Translate this page into:
Predictors of Dropout from Outpatient Mental Health Services; A Study from Rohtak, India
Address for correspondence: Dr. Sidharth Arya, Institute of Mental Health, Pt BD Sharma University of Health Sciences, Rohtak - 124 001, Haryana, India. E-mail: draryasid3188@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Dropout from mental health services is problematic in both developed and developing nations and often leads to poor outcomes. There is a lack of hospital-based studies assessing the factors responsible for treatment dropout from mental health services in Indian settings. This study aims to contribute in that direction by presenting a study done in a tertiary care hospital in North India.
Methodology:
This was a hospital-based retrospective chart review carried out on randomly selected 139 patients at a tertiary hospital from January 1, 2014, to June 30, 2014. For this chart review, an abstraction form was designed that recorded six sociodemographic variables, nine clinical factors, and two outcome variables (more than one follow-up and active follow-up till 6 months).
Results:
Out of 139 patients, 53 patients dropped out after the first visit and 105 patients dropped out by the end of 6 months. Lower education status (odds ratio [OR] = 8.2, 95% confidence interval [CI]: 2.30–29.50), severe mental illness (OR = 2.6, 95% CI: 1.05–6.49), and early referral to clinical psychologist (CP) (OR = 7.8, 95% CI: 1.87–6.49) were predictors of better rates of follow-up after first visit. Lower education status (OR = 4.9, 95% CI: 1.45–17.08), early referral to CP (OR = 5.8, 95% CI: 2.09–38.35), and previous treatment history (OR = 8.9, 95% CI: 1.97–17.52) were predictors of better rates of follow-up at the end of 6 months.
Conclusion:
The findings that education status, diagnosis, utilizing services of CP, and psychiatric services in past are correlated with dropout rates may be helpful in targeting patients who are more vulnerable to dropping out of care in the given setting.
Keywords
Disengagement
dropout
mental health services
outpatient
treatment retention
INTRODUCTION
The problem of lack of availability of evidence-based psychiatric care[123] is further compounded by dropout from psychiatric care. Dropout may operationally be defined as the termination of contact with the services when there has not been a clinical resolution or an agreed termination.[4] Dropout from psychiatric care has been found to limit the possibility of monitoring and leads to a poor prognosis.[5] While some of the observed dropout may reflect reduced need for services, disengagement from mental health services can be a significant problem for individuals with mental illnesses that can lead to devastating consequences including exacerbation of psychiatric symptoms, repeated hospitalizations, homelessness, violence against others, and suicide.[67]
Many studies from the developed countries inform the correlates of dropping out from psychiatric care.[891011] World Mental Health Survey carried out by the World Health Organization comparing the dropout between high-income and lower income countries found that the dropout rate was higher in the latter group.[12] While dropout from psychiatric care is common in India, there is a paucity of hospital-based studies from India that have examined the factors contributing to dropout. This study aims to contribute toward reducing this gap.
Aims and objectives
The study aims to study the rates and predictors of dropout from psychiatric services from a tertiary care center in Rohtak, India.
METHODOLOGY
Patient records from a psychiatric clinic at a tertiary care hospital in North India were reviewed. The study center is a tertiary care center with inpatient and outpatient facilities for psychiatric illnesses. Patients seen at the clinic undergo comprehensive evaluation including a detailed interview. Each patient undergoes a thorough general physical examination and mental status examination. All the details are entered in a semi-structured pro forma. In many cases, patients also receive interventions from clinical psychologist (CP) and psychiatric social worker (PSW). The psychiatric diagnosis is made using International Classification of Diseases-10 criteria.
Treatment charts of every 10th patient seen at the initial visit between January 1, 2014, and June 30, 2014, were selected to obtain a representative sample of clinic patients. The chart review was done on July 1, 2015, to be reasonably sure that the termination of contact for the episode of care had occurred rather than it being a case of a few missed follow-ups.
Each chart was reviewed for the presence of a psychiatric diagnosis. If the chart did not contain this diagnosis and therefore was referred to another clinic, for instance neurology or internal medicine, the next 10th chart was chosen. Similarly, the chart of those patients whose care was terminated by the psychiatrist because of resolution of symptoms before 6 months were also excluded from the analysis and the next 10th chart was chosen. This yielded a final total of 139 charts.
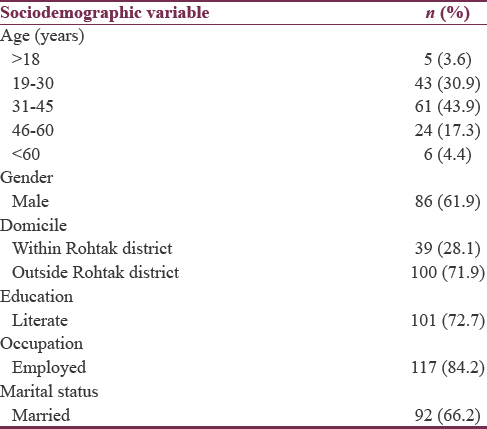
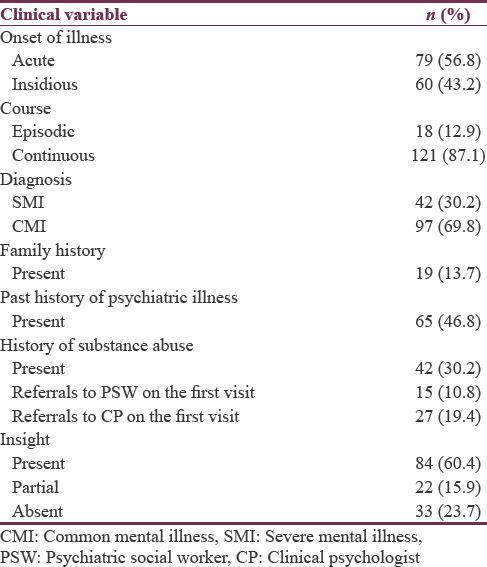
For this chart review, an abstraction form was designed that recorded six sociodemographic variables [Table 1] and nine clinical factors [Table 2] as well as two outcome variables (more than one follow-up and active follow-up till 6 months).
Statistical analysis
Of overall data, 95% was complete, and among 18 variables, only substance use category had missing values of around 15%, all other missing values for remaining variables were <10%. All these values were assumed to be as missing completely at random process, and multiple imputation technique was used to fill in the missing values. Odds ratio using binary logistic regression analysis for the categorical variables of more than one follow-up and active follow-up was calculated.
RESULTS
Table 1 shows the distribution of participants on the basis of sociodemographic variables.
It can be seen that 74.8% of the sample belonged to the age group of 18–45 years, 61.9% were males, 72.7% were literate, 84.2% were employed, 66.2% were married, and 71.9% resided outside the district in which the hospital is located.
Table 2 depicts the distribution of participants on the basis of clinical variables.
It shows that majority of the cases studied had presented with an acute onset of illness and a continuous course. About 30% of the cases studied had been suffering from severe mental illness (SMI). More than 3/4th of the cases studied were recorded to have at least partial insight into their illness. Almost half of the participants had a past history of psychiatric illness. Family history of mental illness was positive in 13.7% of the patients, and 30.2% had a history of substance abuse. About 10% and 20% of the cases had received a referral to the PSW and CP at the first visit, respectively.
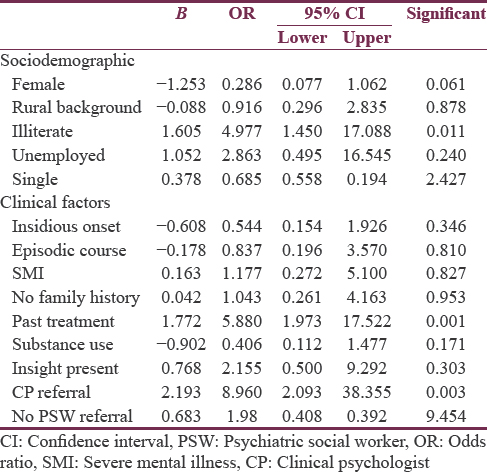
Tables 3 and 4 illustrate how various sociodemographic and clinical variables are associated with dropping out of psychiatric care. Dropout from psychiatric care was examined at 2 time points, namely, after initial visit and at the end of 6 months from the initial visit.
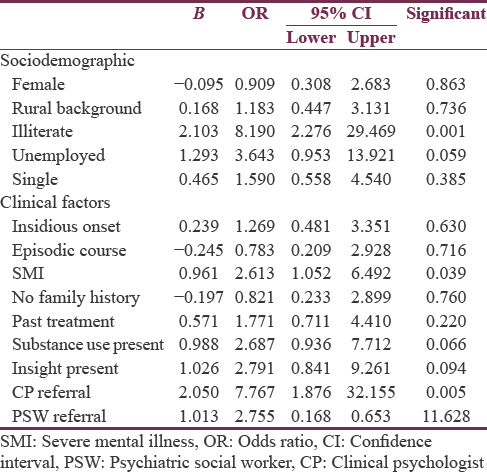
Out of 139 patients, 53 patients dropped out after the first visit and 105 patients dropped out by the end of 6 months. It can be seen that illiterate patients were about 8 times less likely to drop out after the first visit as compared to literate patients. Similarly, patients with SMI were about 2 times less likely to drop out after initial visit as compared to patients with common mental illness. It was also seen that patients who were offered referral to CP at the first visit were about 8 times less likely to drop out after the first visit.
When the dropout rates at the end of 6 months were examined in the light of sociodemographic and clinical variables, it was found that illiterate patients were 4 times more likely and patients receiving referral to CP were 8 times more likely to remain in psychiatric care at the end of 6 months. It was also revealed that patients who had a past history of treatment for a psychiatric illness were about 5 times more likely to be retained in the service.
DISCUSSION
This study examines the sociodemographic and clinical variables that predict dropping out from psychiatric care. In this study, it was found that about two out of five patients dropped out of care after first visit and about three out of four dropped out by the end of 6 months from the initial visit. Two Indian studies[1314] have previously reported on the subject of adherence to treatment in mental illnesses. Despite different patient characteristics and methodology, the dropout rate was similar to our study. The NCS study found that one-sixth (16.6%) of respondents who met diagnostic criteria for a serious mental illness had dropped out of treatment.[2] A review of literature that exclusively focused on individuals with schizophrenia or psychotic illnesses reported that one in four patients fail to adhere to treatment programs.[15] While the rates of dropout in our study are not directly comparable with the rates revealed in the studies quoted above because the patient population in our study included patients across all diagnostic categories, we might still surmise that dropout rates are higher in our center as compared to that in the developed countries. This might be explained by two circumstances that exist in developing countries like India. First, record keeping is poor, and the choices available for treatment are manifold. Hence, dropout from one center may not necessarily mean dropout from care.[16] Second, there is almost complete absence of community psychiatry facilities which can keep a track of patients in their catchment area.
In this study, it was found that illiterate patients and patients who were offered a referral to CP were less likely to drop out after the initial visit and at the end of 6 months after the initial visit. The diagnosis of SMI predicted lesser dropout after the first visit but not at the end of 6 months from the initial visit, whereas those with past history of contact with psychiatric services reported a better follow-up at the end of 6 months.
The correlates and reasons for disengagement from care suggested in previous studies[48910] include younger age, male gender, ethnic minority background, low social functioning, and social isolation, as evidenced by not being married or being out of contact with family, low educational attainment, and unemployment. In terms of clinical characteristics, individuals with a co-occurring serious mental illness and a substance use disorder have very high rates of treatment disengagement.
It appears counterintuitive that literate people should drop out at a rate which is 8 times higher than illiterate patients and many studies suggest the opposite viewpoint. In our setting, two surmises can be drawn from this finding. First, the socioeconomic status of literate patients is likely to be higher, and they might therefore be able to afford treatment at a private health facility. Second, it has been observed while working in the hospital that literate patients often perceive higher stigma related with mental health facility and hence are less likely to continue treatment.
Another interesting finding in this study is that referrals to CP have been associated with lesser dropout rates. Previous studies have reported higher preference of nonpharmacological treatment.[1718] It might indicate that steps should be taken to strengthen the multidisciplinary approach to the treatment of mental illnesses in Indian settings.
It also emerges that presence of SMI is a predictor of lower dropout rates after the initial visit but not at the end of 6 months. It maybe hypothesized that the treatment was sought for as long as the patients were symptomatic and discontinued once significant improvement occurred. However, this pattern is not clear and warrants additional research. Another important finding to come out of the study is the higher follow-up rate at the end of 6 months in those who have had contact with psychiatric services in the past. This might be due to positive experiences in the past with psychiatric services and as well as from better understanding of psychiatric illness due to greater exposure to psychiatric services.[19]
This study suffers from some limitations. First, the lack of psychiatry registers and community catchment model of services make it difficult to ascertain whether those patients who have dropped out from our service have sought care elsewhere or not. Second, the patient population studied is not homogeneous in terms of diagnosis, and the sample size is small. Third, the study has not evaluated client perspectives and their reasons for dropping out.
CONCLUSION
Drop out from psychiatric care adversely impact the outcomes in mental disorders. In our setting, it was found that some factors such as education status, diagnosis, utilizing services of CP, and psychiatric services in past have been found to correlate with dropout rates. This study needs to be replicated in other settings to examine if these findings are generalizable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank State Institute of Mental Health, Institute of Mental Health, Pt BDS UHS Rohtak for their cooperation in the study.
REFERENCES
- Prevalence of treated and untreated DSM-III schizophrenia. Results of a two-stage community survey. J Nerv Ment Dis. 1985;173:577-81.
- [Google Scholar]
- The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36:987-1007.
- [Google Scholar]
- Schizophrenic patients who were never treated – A study in an Indian urban community. Psychol Med. 1998;28:1113-7.
- [Google Scholar]
- Dropping out of care: Inappropriate terminations of contact with community-based psychiatric services. Br J Psychiatry. 2002;181:331-8.
- [Google Scholar]
- Use of a critical time intervention to promote continuity of care after psychiatric inpatient hospitalization. Psychiatr Serv. 2009;60:451-8.
- [Google Scholar]
- Longitudinal patterns of health system retention among veterans with schizophrenia or bipolar disorder. Community Ment Health J. 2008;44:321-30.
- [Google Scholar]
- Non-compliance in community psychiatry: Failed appointments in the referral system to psychiatric outpatient treatment. Nord J Psychiatry. 2002;56:151-6.
- [Google Scholar]
- Monitoring community psychiatric services in Italy: Differences between patients who leave care and those who stay in treatment. Br J Psychiatry. 2002;180:254-9.
- [Google Scholar]
- Predicting clinical and social outcome of patients attending ‘real world’ mental health services: A 6-year multi-wave follow-up study. Acta Psychiatr Scand Suppl. 2007;116:16-30.
- [Google Scholar]
- Mental health treatment dropout and its correlates in a general population sample. Med Care. 2007;45:224-9.
- [Google Scholar]
- Drop out from out-patient mental healthcare in the World Health Organization's World Mental Health Survey initiative. Br J Psychiatry. 2013;202:42-9.
- [Google Scholar]
- Factors affecting non-adherence among patients diagnosed with unipolar depression in a psychiatric department of a tertiary hospital in Kolkata, India. Depress Res Treat 2013 2013:809542.
- [Google Scholar]
- How often do patients with psychosis fail to adhere to treatment programmes. A systematic review? Psychol Med. 2003;33:1149-60.
- [Google Scholar]
- “Where do patients with severe mental illness go after dropping out of psychiatric care?” – An exploratory study using pathways to care approach. Asian J Psychiatr. 2014;11:74-5.
- [Google Scholar]
- Perspectives of young people on depression: Awareness, experiences, attitudes and treatment preferences. Early Interv Psychiatry. 2007;1:333-9.
- [Google Scholar]
- Patient preference for psychological vs. pharmacologic treatment of psychiatric disorders: A meta-analytic review. J Clin Psychiatry. 2013;74:595-602.
- [Google Scholar]
- Dropout from outpatient mental health care in the United States. Psychiatr Serv. 2009;60:898-907.
- [Google Scholar]






