Translate this page into:
Predictors of In-hospital Mortality of Acute Ischemic Stroke in Adult Population
Address for correspondence: Dr. Bhupendra Shah, Department of Internal Medicine, B.P. Koirala Institute of Health Sciences, Dharan, Nepal. E-mail: doctorbhupen@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Stroke is the second most common cause of mortality worldwide. Data regarding the predictors of mortality of acute ischemic stroke are widely discordant. Identifying the predictors and providing the utmost care to a high-risk patient is still an unmet need in middle- to low-income countries. We did this study to identify the predictor of in-hospital mortality of acute ischemic stroke.
Materials and Methods:
We conducted a retrospective study of patients with acute ischemic stroke presented to the tertiary care center in eastern Nepal from January 2012 to December 2016. We enrolled patients of age 18 years and older with acute ischemic stroke in this study. The primary outcome of the study was in-hospital mortality of enrolled patients. Predictors of mortality were analyzed by comparing the patients with acute ischemic stroke who had mortality with those who survived.
Results:
The mean age of enrolled patients was 66 years. Among 257, the in-hospital mortality rate was 20.5%. The patients with in-hospital mortality had lower Glasgow coma scale (GCS) score (9 vs. 12, P < 0.001) compared to those who survived. During admission, a patient with in-hospital mortality had significantly lower arterial oxygen saturation (92 vs. 95, P < 0.001), higher pulse rate (91 vs. 83, P = 0.009), and higher respiratory rate (24 vs. 21, P < 0.001) than those patients with acute ischemic stroke who survived.
Conclusion:
Lower GCS score, baseline higher pulse rate, higher respiratory rate, and lower arterial oxygen saturation are the predictors of in-hospital mortality of adult with acute ischemic stroke.
Keywords
Ischemic stroke
mortality
predictors
INTRODUCTION
Stroke is the second most common cause of death and third leading cause of disability worldwide.[1] The in-hospital mortality rate of stroke of general ward group is 14.7% and 6.9% for stroke care unit group.[2] Advancing age, unconsciousness, severe stroke, large vessel stroke, atrial fibrillation, previous history of stroke, hyponatremia, high fasting blood sugar, and aspiration pneumonia were some of the predictors of mortality for a stroke.[3456] There is no consensus regarding the predictors of mortality in acute ischemic stroke among the researcher thus a definite scoring system for predicting the mortality of patient of acute ischemic stroke is still not practiced.
The management of acute stroke in low to middle-income countries is in snail's pace thus becoming a difficult task to handle the burden of acute stroke in health-care centers. Predicting the mortality of patient with stroke, identifying the high-risk patient and managing them with utmost care is still the unmet need of the country like Nepal. The data regarding the predictors of mortality from low to middle-income countries, where still the concept of stroke unit care is in infancy stage are limited.
This study is our endeavor to determine the predictor of the mortality of the patient of acute ischemic stroke in a tertiary care center in eastern Nepal by doing a retrospective analysis of patient of acute ischemic stroke admitted to the hospital.
MATERIALS AND METHODS
Study design
We conducted the retrospective study at B.P. Koirala Institute of Health Sciences, a pioneer tertiary care center in eastern Nepal. The center lacks separate neurology department and stroke unit care. We enrolled patient aged 18 years and older who were diagnosed as a case of ischemic stroke by treating physician and admitted to the Department of Internal Medicine from January 2012 to December 2016. Patients with Traumatic brain injuries were excluded from the study. The protocol was reviewed by Department research unit of Internal Medicine.
Study procedure
We retrieved the patient's hand written record file from the record section after getting permission from the head of the Department of Internal medicine and hospital director of the Institute. We recorded the data regarding the clinic-epidemiological profile and outcome of the patient. Glasgow coma scale (GCS) score, Blood pressure, respiratory rate, pulse rate, temperature, saturation of oxygen during triaging, and initial laboratory report were taken as participant's baseline value and recorded in pro forma.
Outcome measures
The primary outcome of the study population was the proportion of patient who had in-hospital mortality, and the secondary outcome was the length of hospital stay.
Statistical analysis
Data from the pro forma were filled into MS Excel 2010 and analyzed by the IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. For the descriptive analysis frequency, percentage, mean, median, standard deviation, and interquartile range were calculated and presented in tabular form whereas for inferential statistic independent t-test or Mann–Whitney test was applied as per need to find out the difference between groups. We consider values as statistically significant at 95% confidence interval if P < 0.05.
RESULTS
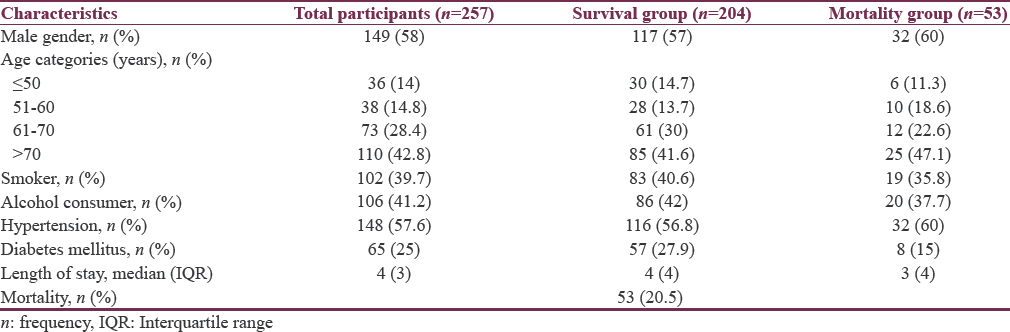
As shown in Table 1, we enrolled 257 patients with acute ischemic stroke in this study. The majority of the patient was male (58%). It occurred predominantly in the elderly population. Among the study population, 39.7% were a smoker and 41.2% had a history of alcohol intake. Most of the patient (57.6%) had a history of hypertension. Out of total participants, 53 patients (20.5%) patients died during hospital stay. The average length of hospital stay of admitted patients with acute ischemic stroke is 4 days.
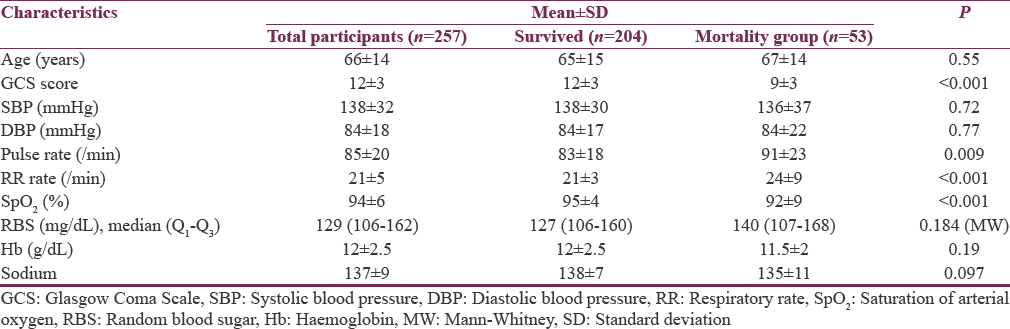
As shown in Table 2, patients with in-hospital mortality had significantly lower GCS score than those patients who survived (9 vs. 12, P < 0.001). There was no statistically significant difference in blood pressure in between survival and mortality group. Pulse rate (91 vs. 83, P = 0.009) and respiratory rate (24 vs. 21, P < 0.001) was significantly higher in mortality group than in survival group. Patients who died had a low saturation of oxygen than those who survived at baseline. There was no significant difference between the level of random blood sugar, haemoglobin, serum sodium in mortality and survival group.
DISCUSSION
In this 5-year retrospective analysis of acute ischemic stroke in a tertiary care center in eastern Nepal, The in-hospital mortality rate of acute ischemic stroke was 20.5%. This mortality rate is higher than reported by Dewan and Rana[7] from the tertiary care center in Central Nepal. This contrast in finding is due to the fact that the majority of patient recruited by them had the National Institutes of Health Stroke Scale (NIHSS) scale <15 which reflects a less severe form of stroke and may be due to the availability of specialized neurology care in their center. The in-hospital mortality rate of acute ischemic stroke was 4.5% in German stroke registry group as reported by Heuschmann et al.[8] This discrepancy in mortality rate from developed country reflects the urgent need of improvising the stroke care in middle- to low-income countries.
Modifiable risk factors such as hypertension, smoking, alcoholism, and diabetes mellitus were present in the majority of patient and similar findings were reported by studies in the other parts of Nepal.[910] These data coincide with the increasing prevalence rate of noncommunicable disease in the country[11] and raises the concern of stakeholder to focus on primary and secondary prevention of noncommunicable diseases.
In this study, the population who had in-hospital mortality had lower GCS score than those who survived (P < 0.001). GCS score is routinely practiced easy and noninvasive tool to prognosticate the traumatic brain injuries, stroke, and nontraumatic coma.[12] Mittal et al. reported GCS score of <8 as a predictor of the mortality,[13] which is similar to our finding.
The data showed that population who expired had a lower saturation of arterial oxygen than survival group (92% vs. 95%, P < 0.001). Hypoxia in acute ischemic stroke may be due to the aspiration pneumonia, brain stem stroke, heart failure, pulmonary embolism, and obstructive sleep apnea.[14] It increases the respiratory distress and may result in mortality of the patient. However, the data regarding the hypoxia and its impact on mortality of acute ischemic stroke are limited.
We found that higher respiratory rate as one of the predictors of the mortality of acute ischemic stroke (P < 0.001). Respiratory dysfunction in strokes such as Cheyne–Stokes breathing and tachypnea was associated with increased mortality of acute stroke.[15] Patient with tachypnea should be given utmost care and should evaluate them for the need of mechanical ventilation even at the emergency room.
Pulse rate was higher in mortality group than survival group. The causes of higher admission pulse rate are the large stroke, severe stroke (NIHSS >15), and atrial fibrillation.[16] The data from this study corroborate with Böhm et al. who reported in their study that faster admission heart rate predicts the mortality and poor functional outcome in a patient with acute ischemic stroke.[17] Admission pulse rate should be monitored carefully and those with higher pulse rate should be taken with utmost care.
Limitation of the study
This was hospital-based retrospective study and data were analyzed from available patient record file, so there were limited data to analyze many predictors of mortality of acute ischemic stroke such as the territory of stroke, the severity of the stroke, and complication of stroke. We could not find an etiological diagnosis for low GCS scale, hypoxia, and increase pulse rate in the population who had mortality.
Future direction
This study reflects the need of prospective study to analyze other clinical features and laboratory parameters to predict the mortality of acute ischemic stroke. This study highlights the need for validation of scoring system to predict the mortality of patient of acute ischemic stroke.
CONCLUSION
In a patient with acute ischemic stroke, poor GCS, lower arterial oxygen saturation, tachypneic, and higher pulse rate predicts the in-hospital mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Prof. Sanjib K. Sharma, Head of the Department of Internal Medicine, Dr. Pashupati Chaudhary, Deputy Hospital Director, B. P. Koirala Institute of Health Sciences for permitting the use of patient record files, Mr. Sunil Parujuli for helping us find the patient record files and editor of Grammarly application for English language editing.
REFERENCES
- The global burden of ischemic stroke: Findings of the GBD 2010 study. Glob Heart. 2014;9:107-12.
- [Google Scholar]
- Impact of stroke unit in a public hospital on length of hospitalization and rate of early mortality of ischemic stroke patients. Arq Neuropsiquiatr. 2013;71:774-9.
- [Google Scholar]
- Predictive variables for mortality after acute ischemic stroke. Stroke. 2007;38:1873-80.
- [Google Scholar]
- Long-term mortality and its risk factors in stroke survivors. J Stroke Cerebrovasc Dis. 2016;25:635-41.
- [Google Scholar]
- Early mortality and functional outcome after acute stroke in Uganda: Prospective study with 30 day follow-up. Springerplus. 2015;4:450.
- [Google Scholar]
- C-reactive protein and early mortality in acute ischemic stroke. Kathmandu Univ Med J (KUMJ). 2011;9:252-5.
- [Google Scholar]
- Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: The German Stroke Registers Study Group. Arch Intern Med. 2004;164:1761-8.
- [Google Scholar]
- A study of risk factors of stroke in patients admitted in manipal teaching hospital, Pokhara. Kathmandu Univ Med J (KUMJ). 2011;9:244-7.
- [Google Scholar]
- Retrospective analysis of stroke and its risk factors at Nepal Medical College Teaching Hospital. Nepal Med Coll J. 2006;8:269-75.
- [Google Scholar]
- Burgeoning burden of non-communicable diseases in Nepal: A scoping review. Global Health. 2015;11:32.
- [Google Scholar]
- The glasgow coma scale: History and current practice. 2002. Trauma. 4:91-103. Available from: http://www.tra.sagepub.com/cgi/doi/101191/1460408602ta233oa
- [Google Scholar]
- Identification of mortality-related predictive factors in hospitalized patients with ischemic stroke. Astrocyte. 2015;1:272-276.
- [Google Scholar]
- Hypoxaemia in acute stroke is frequent and worsens outcome. Cerebrovasc Dis. 2006;21:166-72.
- [Google Scholar]
- Cardiac and respiratory monitoring of acute stroke patients. Heart Lung. 1977;6:469-74.
- [Google Scholar]
- Heart rate monitoring on the stroke unit. What does heart beat tell about prognosis? an observational study. BMC Neurol. 2011;11:47.
- [Google Scholar]
- Impact of resting heart rate on mortality, disability and cognitive decline in patients after ischaemic stroke. Eur Heart J. 2012;33:2804-12.
- [Google Scholar]






