Translate this page into:
Prevalence of Autism Spectrum Disorder among Rural, Urban, and Tribal Children (1–10 Years of Age)
Address for correspondence: Dr. Sunil Kumar Raina, Department of Community Medicine, Dr. R. P. Government Medical College, Tanda, Kangra, Himachal Pradesh, India. E-mail: ojasrainasunil@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Studies on autism spectrum disorders (ASDs) have largely focused on children in specific settings. The current scenario of research in ASDs is limited largely to clinic-based case reports, case series, and retrospective chart reviews. The present study is the first population-based prevalence study conducted across rural, urban, and tribal populations in India.
Materials and Methods:
A cross-sectional two-phase study was conducted covering children in the age group of 1–10 years of age across geographical regions representing rural, urban, and tribal populations. The first phase (screening phase) involved administration of the Hindi version of the Indian Scale for Assessment of Autism. Those identified as suspected of ASD and 10% of all classified as nonsuspects for autism were also evaluated by the clinical team in second phase (evaluation phase).
Results:
Forty-three children out of a total of 28,070 children in rural, urban, and tribal area in the age group of 1–10 years were diagnosed as cases of ASD yielding a prevalence of 0.15% (95% confidence interval [CI] =0.15–0.25). Logistic regression analysis showed a two times significantly higher risk of diagnosing ASD in rural area as compared to tribal (odds ratio [OR]; 95% CI = 2.17 [1.04–4.52], P = 0.04). Male sex and upper socioeconomic group of head of family/father had a higher risk of getting diagnosed as autism as compared to lower socioeconomic group (OR; 95% CI - 3.23; 0.24–44.28, P = 0.38).
Conclusions:
Estimation of true prevalence of ASD in India is going to improve policies on developmental disabilities.
Keywords
Autism spectrum disorder
children
prevalence
rural
tribal
urban
INTRODUCTION
Autism spectrum disorders (ASDs) are a spectrum of disorders characterized by pervasive impairments in social reciprocity and/or communication, stereotyped behavior, and restricted interests.[1] ASD has been the focus of debate in recent years, largely as a result of multinational reports of increase in its prevalence.[1] Studies reporting on the prevalence of ASD have reported the prevalence estimates ranging from 0.07% to 1.8%.[234567] The studies also point to an apparent increase in the prevalence of ASD. This reported increase in prevalence appears partly attributable to greater public awareness, broadening ASD diagnostic criteria, lower age at diagnosis, and diagnostic substitution.[8]
Studies on ASD have largely focused on specific children populations; populations of children that are more likely to include children with ASD or children with histories of special needs or developmental delays.[139] In other words, the current scenario of research in ASDs is limited largely to clinic-based case reports, case series, and retrospective chart reviews. A few attempts have also been made to study neurobiological, genetic substrates, and effectiveness of available treatment approaches in ASD.
An extensive PubMed search on the prevalence or incidence of ASD in India reveals a paucity of epidemiological data. Data further reveal that there are no specific community-linked studies.[10] In this direction, this is the first population-based prevalence study conducted across rural, urban, and tribal populations in India.
Earlier, we published a midterm report of the present study.[11]
MATERIALS AND METHODS
Ethics
The study has been approved by the Institutional Ethics Committee. A written informed consent was obtained from parents of the children. Further, assent was obtained from children over the age of 7 years.
Study site
The state of Himachal Pradesh is predominantly mountainous with altitude ranging from 350 m to 7000 m above the sea. Himachal Pradesh is located in northwest of India, between the latitudes 30°22.40–33°12.20 N and the longitudes 75°45.55–79°04.20 E.[12] It is spread over 12 districts covering a total population of 6,856,509.[12]
Details of selected areas
For the purpose of the study, eligible population (children 1–10 years of age) from distinct geographical areas of this state, namely, a tribal area, a rural area, and an urban area was identified for inclusion. For selecting these geographical areas, the entire geography of the state was mapped according to the notified description for each area. On the basis of this, notification areas were identified as tribal areas, rural areas, and urban areas. From each grouping of the area's cluster, census blocks (for study population) were selected by a simple random sampling technique.
The study population thus covered included entire eligible population of the selected areas (tribal, rural, and urban) falling within three districts of Himachal Pradesh and covering a total population of 191,558.
Urban area
Kangra is situated in the Western Himalayas and falls in the humid zone. It is situated in the Western Himalayas between 31°2”–32°5” (N) latitude and 75°–77°45” (E) longitude. The urban areas to be studied were selected from this district.
Towns of Dharamsala and Palampur, which are generally having a hilly topography, and towns of Kangra and Nurpur, with a relatively plain terrain, were included in the study.[12]
Rural area
Una lies in the southwest of the state. The topography of this place is generally plain with low hills and lies in the subhumid tropical climatic zone. It is situated at an altitude ranging between 350 and 1200 m above mean sea level and is bounded between 75°58’2”–76°28’25” (E) longitude and 31°17’52”–31°52’0” (N) latitude. Haroli block of this district was selected for the study.[12]
Tribal area
Bharmour and Pangi were selected for the study of prevalence of autism in the tribal area of Himachal Pradesh. Bharmour is situated in the southeast of the district Chamba (Himachal Pradesh). It falls between 76°20’0” and 76°52’30” N latitude and 32°11’0” and 32°36’00” E longitude with a total geographical area of 1797.28 km2. This region is mostly inhabited by a distinct tribe of nomadic pastoralists known as “Gaddis.” They travel from one ecological zone to another in winter and summer seasons. Pangi was also selected for the study of prevalence of autism in this state. Pangi of Chamba district was also selected for the study. It lies in the northwestern extremity of the state. The villages of this area lie at an altitude ranging between 2100 m and 3000 m. It is situated in the semiarid zone of the inner Himalayas, which makes its terrain rough and difficult.
Study design and selection criteria
A cross-sectional study design was used for estimating the prevalence of ASD. The study covered the entire eligible population (children aged 1–10 years of age) of the selected areas available for participation on the day of survey. However, children with a history of hearing impairment were excluded from the study. No secondary visit was conducted and only de facto population was studied. All the houses from the selected areas were surveyed by a house-to-house survey to screen children with autism. The research was carried out in two phases: A screening phase and an evaluation phase.
Screening phase
Instrument
The study participants were screened by investigators trained in the diagnosis of ASD using the Hindi version of the Indian Scale for Assessment of Autism (ISAA).[13] The ISAA is based on childhood autism rating scale. It has forty items divided under six domains - social relationship and reciprocity; emotional responsiveness; speech, language, and communication; behavior patterns; sensory aspects; and cognitive component. The items are rated from 1 to 5 with an increased score indicating increased severity of the problem. A score <70 was taken as no autism, 70–106 as mild autism, 107–153 as moderate autism, and a score >153 severe autism. The Hindi version Indian Scale for Assessment of Autism (hereafter referred as HISSA) was modified to suit local needs using a systematic, iterative process. The details have been provided somewhere else.[11]
The screening phase also included an assessment of the sociodemographic profile of the participants (using a socioeconomic status [SES] pro forma) and administration of a behavioral checklist in addition to administration of HISAA.[1314] Separate SES pro forma (modified Kuppuswamy for the urban area and modified Prasad scale for the rural and tribal areas) was used for the urban, rural, and tribal areas.[1314]
Evaluation phase
After the screening phase, all the subjects who were scoring above seventy on the ISAA were considered suspected cases of autism and were evaluated by a clinical team comprising public health specialists, pediatrician, neurologist, and clinical psychologist. The evaluation included an account of the prenatal conditions, birth history, developmental and medical histories, findings from earlier evaluations (including a history of hearing impairment), and intellectual and behavioral functioning. The clinical evaluation also included observing the child for a few minutes.
The screening scores on the scale were also reconsidered and altered (wherever required) as per the recommendations of the clinical team. A child was defined as a confirmed case of ASD after confirmation by the clinical team.
Further, 10% of all the children who scored less and were thus classified as nonsuspects for autism were also evaluated by the clinical team.
RESULTS
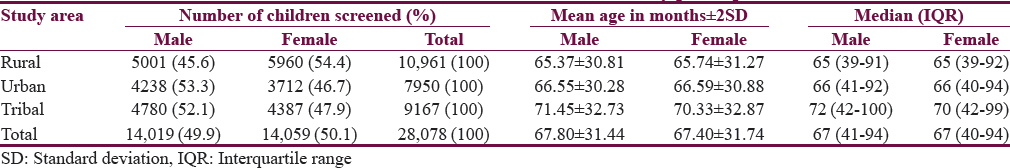
A total of 28,078 (children in the age group of 1–10 years) participants were screened using the standardized tools. The population sample included 14,059 (50.1%) females and 14,019 (49.9%) males. The number of females exceeded the number of males in the rural population, i.e., Una, whereas it was opposite for the tribal and urban areas. The mean age of the children screened in tribal area (male: 71.45 ± 32.73, female: 70.33 ± 32.87) was higher than that of rural and urban children [Table 1].
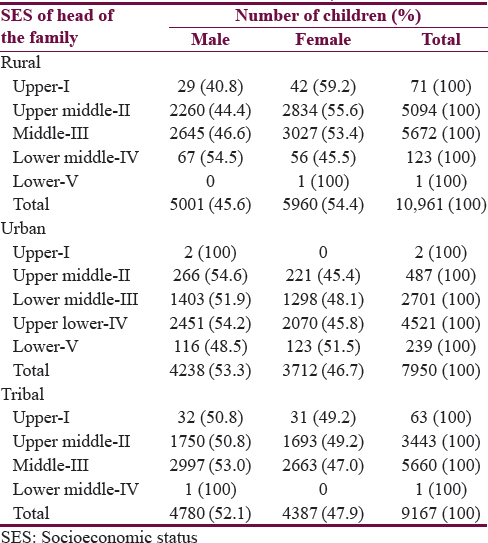
The SES of the head of the family/father (as per Uday Pareek scale) of the screened rural children in Table 2 shows that around half of the participants belonged to middle class (51.7%) followed by upper middle class (46.5%). The majority of children in tribal area (61.7%) belonged to middle class followed by upper middle class (37.6%). In urban area, 56.9% of participants screened belonged to upper lower class (according to modified Kuppuswamy scale) and 33.9% to lower middle class [Table 2].
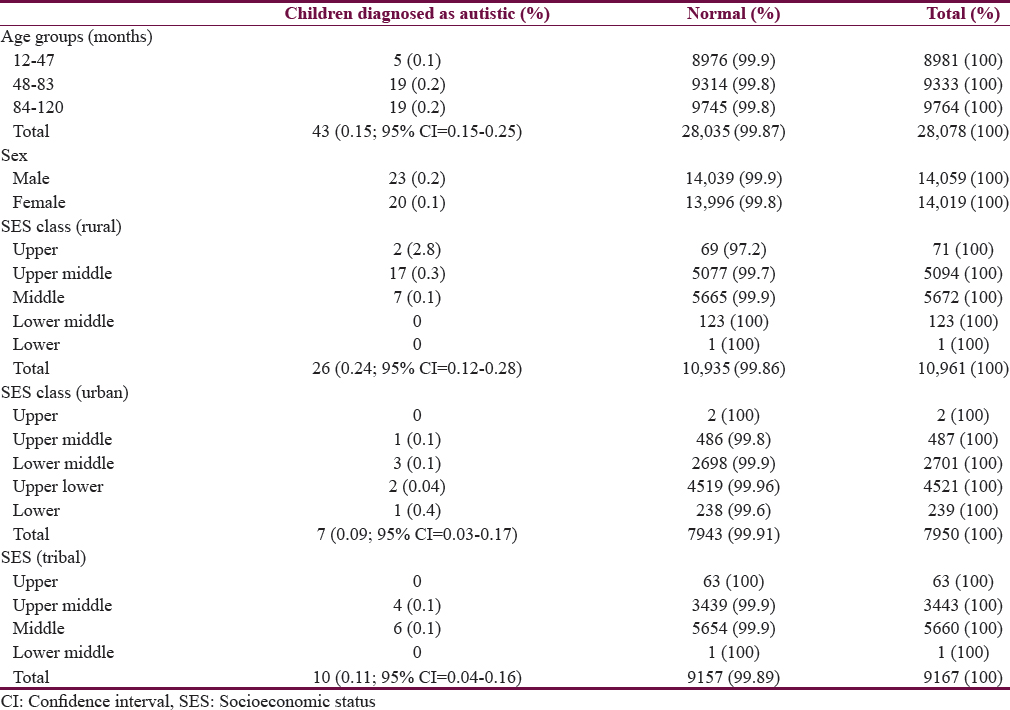
After the evaluation by the experts in the selected areas, 43 children out of a total of 28,070 children from rural, urban, and tribal areas in the age group of 1–10 years were diagnosed as cases of ASD yielding a prevalence of 0.15% (95% confidence interval [CI] = 0.15–0.25).
Majority of these 43 diagnosed (88.4%; 38/43) were above 4 years of age. Proportion of children with diagnosed autism was same across 48–83 months and 84–120 months age group (0.2%). A higher proportion of male children (0.2%) were identified as cases of ASD as compared to females (0.1%).
The prevalence of ASD was found to be highest in the rural area with 26 children in the age group of 1–10 identified as cases of ASD out of a total of 10,961 children studied yielding a prevalence of 0.24% (95% CI = 0.12–0.28). The prevalence was almost similar in urban and rural areas at 0.09% (95% CI = 0.03–0.17) and 0.11% (95% CI = 0.04–0.16), respectively.
A higher proportion of ASD was observed among upper class SES (2.8%) of rural area. Around two-thirds of the children with ASD (17/23) were from upper middle class in rural area. Applying the same scale for SES in tribal area shows that majority of the autistic children belonged to upper middle class families (56.3%). However, majority of these urban children with ASD were from lower middle class family (30%; 3/10) [Table 3].
Logistic regression analysis model was run with children diagnosed with autism as dependent variable and area of residence, age groups, sex, and SES as independent variables [Table 4]. A two times significantly higher risk of diagnosing ASD was observed in rural area as compared to tribal (odds ratio [OR]; 95% CI = 2.17 [1.04–4.52], P = 0.04). Higher age group (48–83 and 84–120 months) had 3–4 times higher chance of getting diagnosed as autism as compared to young age children (12–47 months) and this association was statistically significant (P = 0.01). Male sex had a 26% higher chance of getting diagnosed with autism as compared to female sex; however, this association was not significant (OR - 1.26; 95% CI - 0.69–2.30, P = 0.46).
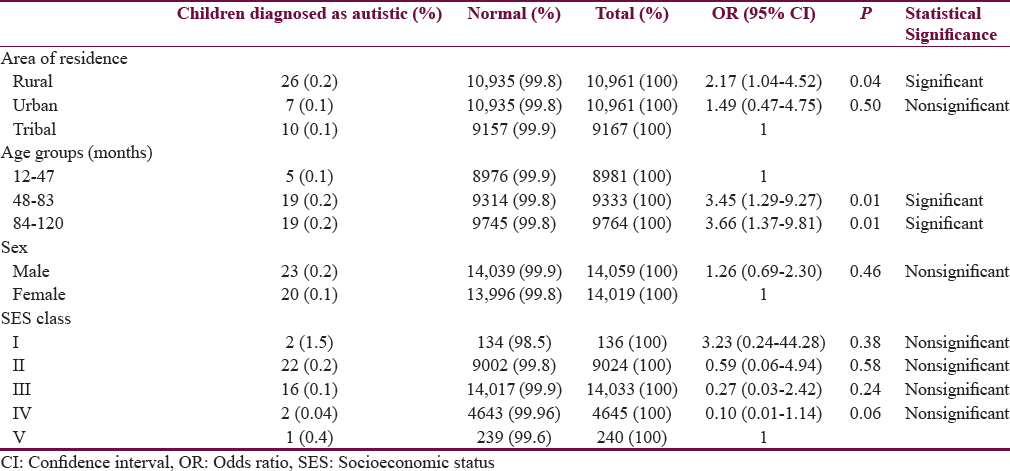
Children in upper Class (I) SES of head of family/father had a nonsignificant three times higher risk of getting diagnosed as autism as compared to lower Class (V) (OR; 95% CI - 3.23; 0.24–44.28, P = 0.38).
DISCUSSION
ASD is a complex neurodevelopmental disorder characterized by qualitative impairments in three domains: Social interaction, communication, and repetitive stereotyped behavior. As a rule, these impairments begin in early childhood (before the age of 3 years), persist throughout the full life span, and often cast a detrimental impact on the well-being of affected individuals.[15] Epidemiological surveys in different geographical regions since 2000 converge to estimates to a median of 17/10,000 for autistic disorder and 62/10,000 for all pervasive developmental disorders combined.[16] The current study was the first community-based study carried out in India on the prevalence of autism among 1–10 years age and reported a prevalence of 15/10,000 (0.15%). Studies in Asia, Europe, and North America have identified individuals with ASD with an average prevalence of between 1% and 2%.[17] The prevalence was significantly higher among children residing in rural areas as compared to urban and tribal. This was in contrast to an Arab study, where most of affected children were from urban areas, especially in Egypt and Jordan.[18] The prevalence is also affected by accessibility to a tertiary care center and source of case identification (mainly families).[19] Increased awareness about ASD with better access to health-care services among urban population leads to early diagnosis and management of the disorder. This could have led to improvement in symptoms and one of the reasons that a relatively lower proportion of study population fell in the category of autism.
Males presented with ASD in a higher proportion as compared to female children consistent with studies from elsewhere showing male predilection,[16] and there is no evidence to date that explains this finding.[20] One possible reason is that female children are more able to mask their behavioral difficulties than males. Furthermore, in developing countries, families may pay more attention to the development of male children compared with females or there could be lack of willingness by parents to report certain behavior exhibited by a female child.[21] However, gender in our study was insignificantly associated with ASD. This result contradicts previous findings in a cohort study that included 118 children with autism followed into adolescence which reported more significant social impairment among females.[22]
The prevalence of ASD was observed to be significantly higher among children 4–10 years with mild autism also higher in same age. The prevalence was higher in early years (1–7 years) for moderate autism. One possible reason could be that the case identification by the family was delayed till motor and speech development. Even though ASD can be diagnosed as early as age 2 years, most children are not diagnosed with ASD until after age 4 years.[17]
The 2011–2012 National Survey of Children's Health, US, included children aged 6–17 years; when further stratified by age, the ASD prevalence was 18.2/1000 children aged 6–9 years, which was much higher as compared to our study (7–10 years, 2/1000).[23] The difference could be due to difference in geography, culture, SES, and methodology used.
SES is one of the fundamental indicators of ASD and is corroborated by our findings.[24] A higher prevalence was observed among “upper class” in rural area and “middle class” in both urban and tribal areas.
A descriptive study conducted at an urban tertiary care center in India reported majority of autistic children from middle class SES. The probable reason for this finding was that upper class patients usually do not avail government hospital medical facilities.[25] In contrast, findings from Saudi Arabia reported most of the children diagnosed with autism belonged to families of low socioeconomic standards with unsatisfactory income.[18] Evidence suggests an inverse correlation between SES and mental health; however, this causation is based on longitudinal studies.[26]
These contrasting observations could be due to a low awareness among the source of identification in lower SES leading to negligence in early identification of the developmental delays further leading to higher mortality in children of lower SES due to associated anomalies with ASD. Furthermore, parents from lower SES groups may postpone seeking medical attention for disorders other than sickness.
The situation in low- and middle-income countries such as India appears to be that child health programs focus mainly on child survival issues. Very little attention is paid to developmental disabilities at policy and implementation level and as a result, budget allocations and human resource deployment are directed away from these programs. Lack of effective identification, referral program, and service delivery for these children is a big barrier.[16]
CONCLUSION
The true estimation of prevalence of ASD in India will go a long way in improving policies regarding developmental disabilities.
Financial support and sponsorship
The study was carried out with a research grant funded by Indian Council of Medical Research, New Delhi (Grant No.: 2010-13320/21:09:2012).
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the support of Dr. Sukhjit Singh, Associate Professor and Head, Department of Psychiatry, Dr. R. P. Government Medical College Tanda, Kangra (Himachal Pradesh) and Dr. Sanjeev Chaudhary, Professor and Head, Department of Paediatrics, Dr. R. P. Government Medical College Tanda, Kangra (Himachal Pradesh) for their help.
REFERENCES
- Infantile autism and other childhood psychoses in a Swedish urban region. Epidemiological aspects. J Child Psychol Psychiatry. 1984;25:35-43.
- [Google Scholar]
- Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: The Special Needs and Autism Project (SNAP) Lancet. 2006;368:210-5.
- [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance Year Principal Investigators; US Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders – Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR Surveill Summ. 2009;58:1-20.
- [Google Scholar]
- Reevaluating the incidence of pervasive developmental disorders: Impact of elevated rates of detection through implementation of an integrated system of screening in Toyota, Japan. Psychiatry Clin Neurosci. 2008;62:152-9.
- [Google Scholar]
- Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. 2006;91:8-15.
- [Google Scholar]
- Epidemiological surveys of autism and other pervasive developmental disorders: An update. J Autism Dev Disord. 2003;33:365-82.
- [Google Scholar]
- Prevalence of autism spectrum disorders among children (1-10 years of age) – Findings of a mid-term report from Northwest India. J Postgrad Med. 2015;61:243-6.
- [Google Scholar]
- Himachal Pradesh – Census 2011. Resource Document. Available from: http://www.census2011.co.in›states
- Kuppuswamy's socio-economic status scale – A revision of economic parameter for 2012. Int J Res Dev Health. 2013;1:2-4.
- [Google Scholar]
- Health-related quality of life in adolescents and young adults with high functioning autism-spectrum disorder. Psychosoc Med. 2010;7 pii: Doc
- [Google Scholar]
- Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5:160-79.
- [Google Scholar]
- CDC. Data and Statistics. Autism Spectrum Disorder. Resource Document. Available from: http://www.cdc.gov/ncbddd/autism/data.html
- Sociodemographic factors in Arab children with autism spectrum disorders. Pan Afr Med J. 2012;13:65.
- [Google Scholar]
- Systemic review of the epidemiology of autism in Arab Gulf countries. Neurosciences (Riyadh). 2014;19:291-6.
- [Google Scholar]
- Heritable and nonheritable risk factors for autism spectrum disorders. Epidemiol Rev. 2002;24:137-53.
- [Google Scholar]
- Autism in Saudi Arabia: Presentation, clinical correlates and comorbidity. Transcult Psychiatry. 2009;46:340-7.
- [Google Scholar]
- Autism spectrum and attention-deficit disorders in girls. Some neuropsychological aspects. Eur Child Adolesc Psychiatry. 2000;9:180-5.
- [Google Scholar]
- Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011-2012. Natl Health Stat Report. 2013;20:1-11.
- [Google Scholar]
- Socioeconomic status and the increased prevalence of autism in California. Am Sociol Rev. 2011;76:320-46.
- [Google Scholar]
- A descriptive hospital based study of children with autism. Indian Pediatr. 2005;42:453-8.
- [Google Scholar]
- Socioeconomic status and mental illness: Tests of social causation and selection hypothesis. Am J Orthopsychiatry. 2005;75:3-18.
- [Google Scholar]






