Translate this page into:
Prevalence and Awareness of Stroke and Other Comorbidities Associated with Diabetes in Northwest India
Raghuram Nagarathna, Medical Director Arogya Dham, SVYASA, Bengaluru 560105 India rnagaratna@gmail.com
Akshay Anand, PhD Department of Neurology, PGIMER Chandigarh, 160014 India akshay1anand@rediffmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Objectives The main purpose of this study is to investigate the prevalence of comorbid conditions in diabetic, prediabetic, and nondiabetic individuals. Additionally, the current study examines the levels of awareness of those comorbidities among North Indian population.
Methods As a part of a national study (Niyantrit Madhumeh Bharat [NMB] screening program), different comorbidity parameters were screened in the northern part of India between April and September 2017. There were 1,215 participants recruited in this study. Biochemical analyses of hemoglobin A1c (HbA1c) were conducted on the study subjects. Subsequently, the study subjects were divided into diabetic, prediabetic, and nondiabetic groups based on their HbA1c results.
Results The study analysis reveals a higher prevalence of peripheral vascular disease (21.2%), ocular diseases (18%), and hypertension (13.4%) in diabetics with other comorbidities. Furthermore, the study found that a vast majority of the participants were unaware of the presence of hypertension (67.2%), dyslipidemia (84.5%), kidney disease (95.2%), peripheral vascular disease (34.5%), and stroke (95.1%).
Conclusion The study concluded that in the northern India, the prevalence of multiple comorbid conditions, such as peripheral vascular disease and hypertension, is higher among diabetic population. Also, the level of awareness of diabetic comorbidities is surprisingly low, which has implications for policymakers, health practitioners, and educators of alternate medicine to increase awareness about diabetes, comorbid conditions, health risk, and possible solution at community and rural level, such as periodic screening programs in this population.
Keywords
diabetes mellitus
comorbidity
awareness
North India
policy change
Introduction
Diabetes mellitus (DM), as a global pandemic, is posing a major public health challenge worldwide. Current global estimates indicate that 415 million people are affected with this condition and projected to escalate to 642 million by the year 2040.1 2
The growing burden of diabetes-related healthcare outcomes, treatment options, care requirements, and costs is complicated by increasingly higher number of associated comorbidities. This includes cardiovascular diseases (CVD), nephropathy, neuropathy, retinopathy, cognitive disorders, and hypertension.3 Past studies found that most patients with DM have a coexisting medical condition and 40% of them have three or more comorbid conditions.4 Interestingly, a previous study described that “a patient with diabetes and no other medical problem is an exception rather than a rule.”5 For example, a higher prevalence (75%) of CVD was also found in DM as compared with non-DM.6 Additionally, a previous study found that 23% of patients with DM had a cluster of hypertension-hyperlipidemia-obesity.7 The high prevalence of diabetic comorbidities indicates the need for investigating the strengths and directions of their relationship across different populations, gender, and their healthcare consequences.
Globally, India has the second largest population with DM after China and faces a daunting task of mitigating public health risks and health cost associated with DM and its comorbid conditions.8 Various factors account for the country-wide prevalence of diabetes, but lack of adequate Indian studies on the increasing prevalence of DM and associated comorbidities demands quality studies to help mitigate associated health risks among the populations. The Indian Council of Medical Research had previously found that the states of North India have a lower proportion of diabetic population (Chandigarh 0.12 million, Jharkhand 0.96 million) as compared with Maharashtra and Tamil Nadu.9
In an overburdened healthcare system like India, diabetic comorbidity may not only affect access to and quality of care but also incur higher healthcare utilization costs creating a higher economic and healthcare burden.10 Studies have reported that health expenditure incurred by diabetic patient is mostly related to the comorbidities and resulting complications.11 12 13 14 Yesudian et al had previously reported a higher total cost (INR 14600; USD 300) incurred by patients with diabetic comorbidities than those without comorbid conditions (INR 4500; USD 90),9 which has important implications for healthcare policies. Therefore, prevalence of different diabetic comorbid conditions across different populations will help policymakers, local authorities, and healthcare providers to evaluate the health and monetary risks in specific patient subgroups, and plan healthcare resource allocation to streamline diabetic care management programs for population subsegments efficiently.
Various studies in India focused mostly on the prevalence of single diabetic comorbidity; however, a few studies have investigated the association of multiple diabetic comorbidities in Indian population. Therefore, the current study aims to investigate the comparative prevalence of multiple diabetic comorbidities in patients with DM and prediabetes. We also aim to investigate the level of awareness regarding those comorbidities among these participants.
Methods
Subject Recruitment and Screening
As a part of a national study (Niyantrit Madhumeh Bharat [NMB] screening program), information of six comorbidity parameters peripheral vascular disease, stroke, hypertension, dyslipidemia, kidney disease, and ocular diseases was obtained by door to door screening, and the subject population was categorized into nondiabetic, prediabetic, and diabetic on the basis of their hemoglobin A1c (HbA1c) values. This observational type of study was conducted at the northern part of India across various regions of Panchkula (Haryana [state]) and Chandigarh (union territory). A total number of 1,215 of registered participants filled the questionnaire prepared under the NMB screening program, mainly coordinated by SVYAS, Bangalore.
Questionnaire
A self-reported questionnaire was structured (as exemplified below) for the current study, which screened for six different comorbid conditions with categorical responses as yes/no/no knowledge.
Have you ever been told by a health provider that you have high blood pressure?
Biochemical Analysis
The study participants were instructed to come for a blood sample in the early morning with overnight fasting. The collected sample was sent for HbA1c analysis to a National Accreditation Board for Testing and Calibration Laboratories (NABL)-accredited laboratory.
Data Analysis
All the registered participants were given a unique identification code and the data was recorded in the Microsoft Excel sheet version 10. The data analysis was done using SPSS statistical software version 21.0.
Ethical Committee Clearance
Institutional ethical committee clearance was taken with reference no: RES/IEC-IYA/001 dated 16 December 2016. Each participant was explained about the study, and informed written consent was taken before filling the registration form.
Results
Of the 1,215 registrations forms, 560 forms were validated and any missing forms were removed. Of the 560 participants, 478 were included in the analysis based on their HbA1c levels. Participants with any missing data were excluded from the study (Fig. 1).
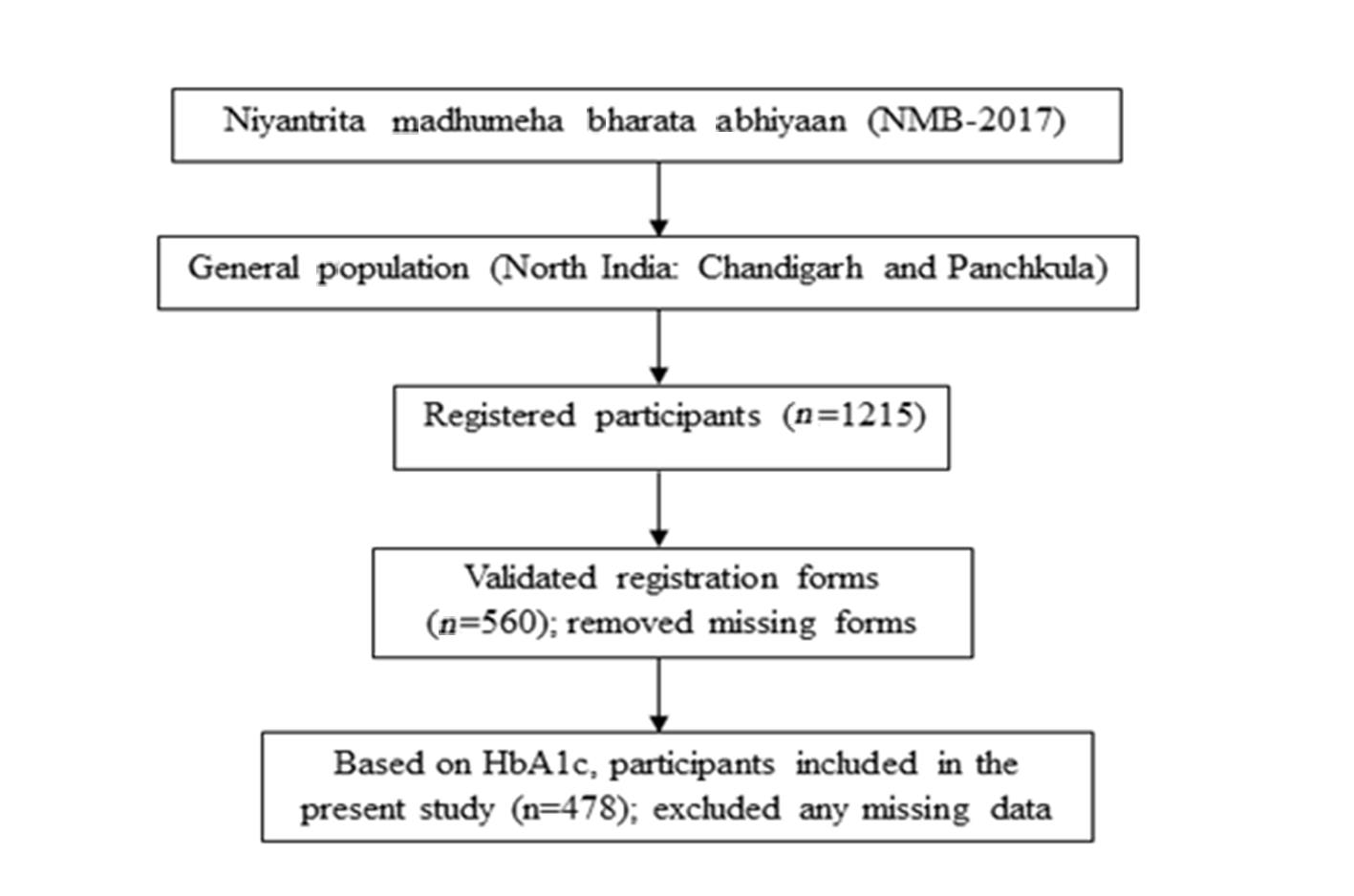
-
Fig. 1 Study profile of the recruited participants.
Fig. 1 Study profile of the recruited participants.
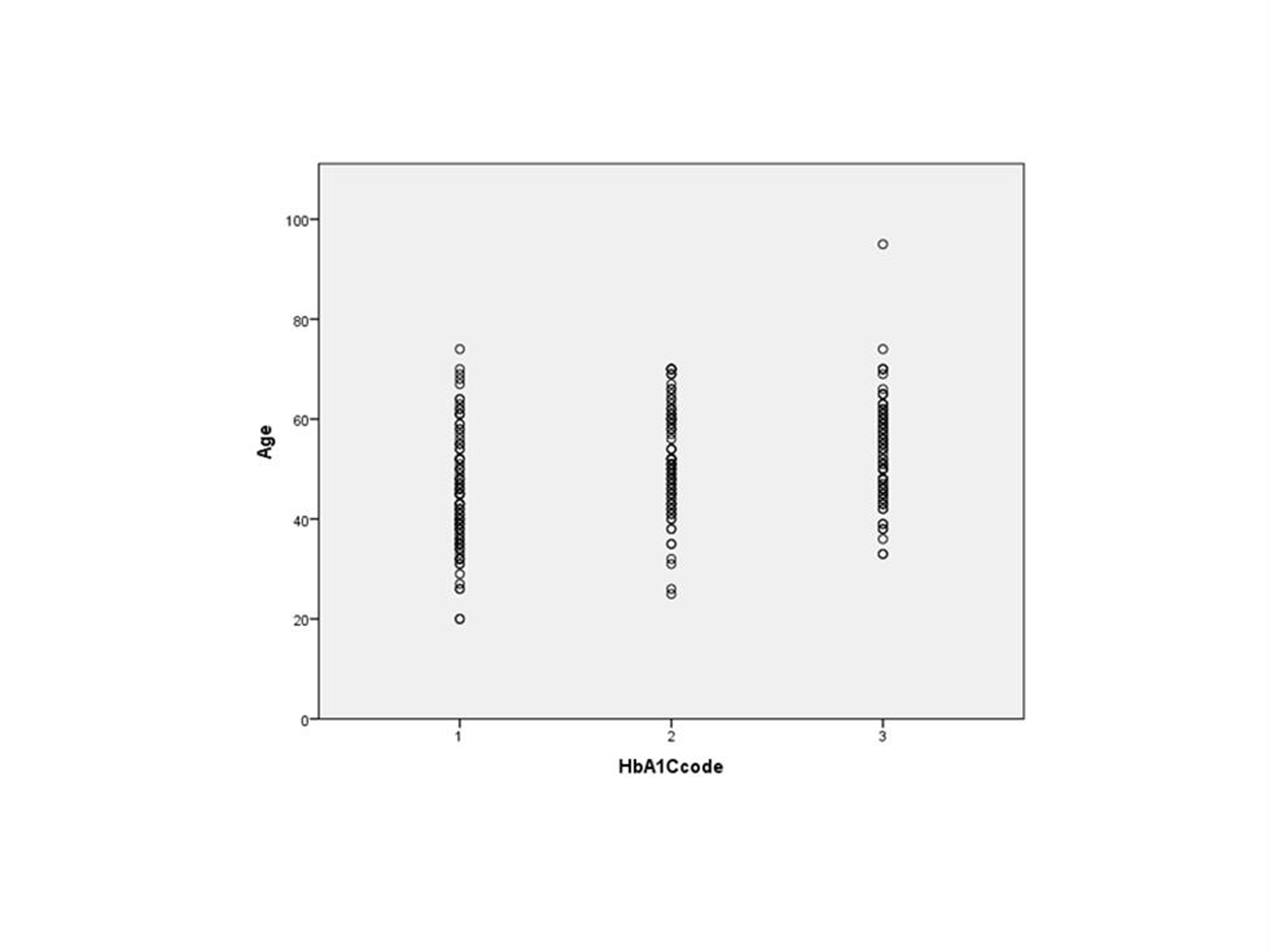
There were 173 participants, who were found nondiabetic (HbA1c < 5.7%), 148 participants were prediabetic (HbA1c between 5.7 and 6.4%), and 157 participants were diabetic (HbA1c > 6.4%). Female population accounted for 73.6% of the participants. The mean age of the participants was 50.14 ± 11.159. Table 1 shows the demographic findings of the participants and Fig. 2 showed HbA1c levels of the subjects across different age of individuals.
|
Abbreviation: HbA1c, hemoglobin A1c. |
||
|
Gender (n) |
Female |
352 (73.6%) |
|
Male |
126 (26.4%) |
|
|
Total |
478 |
|
|
Age (y) |
50.14 ± 11.159 |
|
|
HbA1c category |
Nondiabetics (<5.7) (n) |
173 |
|
Prediabetics (5.7–6.4) (n) |
148 |
|
|
Diabetics (≥6.5) (n) |
157 |
|
|
Total |
478 |
|
-
Fig. 2 Representation of hemoglobin A1c (HbA1c) across different age individuals (1: nondiabetics; 2: prediabetics; 3: diabetics).
Fig. 2 Representation of hemoglobin A1c (HbA1c) across different age individuals (1: nondiabetics; 2: prediabetics; 3: diabetics).
Out of 478 individuals, the missing data of each comorbidity were excluded. Remaining data were analyzed to understand the prevalence of six different comorbidities among nondiabetic, diabetic, and prediabetic population groups. Furthermore, data was analyzed for the percentages of population who are not aware of their comorbidities.
Prevalence of Comorbidities in Nondiabetic, Diabetic, and PreDiabetic Groups
The statistical analysis depicted in Table 2 found a higher prevalence of peripheral vascular disease (21.2%), ocular diseases (18%), and hypertension (13.4%) in diabetics compared with other comorbidities.
|
Comorbidities |
Nondiabetic (HbA1c <5.7) |
Prediabetic (HbA1c 5.7–6.4) |
Diabetic (HbA1c ≥6.5) |
|||
|---|---|---|---|---|---|---|
|
Present/aware n (% total) |
Absent/not aware n (% total) |
Present/aware n (% total) |
Absent/not aware n (% total) |
Present/aware n (% total) |
Absent/not aware n (% total) |
|
|
Abbreviation: HbA1c, hemoglobin A1c. |
||||||
|
Hypertension (n = 299) |
29 (9.7%) |
75 (25.1%) |
29 (9.7%) |
64 (21.4%) |
40 (13.4%) |
62 (20.7%) |
|
Dyslipidemia (n = 298) |
13 (4.4%) |
91 (30.5%) |
13 (4.4%) |
79 (26.5%) |
17 (5.7%) |
85 (28.5%) |
|
Kidney disease (n = 299) |
5 (1.7%) |
99 (33.1%) |
5 (1.7%) |
88 (29.4%) |
7 (2.3%) |
95 (31.8%) |
|
Peripheral vascular disease (n = 245) |
60 (24.5%) |
33 (13.5%) |
46 (18.8%) |
27 (11.0%) |
52 (21.2%) |
27 (11.0%) |
|
Stroke (n = 245) |
4 (1.6%) |
89 (36.3%) |
5 (2.0%) |
68 (27.8%) |
3 (1.2%) |
76 (31.0%) |
|
Ocular diseases (n = 245) |
33 (13.5%) |
60 (24.5%) |
35 (14.3%) |
38 (15.5%) |
44 (18.0%) |
35 (14.3%) |
The prediabetics exhibited higher prevalence of peripheral vascular disease (18.8%) followed by ocular diseases (14.3%) and hypertension (9.7%), which were lower than the diabetic population. The prevalence of other comorbid conditions was similar in both diabetic and prediabetic groups for dyslipidemia (4.4 vs. 5.7%), kidney diseases (1.7 vs. 2.3%), and stroke (2 vs. 1.2%). However, the prevalence of overall comorbidities was higher in the diabetic group as compared with the prediabetic group. The prevalence of all the six comorbidities except peripheral vascular diseases (24.5 vs. 18.8%) was similar among nondiabetic and prediabetic population.
Prevalence of Comorbidity Unawareness among Nondiabetic, PreDiabetic, and Diabetic Population
The statistical analysis depicted in Table 2 shows that among nondiabetics, prediabetics, and diabetics, a total of 67.2% of individuals reported being unaware of having hypertension (20.7% in diabetics), 84.5% individuals of dyslipidemia (28.5% in diabetics), 95.2% of kidney disease (31.8% in diabetics), 34.5% of peripheral vascular disease (11% in diabetics), 54.3% of ocular diseases (14.3% in diabetics), and 95.1% of stroke (31% in diabetics).
Discussion
The data collected from the NMB screening program has identified six comorbid conditions related to nondiabetic, prediabetic, and diabetic individuals. In the current study, comparing diabetes with other comorbid conditions, a higher prevalence of peripheral vascular disease and hypertension was observed in both diabetics and prediabetics. The diabetic group of this population had an increased risk of hypertension, dyslipidemia, and ocular diseases compared with prediabetic group. Hypertension is a common comorbid condition with diabetic patients. A study reports that hypertension is three times more prevalent in diabetics as compared with the nondiabetics.15 Tripathy et al investigating the prevalence of diabetic comorbidities in a North Indian population found frequent coexistence of DM, hypertension, obesity, and dyslipidemia that is consistent with our findings.16
Knowledge of the prevalence about coexisting medical conditions in specific population groups helps healthcare providers and policymakers to allocate health resources efficiently and tailor diabetic care management to effectively utilize healthcare programs while decreasing healthcare expenditure.10 In light of increasing prevalence of diabetes and associated comorbid conditions, there is a need for proper guidelines to address health risks of diabetes with other comorbid conditions. Otherwise, the presence of coexisting medical conditions may deteriorate health and quality of life. Additionally, such conditions may impair diabetes self-care management and adherence to medical treatment leading to adverse health outcomes. Additionally, this can impose excessive health expenditure and impose a huge financial burden on patients, their families, and the government.10 Certain diabetic comorbidities concordantly share similar pathophysiologic risks or disease management plan. A study reports that ~75% of adults with diabetes have concomitant hypertension, which is possibly due to their common underlying risk factors.17 The chronicity of the disease and increased prevalence of comorbid conditions make its management complex for the patient and for the healthcare providers alike.18 The Veterans Affairs/Department of Defense guideline recommends assessing patients’ total health status during their diabetes management.19 However, diabetes care guidelines have mostly centered their recommendations on diabetic-specific management.
In the present study, the awareness about different comorbidities in the study population was surprisingly less. Nearly one-third of the participants with diabetes showed no awareness of coexisting dyslipidemia, kidney disease, and stroke. Despite the higher literacy rate, per capita income, and a standard of living in Chandigarh among all other Indian states, people were found unaware of their comorbid conditions. This is unexpected because studies have shown individuals with higher education level are more likely to undergo annual health check-ups, to follow medications, and perform physical activity.20 We have conceptualized a theoretical framework of knowledge, attitude, and practice as public health determinants of health outcomes, which can reflect the outcome of unawareness and lack of knowledge in this population (Fig. 3).
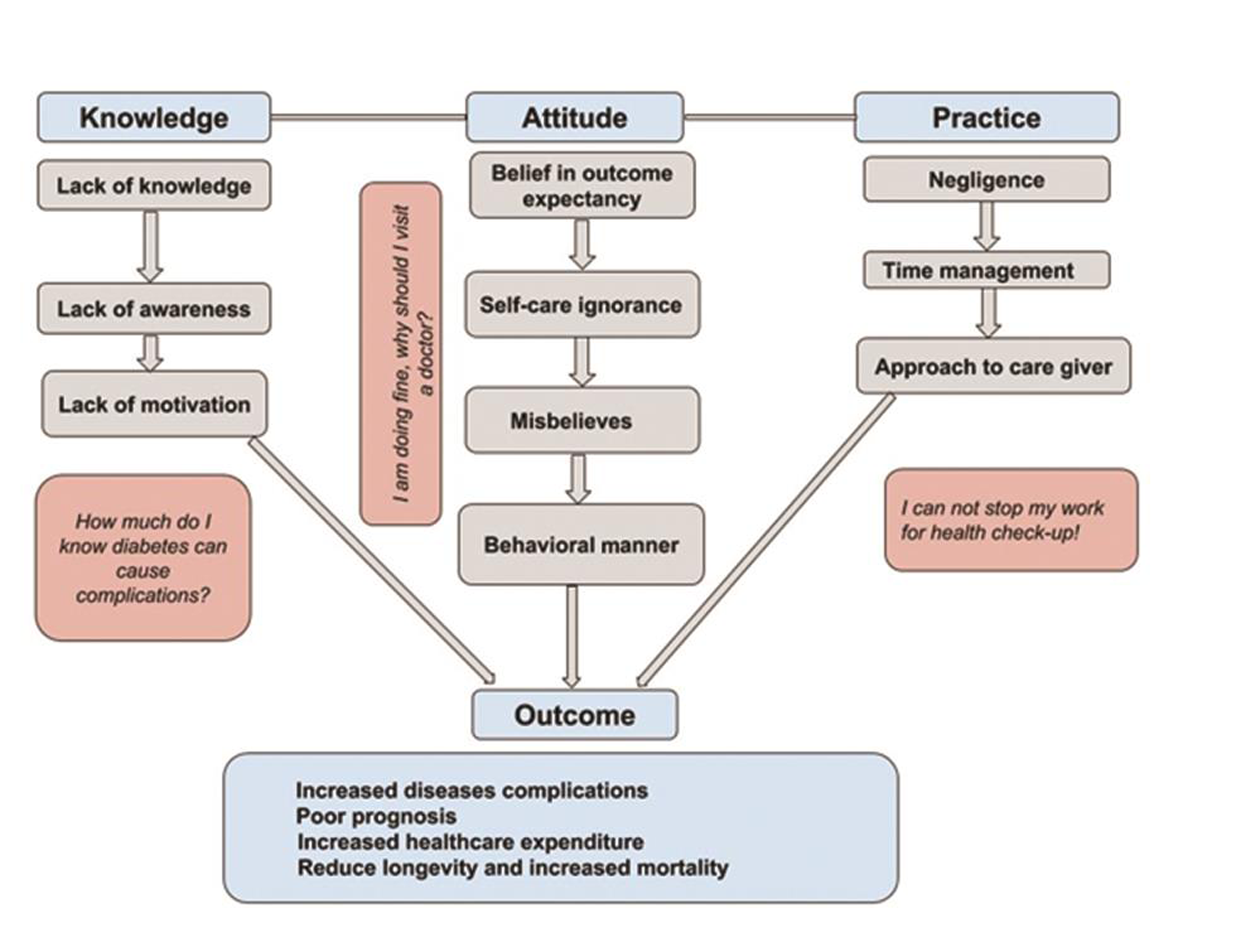
-
Fig. 3 A conceptual framework of knowledge, attitude, and practice as determinants of health outcomes.
Fig. 3 A conceptual framework of knowledge, attitude, and practice as determinants of health outcomes.
Mohan et al conducted a study in Indian population regarding knowledge and awareness among diabetics and found that less than 20% of the whole population and over 40% of known diabetic patients are not aware that diabetes can cause health complications. The study also reports that only 30% of individuals had knowledge of diabetes-related kidney, eye, and nerve diseases.21 Among diabetic subjects, the awareness of complications of diabetes was inadequate, which indicates that the majority of patients in this population have not been educated about diabetic comorbidities by healthcare providers providing an opportunity for increased public health initiatives. The lack of awareness because of poor diabetic education, short consultation time, and lack of diabetic educators indicates a need for installing diabetic education programs and increasing awareness for the diabetic population.22 23 Alternate programs to manage diabetes as shown in Fig. 3 can be useful with awareness creation. Mind-body practices such as Yoga have been shown to act on mind-body level and have been successful in the management of type 2 diabetes.24 Poor control of diabetes and its complications can result from oversecretion of cortisol and resulting insulin resistance, due to stress-mediated chronic activation of hypothalamic–pituitary–adrenal axis and sympathetic nervous system and reduced parasympathetic activity with increased levels of inflammatory cytokines. Yoga effectively enhances vagal activity and the associated antistress mechanisms that improve diabetic control as illustrated in Fig. 4.25
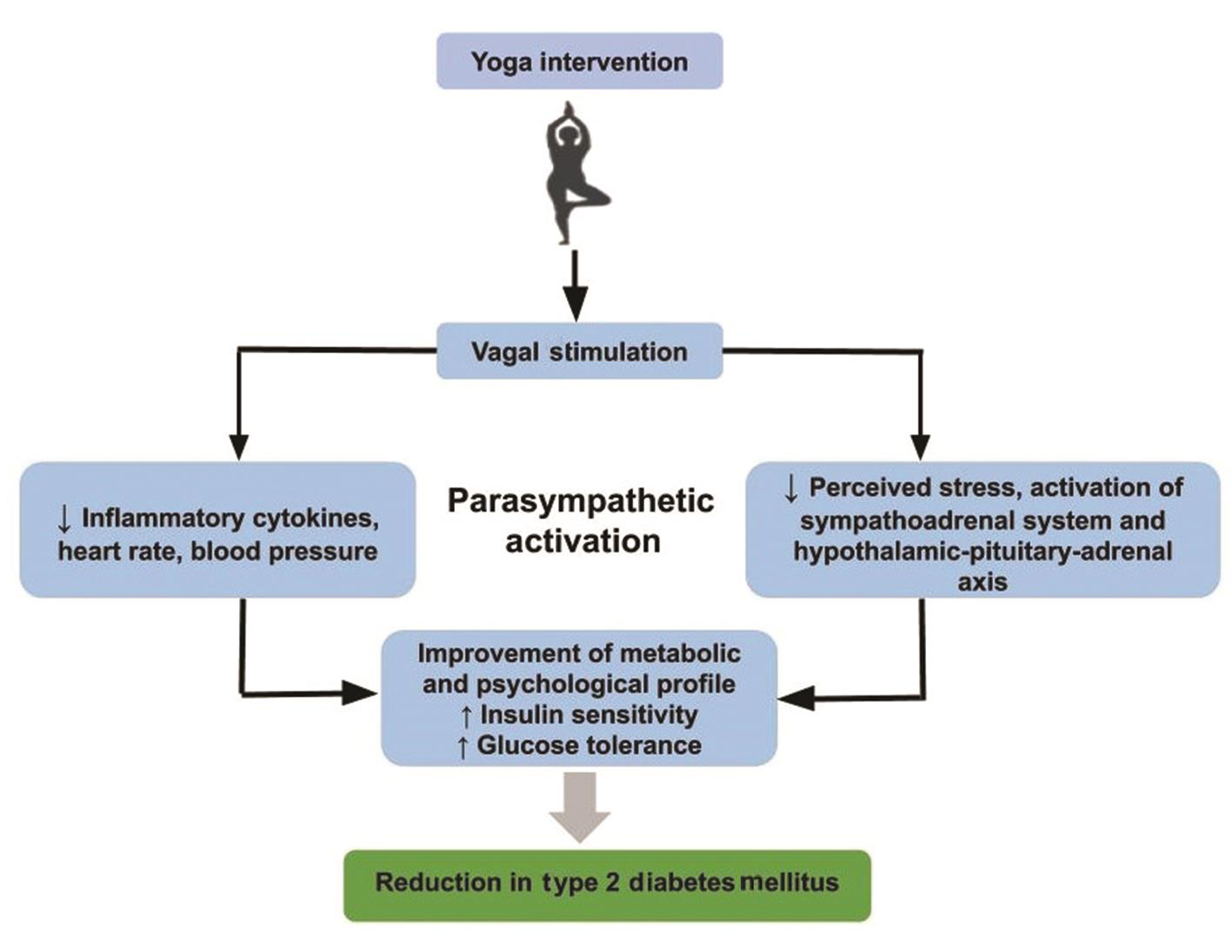
-
Fig. 4 Diagrammatical conceptual outlines of Yoga intervention and reduction in type 2 diabetes as health outcomes.
Fig. 4 Diagrammatical conceptual outlines of Yoga intervention and reduction in type 2 diabetes as health outcomes.
Diabetic education is one of the key strategies in diabetic management and studies have shown increased knowledge about diabetes and associated comorbidities that can benefit patients by improving patient compliance, and decreasing complications of diabetes.28 29 30 The results reflected in this study are significant indicators of prevalent problematic scenarios in the whole India.
Conclusion
The current study was performed in a large representative sample of the northern part of India across various regions of Panchkula (Haryana [state]) and Chandigarh (union territory) reporting six comorbid conditions among diabetic subjects with a higher prevalence of peripheral vascular disease, hypertension, and ocular diseases. Interestingly, the study also reflected poor knowledge and awareness of diabetes-related comorbidities. This emphasizes the necessity of increasing diabetes awareness at a large scale. This can be done either in the form of hospital- and community-based diabetic education programs or upcoming Ayushman Bharat wellness centers. Also, such findings indicate a necessity for community and rural screening programs and patients’ referral to tertiary care health centers, which could be the first step toward prevention, early detection, and control of health complications.
Acknowledgment
The authors acknowledge the support of CCRYN for man power, MOHFW for supporting the cost of investigations, and IYA for the overall project implementation. They also acknowledge Diksha Puri, Divya Dwiwedi, and Debopriya Basu for the validation of the data.
Authors’ Contributions
V. P.—writing and editing of the manuscript; V.S.—writing and editing of the manuscript; S.K.—data analysis; R.N.—conceptualization, Project PI and overall responsibility of manuscript for correspondence; M.S.S.—writing of the manuscript; K.S.—monitoring validation processes; N.K.—data collection and validation; A.K.S.—national coordination of project and writing; N.M.—supervised the work of NK; V.B.—medical person to oversee ethical issues; A.A.—concept of manuscript; H.R.N.—vision, project execution, troubleshooting.
Conflict of Interest
None declared.
Funding This research work was supported by Ministry of AYUSH, Government of India (grant number: 16-63/2016-17/CCRYN/RES/Y&D/MCT/ dated 15.12.2016).
References
- IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311-321.
- [Google Scholar]
- Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016;12(6):357-370.
- [Google Scholar]
- Prevalence and pattern of co-morbidity among type 2 diabetics attending urban primary healthcare centers at Bhubaneswar (India) PLoS One. 2017;12(8):e0181661.
- [Google Scholar]
- Prevalence of comorbid depression is high in out-patients with type 1 or type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diabet Med. 2010;27(2):217-224.
- [Google Scholar]
- The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diabetes Care. 2002;25(3):482-486.
- [Google Scholar]
- Multiple chronic conditions in type 2 diabetes mellitus: prevalence and consequences. Am J Manag Care. 2015;21(1):e23-e34.
- [Google Scholar]
- Comorbidity in patients with diabetes mellitus: impact on medical health care utilization. BMC Health Serv Res. 2006;6(1):84.
- [Google Scholar]
- The economic burden of diabetes in India: a review of the literature. Global Health. 2014;10(1):80.
- [Google Scholar]
- Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963-970.
- [Google Scholar]
- The cost of diabetes care—an elephant in the room. Diabetes Care. 2018;41(5):929-932.
- [Google Scholar]
- Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(3):293-301.
- [Google Scholar]
- Healthcare use and expenditure for diabetes in Bangladesh. BMJ Glob Health. 2017;2(1):e000033.
- [Google Scholar]
- Diabetes and hypertension physiopathology and therapeutics. J Hum Hypertens. 2000;14(01):S26-S31.
- [Google Scholar]
- Prevalence and determinants of comorbid diabetes and hypertension: evidence from noncommunicable disease risk factor STEPS survey, India. Diabetes Metab Syndr. 2017;11(01):S459-S465.
- [Google Scholar]
- Comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J Clin Hypertens (Greenwich). 2011;13(4):244-251.
- [Google Scholar]
- Comorbidity type and health care costs in type 2 diabetes: a retrospective claims database analysis. Diabetes Ther. 2018;9(5):1907-1918.
- [Google Scholar]
- Prioritization of care in adults with diabetes and comorbidity. Ann N Y Acad Sci. 2011;1243(1):69-87.
- [Google Scholar]
- Prevalence and risk factors of diabetes in a community-based study in North India: the Chandigarh Urban Diabetes Study (CUDS) Diabetes Metab. 2011;37(3):216-221.
- [Google Scholar]
- Awareness and knowledge of diabetes in Chennai-the Chennai urban rural epidemiology study [CURES-9] J Assoc Physicians India. 2005;53:283-287.
- [Google Scholar]
- Prevalence and risk factors of diabetes in a large community-based study in North India: results from a STEPS survey in Punjab, India. Diabetol Metab Syndr. 2017;9(1):8.
- [Google Scholar]
- Yoga for adults with type 2 diabetes: a systematic review of controlled trials. J Diabetes Res. 2016;2016:6979370.
- [Google Scholar]
- Partitioning of radiological, stress and biochemical changes in pre-diabetic women subjected to Diabetic Yoga Protocol. Diabetes Metab Syndr. 2019;13(4):2705-2713.
- [Google Scholar]
- Therapeutic role of Yoga in type 2 diabetes. Endocrinol Metab (Seoul). 2018;33(3):307-317.
- [Google Scholar]
- Psycho-neuro-endocrine-immune mechanisms of action of yoga in type II diabetes. Anc Sci Life. 2015;35(1):12-17.
- [Google Scholar]
- RSSDI clinical practice recommendations for the management of type 2 diabetes mellitus 2017. Int J Diabetes Dev Ctries. 2018;38:1-115. (1, Suppl 1)
- [Google Scholar]
- Knowledge and awareness of diabetes in urban and rural India: the Indian Council of Medical Research India diabetes study (phase I): Indian Council of Medical Research India diabetes 4. Indian J Endocrinol Metab. 2014;18(3):379-385.
- [Google Scholar]
- Effectiveness of the multidisciplinary risk assessment and management program for patients with diabetes mellitus (RAMP-DM) for diabetic microvascular complications: a population-based cohort study. Diabetes Metab. 2016;42(6):424-432.
- [Google Scholar]






