Translate this page into:
Prevalence of Psychiatric Illness among Residents of Old Age Homes in Northern India
Address for correspondence: Mr. Shamsi Akbar, Department of Geriatric Mental Health, KG Medical University, Lucknow, Uttar Pradesh, India. E-mail: shamsiakbar85@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
There are many factors which compelled older adults to live in old age homes (OAHs) and vulnerable to psychological problems. Studies reported high prevalence of mental health problems (20%–60%) among elderlies of OAHs. Therefore, the study was conducted to explore prevalence of psychiatric illness (PI) among residents of OAHs of Northern India.
Settings and Design:
The present study was conducted in OAHs of Districts Bareilly, Lucknow, Varanasi, Dehradun, and Haridwar, using cross-sectional descriptive study method. Sample Size were 306 (male – 98 [32.5%] and female n = 208 [68%]) residing in OAHs selected by means of purposive sampling.
Subjects and Methods:
Inclusion criteria: (a) older adults aged 60 years and above residing in OAHs and able to communicate. (b) Staying in OAHs for 6 months or more. (c) Able to understand comprehends and reply to questions and (d) Giving written informed consent. Exclusion criteria: (a) Residents who declined/not interested to participate in the study. (b) Residents having any sensory impairment/physical health problem which can impede the interview. Research tools were (i) a semi-structured pro forma, (ii) Hindi Mental Status Examination, (iii) Survey psychiatric assessment schedule, and (iv) Schedules for clinical assessment in neuropsychiatry-based clinical interview for diagnosis of PIs according to International Classification of Disease 10.
Statistical Analysis Used:
The quantitative data obtained was analyzed by means of frequency tables.
Results:
The results show overall prevalence of PI is 43% among residents of OAHs. The prevalence of PI was found to be higher among females compared to males. Depression was the most common among the residents of OAHs.
Conclusions:
There is an urgent need of trained professionals to provide professional help for highly prevalent psychiatric disorders among residents of OAHs.
Keywords
Depression
old age homes
prevalence
psychiatry
psychological problems
INTRODUCTION
Aging is a part of natural developmental process in the life of any living being. For human beings, it is not just a biological phenomenon; however, it has psychological and social implications too. With improved economic status and health-care facilities, the number of people living beyond age 60 years is rapidly increasing. Various authors agree on 65 years and above age as cutoff for defining old age[1]. In the developing country, every sixth person is over 65 years of age. In the next 30 years, it will be every fourth person. India, with 1.27 billion people is the second most populous country in the world and population growth rate at 1.58%, is predicted to have more than 1.53 billion people by the end of 2030. Demographers have presumed that by the year 2050 more than 40% of people would only be elders in India.[2] The enormous growth in the proportion of older adults in the country, change in family structure, and other contemporary changes in the psychosocial matrix and values often compel the elderly to live alone or to shift from their own homes to institutions and old age homes (OAHs).[3]
The residents living in OAHs often confront problems due to highly institutionalized, depersonalized, and bureaucratic atmosphere in OAHs. Elderly living in such homes face problems of adjustment with tight and rigid schedules, separation from the family, isolation from the social milieu, anxiety over adopting oneself to a new environment, and close encounters with death and ailment in the institutions. A recent study reported that misbehavior of children (29.8%) and lack of financial support (29.3%) were the most common reasons for living in OAHs.[4] All above factors make the older adults vulnerable to psychological problems. Studies indicate that the average prevalence of mental health problems among elderly is 41.3% in the community[5] and 64.4% living in OAHs.[6] In India, overall prevalence of psychiatric illness (PI) among elderly aged 60 years and above found 33.9%.[7] Depression was the most common psychiatric disorders in elderly living in OAHs. There is geographical (hills, plane, dessert, and sea), sociocultural (joint and nuclear families, different religions and their practices), vocational (farming, business, IT, fishing, unemployment, educational, retirement), and lifestyle (food habits, exercise, entertainment, clubs, and social service) diversity in India by different regions. Therefore, study findings of the other regions of the country cannot be generalized. Hence, this study was planned to find the prevalence of PI among residents of OAHs of different cities of the state of Uttar Pradesh and Uttarakhand in India which is situated in North region of the country based on a research work entitled “A Study of Psychiatric Morbidity, Quality of Life and Expectations of Inmates of OAHs in Northern India,” enrolled under PhD. Programme in the Department of Geriatric Mental Health, King George's Medical University Lucknow, approved by the Ethical Committee of King George Medical University. Only a part of above PhD thesis work is being presented in this paper.
Aim
The present study presents prevalence of PI among the residents of OAHs.
SUBJECTS AND METHODS
The present study was conducted on purposely selected 306 residents of OAHs in the Districts of Bareilly, Lucknow, Varanasi, Dehradun, and Haridwar fulfilling inclusion/exclusion criteria. Of them, 98 (32.5%) were male and 208 female (68%). Inclusion criteria: (a) older adults aged 60 years and above residing in OAHs and able to communicate. (b) Staying in OAHs since 6 months or more. (c) Be able to understand comprehend and reply to questions, and (d) Giving written informed consent. Exclusion criteria: (a) Residents who declined/not interested to participate in the study. (b) Residents having any sensory impairment/physical health problem which can impede the interview of the research tools: (i) A semi-structured pro forma (ii) Hindi Mental Status Examination (HMSE), (iii) Survey Psychiatric Assessment Schedule (SPAS), and (iv) Schedules for clinical assessment in neuropsychiatry (SCAN)-based clinical interview for the diagnosis of PIs according to the International Classification of Disease (ICD) 10-diagnostic criteria and research.
Procedure
A total number of OAHs in district Bareilly, Lucknow, Varanasi, Dehradun, and Haridwar were identified through help age India directory and local resources. There were two types of OAHs; 1. Private-in which inmates had to pay some amount per month, the other one was public type, i.e. free of cost. Permission was obtained for the present study from the administrative authority of identified OAHs. After getting permission from OAHs, data collection was done. Before collecting the data, written informed consent from all older adults was obtained. Socio-demographic details were obtained from the participants with help of semi-structured identification pro forma. HMSE was administered on included participants to screen cognitive Impairment. SPAS was used to screen the group of PI. Participants screened “in” on SPAS were further assessed through SCAN-based clinical interview for making specific diagnosis as per ICD-10 diagnostic criteria for research.
RESULTS
The quantitative data obtained was analyzed by means of frequency tables in the following order.
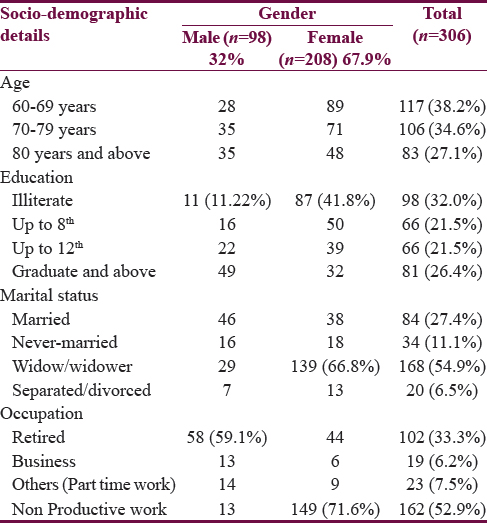
Gender-wise comparison sociodemographic characteristics of older adults living in old age homes
Table 1 shows a total number of 306 participants (98 male, 208 females) formed the sample of the study. Majority of the participants were in the age group of 60–69 years (38.2%), followed by 70–79 years (34.6%), and 80 years and above (27.1%). Mean age of the total sample was found to be 73.14 ± 9.002 years. Age wise there was no significant difference found between the male and female participants. Significant differences were found on the sociodemographic variables of education (P < 0.000), marital status (P < 0.000), and occupation (P < 0.000) between male and female participants. Their educational levels were as follows: illiterate were 32.0%, up to 8th standard were 21.5%, up to 12th standard were 21.5% followed by graduate and above at 26.4%. Marital status of the participants; 54.9% were widow/widower, followed by 27.4% who were married, 11.1% were never married, and 6.5% were separated/divorced. Their occupation levels; 52.9% were nonproductive workers followed by 33.3% who were retired, 7.5% were part-time workers, and 6.2% were in some kind of business. Sociodemographic details showed that most of the OAHs residents were females rather than males.
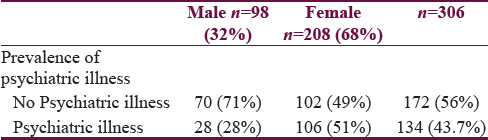
Prevalence of psychiatric illness among residents of old age homes
Table 2 shows that there was a significant difference (P < 0.000) between both sexes regarding the prevalence of PI. The prevalence of PI was more in females (51%) as compared to males (28%).
DISCUSSION
Sociodemographic status
Majority of the study participants were between 60 and 69 years of age which is comparable to earlier studies.[8] Further, most of them were female, illiterate, and widows/widowers. Similar findings were obtained through some of the previous studies.[69] The lower educational status of study participants has been also reported by Purty et al.[10] Most of the female inmates of OAHs said that they were homemakers and spent their whole time doing household work. The residents living in OAHs often confront problems due to highly institutionalized, depersonalized, and bureaucratic atmosphere in OAHs. Elderly living in such homes face problems of adjustment with tight and rigid schedules, separation from the family, isolation from the social milieu, anxiety over adopting oneself to a new environment and close encounters with death and ailment in the institutions. These factors make the older adults living in OAHs vulnerable to psychological problems.[8] Followed by the psychiatric morbidity were elucidated in following order.
Psychiatric illness
The findings were shown in the present study overall prevalence of PI is 43%, with prevalence in females at 51% and in males at 21%. This finding is supported by the study done by Tiwari et al.[6] Depression (37.7%) was found to be the most common mental health problem whereas anxiety disorders (13.3%) and dementias (11.1%) were the least[61112] and their studies highlight the need for proper assessment and confirmation of depression and anxiety, especially among the institutional elderly persons.
In the present study, depression was the most prevalent disorder (53.7%), followed by dementia (21.6%), and the least prevalent disorder being BPAD (0.7%). These findings were supported by a study by Kumar et al.[9] In their study in India, more than half of the inhabitants of OAHs were found to be suffering from one or other mental health problems, depression being the most common one. Similar findings by Barua et al.[13] show that the median prevalence rate of depression among the elderly Indian population was determined to be 21.9%, interquartile range = (11.6%–31.1%). Most common mental disorder which characterized by declining mood, loss of motivation, lack of physical energy, inability to feel pleasure, disturbed sleep, feelings of hopelessness, helplessness and worthlessness, and poor concentration in depression.[14] Praveen Kumar et al.[12] study showed high prevalence of depression and anxiety. Variations in the prevalence of depression and anxiety across many studies can be attributed to type of screening tools used. The prevalence of anxiety in this study was 94.6% among institutional elderly persons when compared with 92.6% among those living in the community. A comparative study was done on the psychiatric morbidity in the geriatric population. Singh et al.[11] study reveals that the prevalence of anxiety was 5% among elderly population living in OAHs and 6.7% in elderly population in the community. A study done in Pune[15] reported that the prevalence of anxiety disorders was 6.4% among the elderly persons aged 65 years and older. Although the levels of anxiety among the elderly people varied from one study to the other, there was no significant difference between the institutional and noninstitutional elderly persons.
CONCLUSIONS
In the present study, findings revealed that 56% of the inmates of OAH had no PI while inmates suffering from PI were 43%. Depression is the most common disorder in older adults was five districts in Northern India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are thankful to the administrative personnel of the OAHs for their cooperation in the study. Authors also greatly appreciate the OAHs residents for participating in the study.
REFERENCES
- Health status of elderly living in the old age homes: An overview. JMSD 2013:131-41.
- [Google Scholar]
- The oldest old and the use of institutional long term care from an international perspective. In: Suzman R, Willis DP, Manton KG, eds. The Oldest Old. New York: Oxford University Press; 1992. p. :250-9.
- [Google Scholar]
- Development and standardization of scale to assess the satisfaction and expectation of older adults in old age homes. 2014. Indian J Sci Res. 4:645-50. Available from: http://www.ijsr.net
- [Google Scholar]
- Mental health status of elderly persons in rural area of India. Indian J Basic Appl Med Res. 2012;1:309-12.
- [Google Scholar]
- Mental health problems among inhabitants of old age homes: A preliminary study. Indian J Psychiatry. 2012;54:144-8.
- [Google Scholar]
- Prevalence of psychiatric disorders among the rural geriatric population: A pilot study in Karnataka, India. Cent Asian J Glob Health. 2015;4:138.
- [Google Scholar]
- A study of psychiatric and physical morbidity among residents of old age home. Int J Health Sci Res. 2012;2:57-74.
- [Google Scholar]
- Mental and physical morbidity in old age homes of Lucknow, India. Delhi Psychiatry J. 2012;15:111-7.
- [Google Scholar]
- Morbidity pattern among the elderly population in the rural area of Tamil Nadu. Turk J Med Sci. 2006;36:45-50.
- [Google Scholar]
- Psychiatric morbidity in geriatric population in old age homes and community: A comparative study. Indian J Psychol Med. 2012;34:39-43.
- [Google Scholar]
- Depression and anxiety among the elderly persons from institutional and noninstitutional settings in the field practice area of a tertiary-care institute, Andhra Pradesh: A comparative study. Int J Med Sci Public Health. 2016;5:2337-40.
- [Google Scholar]
- Depression in old age: Prevalence and predictors. Int J Health Sci Res. 2016;6:206-12.
- [Google Scholar]
- Prevalence of psychiatric and physical morbidity in an urban geriatric population. Indian J Psychiatry. 2011;53:121-7.
- [Google Scholar]






