15:e71-5.
- [Google Scholar]
- Primary pleomorphic liposarcoma of the spine. Case report and review of the literature. Int J Surg Case Rep. 2016;25:114-9.
- [Google Scholar]
- Primary dumbbell-shaped epidural myxoid liposarcoma of the thoracic spine: A case report and review of the literature. Oncol Lett. 2016;11:1421-4.
- [Google Scholar]






