Translate this page into:
Practices for respecting the newborn’s sleep-wake cycle: Interventional study in the neonatal intensive care unit
*Corresponding author: Saïd Boujraf, Clinical Neurosciences Laboratory, Faculty of Medicine and Pharmacy, University of Fez, Fez, Morocco. sboujraf@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Faez N, Hmami F, Boujraf S, Kojmane W, Atmani S. Practices for respecting the newborn’s sleep-wake cycle: Interventional study in the neonatal intensive care unit. J Neurosci Rural Pract. 2024;15:278-85. doi: 10.25259/JNRP_579_2023
Abstract
Objectives:
Premature newborns are exposed to a great deal of over-stimulation, which can affect their cerebral development. For better sleep, certain practices should be recommended. The aim of this study was to evaluate the effect of a professional training program on the improvement of practices promoting respect for the newborn’s sleep-wake cycle.
Materials and Methods:
This was an interventional study with a longitudinal, single-group, and before-and-after design. The experimental design followed a three-stage time series: Eight months before, three months after, then eight months after intervention. It targeted a comprehensive sample of 66 professionals. It took place between October 2020 and March 2022 at the Neonatal Intensive Care Unit of the Hassan II University Hospital in Fez, Morocco. It was based on an observation grid and a self-administered questionnaire, validated and tested with a Cronbach’s alpha reliability of 0.91.
Results:
The light environment showed significant differences between the 1st and 3rd step (3.3% vs. 45.0%; P = 0.02; confidence interval [CI] = 13.644–10.456) for knowledge and (13.3% vs. 78.3%; P = 0.01; CI = 14.412–10.888) for practices; the noise environment showed a positive improvement between the 2nd and 3rd intervention (31.7% vs. 41.7%; P < 0.001; CI = 5.954–2.913) for knowledge and (65.0% vs. 73.3%; P < 0.001; CI = 3.597–1.236) for practices, with an average of (8.98 ± 0.30–28.15 ± 0.48; CI = 3.806–1.094) between the 1st and 3rd step. Practices surrounding sleep and wakefulness reported significant improvement between the three periods (14.35 ± 0.22 vs. 18.10 ± 0.35 vs. 19.90 ± 0.35; P P < 0.001; CI = 4.647–2.853) for sleep and (13.25 ± 0.48 vs. 22.27 ± 0.59; P < 0.001; CI = 10.563–7.471) for wakefulness with statistically significant correlations between knowledge and practices (0.426**) for sleep and (0.606**) for wakefulness.
Conclusion:
The study demonstrated the positive impact of this sleep management and assessment program on the development of professional skills. Its implementation requires rigorous application of developmental support strategies for individualized care in neonatology.
Keywords
Newborn
Sleep
Wake
Knowledge
Practice
Professional care
INTRODUCTION
Sleep is fundamental to the survival and maturity of the organism.[1,2] It has several roles including thermoregulation, energy conservation, and neuronal detoxification as well as participating in brain plasticity.[3,4] Several studies have suggested evidence-based approaches to improving sleep in infants admitted to the neonatal intensive care unit (NICU).[5,6]
Protecting the developing brains of preterm infants remains a public health priority.[7] However, the over-stimulating environment does not offer the best conditions for the child to develop its sub-systems including the sleep-wake system. When the sleep-wake system is disorganized, the newborn expresses maladaptive behaviors including restless sleep.[8] Among other things, despite the high participation of professionals in health-related continuing education courses, the impact of training on knowledge acquisition and clinical practice is rarely evaluated. A significant number of healthcare professionals working in NICUs have received no training in developmental care including newborn sleep.[9,10]
Sleep disruption can have a negative effect on clinical outcomes, growth development, and also delay discharge from hospital.[11,12] However, in the neonatal environment, sleep deprivation is one of the strongest causes of discomfort and is a direct consequence of noise and light pollution, medical care, and negative attitudes to the sleep-wake cycle.[13,14] Certainly, the lighting environment must be taken into account when designing NICU layouts and fixtures.[15] It has been proven that exposure to intense or variable lighting, noise, and repetitive handling can be stressful leading to increased heart and respiratory rates and reduced blood oxygen levels.[16] These disorders can be avoided by a better understanding of sleep mechanisms.[6] Furthermore, nursing care and medical interventions had both positive and negative effects on the sleep-wake situation. Infants slept more peacefully when care was provided in accordance with best practice recommendations.[17]
MATERIALS AND METHODS
Study design and setting
This is an interventional study with a prospective, single-group, and before-and-after design.[18] It took place in the NICU of the Mother and Child Hospital of the Hassan II University Hospital in Fez, Morocco. It took place between October 2020 and Mai 2022 (19 months). The experimental design followed a chronological series in three stages: Eight months before, three months after, then eight months after intervention. The first stage (pre-intervention) enabled a pre-assessment of professional practices relating to respect for the sleep-wake cycle in neonatology. The intervention stage focused on a training program for professionals applying interactive teaching strategies. In addition, preventive measures against COVID-19 as well as small-group teaching were taken into consideration. The post-intervention phase was carried out in two stages. It was a progressive evaluation that assessed the level of adherence of professionals to the recommended practices and further determined the effects of the intervention on improving clinical practices. To avoid tracking bias, each new professional recruited to the unit received training before the intervention stage.
Criteria for judging the procedure: A judgment of significance, based on statistical analysis of the results to determine the differences with a significance threshold set at 5%. Results criteria are expressed by measuring frequencies and averages of changes in sleep-wake cycle practices after intervention.
Study participants
The study involved all healthcare professionals working in the highly specialized unit within the healthcare system; 66 multidisciplinary staff: doctors (n = 21), nurses (n = 27), and caregivers (n = 19). The choice of this population was justified by two inclusion criteria: Membership of the unit and care practice. The only exclusion criterion was refusal to participate in the study.
Study tools
This study is based on a local questionnaire survey, tested and validated by a team of experts with a Cronbach’s alpha reliability of 0.91 and an intra-class correlation coefficient of 0.8. A total of 160 variables were selected, rated on a three-statement Likert scale, and divided into four sections: Socioprofessional characteristics, knowledge, practices, and care environment. The completion rate was 91%. In addition, an observation and description grid of behavioral situations and care practices before and after was drawn up for 60 participants. It was divided into three criteria: (a) Light environment (b) Sound environment (c) Care activities. For this purpose, three possible ratings were grouped into a scale of low, medium, and high.
Statistical analysis
Data was processed using the Statistical Package for the Social Sciences version 30 software. Descriptive statistical analyses, Pearson correlations, analysis of variances (ANOVAs), and regression tests were performed to measure the strength of the relationship between variables.
Ethical consideration
This work is part of a doctoral project in Developmental Support Care in neonatology. Certainly, ethical principles have been established while adhering to the norms of scientific research. Approval has been obtained from the Hassan II University Hospital Ethics Committee under reference number 21/19. Participants’ right to privacy is protected by the anonymity and confidentiality of personal information. In addition, informed consent and the right to information were protected through an information sheet that was completed by participants before enrolment in the study.
RESULTS
Sociodemographic characteristics
18 (30.0%) doctors, 25 (41.6%) nurses, and 17 (28.3%) caregivers. 46 (76.6%) women and 34 (57.0%) are aged between 25 and 35 and 29 (48.3%) have been with the company for <5 years.
Professional knowledge assessment
Regarding their training in newborn sleep-wake, the pre-intervention step (T0) showed that 56 (93.3%) had not received any training in this area. The results of the post-intervention steps (T1) and (T2) showed a significant evolution in the participation of professionals in the training program, with a percentage of 58 (96.7%).
Concerning their knowledge of the role of sleep in child development, at the pre-intervention step, 22 (36.7%) were for improved concentration and consolidation of information memorized during wakefulness, 10 (16.7%) were for growth hormone and cortisol production, 9 (15.0%) for brain development while only 7 (11.7%) for visual system development and 2 (3.3%) for improved humanitarian responses. This conception evolved moderately in post-intervention step 1, with a frequency of over 48 (80.0%) in the majority of items. The post-intervention 2, on the other hand, showed a high degree of evolution in all the items presented, with an agreement of over 58 (96.7%) participants.
In terms of their knowledge of sleep phases, the pre-intervention highlighted the participants’ difficulty in choosing the right answer. Certainly, only 17 (28.3%) were in agreement with the presence of three phases (deep, paradoxical, and intermediate), 10 (16.7%) were for two phases (calm and restless) and 8 (13.3%) were for a single phase (rapid sleep). Thus, 25 (41.7%) chose no answer. Post-intervention 1 saw an improvement in responses, with a frequency of 45 (75.0%) for the three-phase item. In the second post-intervention step, 57 (95.0%) participants agreed with this response.
For their opinion on the consequences of sleep deprivation, the pre-intervention step highlighted a lack of knowledge on most of the proposed items. Certainly, only 19 (31.7%) agreed with lack of attention and behavioral problems, 9 (15.0%) agreed with reduced immune defenses, loss of appetite, and sudden infant death syndrome. Thus, only 2 (3.3%) agreed with the risk of obesity or diabetes, increased pain perception, and arterial hypertension. Post-intervention 1 marked an improvement in participants’ knowledge of the same items, with agreement exceeding 19 (31.7%) in most cases. Among other things, post-intervention 2 showed an evolution in responses, with an agreement of over 51 (85.0%).
Professional practice assessment
Within the framework of practices surrounding newborn awakening, the pre-intervention step illustrated that 26 (43.3%) ensure cleanliness and warmth of hands and equipment before touching the baby. The 11 (18.3%) said that they moved to the side where the baby’s face was to stimulate his gaze, but only 6 (10.0%) took advantage of his awakening for feeding and care, 2 (3.3%) waited for him to stabilize before starting care, and none 0 (0.0%) took advantage of the waking moment to observe and communicate with the baby. Among other things, these attitudes changed at post-intervention 1, with a frequency of over 44 (73.3%). At post-intervention 2, professional recruitment, which exceeded recommended practices by 52 (86.7%), showed a significant improvement.
Concerning practices related to newborn sleep, at the pre-intervention stage, none of the 0 (0.0%) participants confirmed respecting the baby’s sleep-wake rhythm, splitting up the care, taking the time to put the baby back to sleep after care, and taking advantage of this time to rigorously observe the baby’s behavior. However, 55 (91.7%) confirmed that they force the newborn to wake up at feeding time, and 56 (93.3%) force him to wake up at nursing time. The latter behaviors decreased significantly in the post-intervention 1, with only 9 (15.0%) and 15 (25.0%) in succession. The post-intervention 2 confirmed a considerable evolution, with an attachment exceeding 54 (90.0%) to practices promoting respect for newborn sleep.
Among other things, the results of the evaluation grid enabled us to establish a clear description of professional practices based on spatial, temporal, and behavioral dimensions. The intervention focused not only on professional skills but also on the care environment. As a result, observation of the attitudes and practices surrounding the newborn’s sleep-wake was poorly assessed in the pre-intervention step. More than 38 (63.3%) were unable to identify the state of alertness and feeding planning on awakening with an absence of 0 (0.0%) behavioral observation, and communication with the baby on awakening. On the other hand, in the post-intervention 1, an evolution was noted in all practices with an average rating of over 22 (33.3%). Certainly, in post-intervention 2, observation confirmed a better improvement in practices with a high ranking of over 56 (93.3%) of participants. In fact, behavior observation showed little difference in the two post-interventions [Table 1].
| Variable/statement | 8 months before | 3 months after | 8 months after | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | Higher | Low | Medium | Higher | Low | Medium | Higher | |
| Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | Nb. (%) | |
| Detects baby’s situation of alertness | 38 (63.3) | 20 (33.3) | 2 (3.3) | 6 (10.0) | 24 (40.0) | 30 (50.0) | 1 (1.7) | 3 (5.0) | 56 (93.3) |
| Plan feeding and care upon awakening | 38 (63.3) | 20 (33.3) | 2 (3.3) | 6 (10.0) | 22 (36.7) | 32 (53.3) | 1 (1.7) | 3 (5.0) | 56 (93.3) |
| Helps baby fall asleep after care | 60 (100.0) | 0 (0.0) | 0 (0.0) | 6 (10.0) | 22 (36.7) | 32 (53.3) | 1 (1.7) | 3 (5.0) | 56 (93.3) |
| Takes advantage of his sleep/wake to observe behavior | 60 (100.0) | 0 (0.0) | 0 (0.0) | 19 (31.7) | 21 (35.0) | 20 (33.3) | 19 (31.7) | 20 (33.3) | 21 (35.0) |
| Ensures warm hands and equipment | 30 (50.0) | 22 (36.7) | 8 (13.3) | 6 (10.0) | 22 (36.7) | 32 (53.3) | 1 (1.7) | 3 (5.0) | 56 (93.3) |
| Take advantage of calm wakefulness for effective communication | 52 (86.7) | 8 (13.3) | 0 (0.0) | 6 (10.0) | 22 (36.7) | 32 (53.3) | 1 (1.7) | 3 (5.0) | 56 (93.3) |
Nb.(%): Number and percentage
With regard to the lighting modes used in newborn rooms in the pre-intervention step, none of the 0 (0.0%) participants proved the presence of continuous dim lighting, 58 (96.7%) stated that they rarely alternate between dim and cyclic lighting, while they affirmed the absence of a well-defined lighting mode in the NICU. This situation evolved moderately in the post-intervention 1, with agreement exceeding 32 (53.3%) for alternating between dimmed and cyclic lighting. This type of lighting underwent a major change in the post-intervention 2, with a remarkable 53 (88.3%) of participants agreeing.
With regard to the presence of light adapted to the newborn’s sleep-wake cycle, the statistics show a very significant positive change in the average responses. Thanks to the training program, significant differences were noted between the 1st and 2nd intervention steps (13.3% vs. 65.0%; P = 0.02; confidence interval [CI] = 12.557–8.576), between the 1st and 3rd steps (13.3% vs. 78.3 %; P = 0.01; CI = 14.412–10.888) and between the 2nd and 3rd steps (65.0% vs. 78.3%; P < 0.001; CI = 6.757–3.343). This confirms a significant improvement in staff light management practices in the NICU [Figure 1].
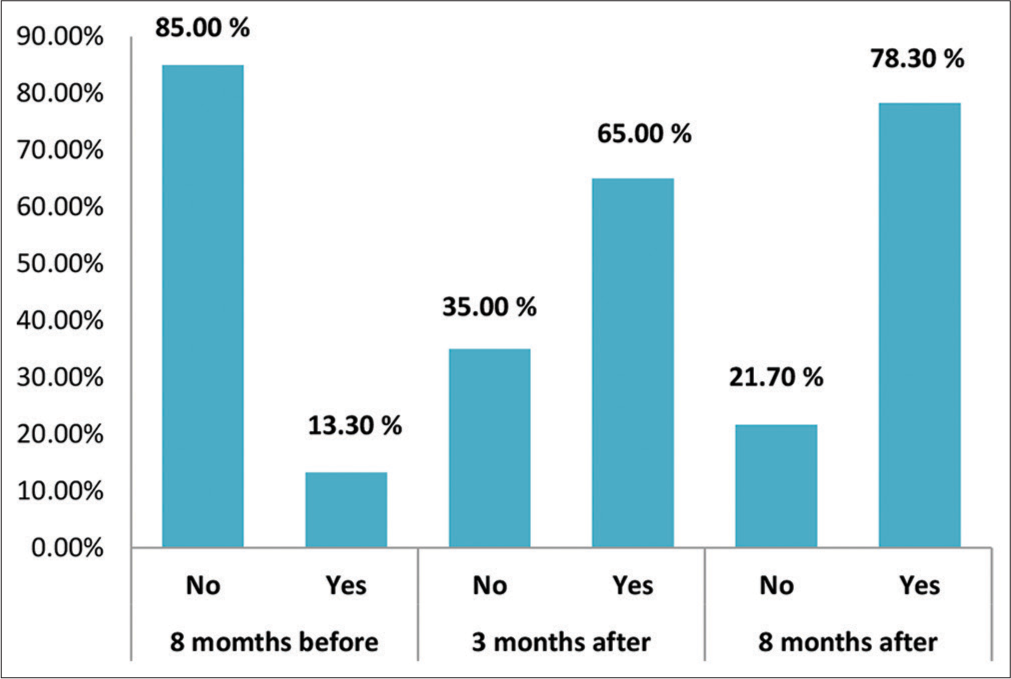
- Brightness adapted to the newborn’s sleep-wake cycle.
With regard to neonatal reactions to light, the results showed that for most items, there were significant differences between the 1st and 2nd step (3.3% vs. 28.3%; P = 0.02; CI = 10.673–6.327). Similarly, there were differences between 1st and 3rd step (3.3% vs. 45.0%; P = 0.02; CI = 13.644–10.456) and between 2nd and 3rd step (28.3% vs. 45.0%; P < 0.001 CI = 3.559–1.408). This explains the considerable evolution in professional knowledge [Table 2].
| Variable/statement | 8 months before | 3 months after | 8 months after | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No (%) | Yes (%) | No (%) | Yes (%) | No (%) | Yes (%) | T0 versus T1 | T0 versus T2 | T1 versus T2 | |
| Modification of physiological parameters | 96.7 | 3.3 | 65.0 | 35.0 | 55.0 | 45.0 | P=0.002 | P<0.001 | P<0.001 |
| Sleep disturbance | 86.7 | 13.3 | 36.7 | 63.3 | 16.7 | 83.3 | P=0.003 | P<0.001 | P=0.002 |
| Ocular damage | 95.0 | 5.0 | 71.7 | 28.3 | 61.7 | 38.3 | P=0.002 | P=0.002 | P<0.001 |
| Circadian rhythm disturbance | 95.0 | 5.0 | 71.7 | 28.3 | 58.3 | 1.7 | P=0.004 | P<0.001 | P<0.001 |
| Slower psychomotor development | 96.7 | 3.3 | 68.3 | 19.0 | 61.7 | 38.3 | P=0.003 | P<0.001 | P=0.002 |
T0: Preintervention step, T1 and T2: Postintervention steps, P-value: Probability, %: Percentage
Regarding the noise environment in the NICU, the decrease in noise near the newborn also marked an evolution. Whereas (10.0% vs. 65.0%; P = 0.02; CI = 12.061–9.206) between steps 1 and 2, participants confirmation gradually increased to (10.0% vs. 73.3%; P = 0.02; CI = 13.221–11.212) between steps 1 and 3. Moreover, this practice peaked in the last study between the 2nd and 3rd intervention steps (65.0% vs. 73.3%; P < 0.001; CI = 3.597–1.236). This explained the adoption of positive attitudes toward noise.
On the subject of neonatal reactions to noise, the results showed a significant change in professional attitudes. Certainly, in most items, significant differences were noted between the 1st and 2nd steps (1.7% vs. 31.7%; P = 0.02; CI = 16.756–12.710). Similarly, there were differences between 1st and 3rd step (1.7% vs. 41.7%; P = 0.02; CI = 20.402–17.932) and between 2nd and 3rd step (31.7% vs. 41.7%; P < 0.001; CI = 5.954–2.913). This confirms a positive development in professional knowledge after the training program [Table 3].
| Variable/statement | 8 mois avant (T0) | 3 mois après (T1) | 8 mois après (T2) | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No (%) | Yes (%) | No (%) | Yes (%) | No (%) | Yes (%) | T0 versus T1 | T0 versus T2 | T1 versus T2 | |
| Weight loss | 98.3 | 1.7 | 68.3 | 31.7 | 58.3 | 41.7 | P=0.002 | P<0.001 | P<0.001 |
| Irregular breathing | 98.3 | 1.7 | 68.3 | 31.7 | 58.3 | 41.7 | P=0.003 | P<0.001 | P=0.002 |
| Peripheral vasoconstriction | 98.3 | 1.7 | 75.0 | 25.0 | 58.7 | 43.3 | P=0.002 | P=0.002 | P<0.001 |
| Decrease in oxygen saturation | 96.7 | 3.3 | 70.0 | 30.0 | 58.3 | 41.7 | P=0.002 | P<0.001 | P<0.001 |
| Restless sleep | 85.0 | 15.0 | 36.7 | 63.3 | 30.3 | 70.0 | P<0.001 | P<0.001 | P<0.001 |
| Irregular heartbeat | 96.7 | 3.3 | 68.3 | 31.7 | 58.3 | 41.7 | P=0.003 | P<0.001 | P<0.001 |
T0: Preintervention step, T1 and T2: Postintervention steps, P-value: Probability, %: Percentage
With regard to noise-related attitude averages, the ANOVA recorded significant differences (P < 0.001) both between the first and second steps (from 8.98 ± 0.30 to 23.72 ± 0.86; CI = 12.473–7.961) and between the first and third steps (8.98 ± 0.30–28.15 ± 0.48; CI = 3.806–1.094). This may be interpreted as an improvement in abilities related to daily attitudes to noise, and those related to the training program [Figure 2].
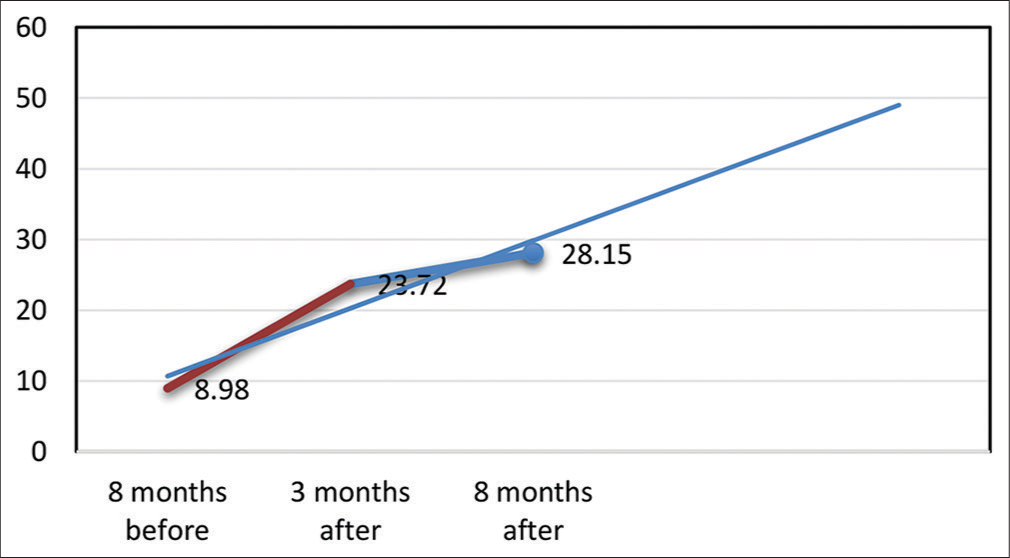
- Average attitudes to noise. Red Line: Pre-intervention evaluation step, Blue Line: Post-intervention evaluation step.
Regarding ANOVA analyses of newborn sleep, practices showed a statistically significant difference between the three periods (14.35 ± 0.22 vs. 18.10 ± 0.35 vs. 19.90 ± 0.35; P < 0.001; CI = 4.647–2.853), which explains the significant improvement in this item after the intervention period. For the averages of practices surrounding newborn awakening, ANOVA analyses showed statistically significant differences between 1st and 2nd step (13.25 ± 0.48 vs. 22.27 ± 0.59; P < 0.001; CI = 10.563–7.471), similarly, the figures proved significant between 1st and 3rd step (24.98 ± 0.48; P < 0.001; CI = 13.175–10.292), also between 2nd and 3rd step. This explains the improvement in professional attitudes in the post-intervention period.
For better verification of correlations between variables, it proved essential to combine the two post-intervention periods for those variables that did not show a considerable difference between them. According to the data from the present study, there was a statistically significant correlation between knowledge relating to the development of the sleep-wake situation and professional practices (0.345**) and those relating to wakefulness (0.523**) in the first pre-intervention step. In the second, post-intervention, this knowledge confirmed more positive correlations with the two practices studied, through a progression of results which are presented successively as the following: (0.426**) and (0.606**) [Table 4].
| Intervention steps | Knowledge: Sleep-wake situation | Practices related to sleep | Practices related to awakening |
|---|---|---|---|
| Before intervention | |||
| Knowledge: Sleep-wake state | |||
| Pearson’s correlation | 1 | 0.345** | 0.523** |
| Sig. (bilateral) | 0.007 | 0.000 | |
| n | 60 | 60 | 60 |
| Practices related to sleep | |||
| Pearson’s correlation | 0.345** | 1 | 0.442** |
| Sig. (bilateral) | 0.007 | 0.000 | |
| n | 60 | 60 | 60 |
| Practices related to awakening | |||
| Pearson’s correlation | 0.523** | 0.442** | 1 |
| Sig. (bilateral) | 0.000 | 0.000 | |
| n | 60 | 60 | 60 |
| After intervention | |||
| Knowledge: Sleep-wake situation | |||
| Pearson’s correlation | 1 | 0.426** | 0.606** |
| Sig. (bilateral) | 0.000 | 0.000 | |
| n | 120 | 120 | 120 |
| Practices related to sleep | |||
| Pearson’s correlation | 0.426** | 1 | 0.636** |
| Sig. (bilateral) | 0.000 | 0.000 | |
| n | 120 | 120 | 120 |
| Practices related to awakening | |||
| Pearson’s correlation | 0.606** | 0.636** | 1 |
| Sig. (bilateral) | 0.000 | 0.000 | |
| n | 120 | 120 | 120 |
DISCUSSION
To the best of our knowledge, the present study is the first in this context to evaluate the impact of a training program on the improvement of practices that promote respect for the newborn’s sleep-wake cycle in the NICU. Moreover, the study population covers a wide range of specialties with more than half of them young and with <5 years’ professional experience. The 56 (93.3%) of them claimed to have no training in the near-intervention period. These characteristics explain the need for professional training. Professional training is an essential component of healthcare system management. Indeed, it is the main means of maintaining or improving the quality of healthcare workers’ work. It is also the most important way of adapting professional behavior to current needs and keeping pace with their evolution.[19] And yet, for better professional development, healthcare personnel are increasingly taking part in continuing education courses to keep pace with ongoing advances and changes in the medical field. This can only be achieved if training improves knowledge and skills, which in turn, translates into better clinical decision making.[20,21]
In terms of knowledge and practical conduct relating to the lighting environment, the results showed a significant improvement in light management and the preservation of newborn sleep. Significant differences were noted between the 1st and 3rd steps (3.3% vs. 45.0%; P = 0.02; CI = 13.644– 10.456) for knowledge and (13.3% vs. 78.3%; P = 0.01; CI = 14.412–10.888) for practices. In this context, a number of studies have shown that lighting control in the NICU is essential.[22,23] Among other things, noise and lighting levels in the NICU are well-known factors that disrupt sleep organization and increase arousals or the number of transitions between sleep condition.[24] It would therefore be advisable to comply with organizational standards to prevent neonatal stress.[15] This explains the importance of professional practices favoring the control of light intensity within the care of hospitalized premature infants.[25] Furthermore, in post-intervention 2, the alternation between subdued and cyclic lighting was widely endorsed by over 53 (88.3%) of participants. Certainly, in addition to circadian biology, attention must be paid to the importance of lighting cycles in the care of newborns, especially premature babies.
Adherence to practices aimed at managing these two lighting methods helps to create an environment adapted to the needs of premature babies with a view to physiological stability and reduced motor activity.[26]
Regarding knowledge and practical attitudes related to the noise environment, the results showed a positive improvement between the 2nd and 3rd intervention steps (31.7% vs. 41.7%; P < 0.001; CI = 5.954–2.913) for knowledge and (65.0% vs. 73.3%; P < 0.001; CI = 3.597–1.236) for practices, with an average of (8.98 ± 0.30 –28.15 ± 0.48; CI = 3.806–1.094) between the first and third step. In addition, the presence of noise in the care environment was specifically identified as a particular concern requiring constant monitoring.[27] With this in mind, care standards recommend noise reduction protocols that include behavioral and infrastructural modifications. In this context, behavioral modification of staff activity is the most cost-effective strategy.[28,29]
With regard to newborn sleep knowledge, more than 57 (95.0%) scored high learning in this area in the post-intervention step 2. Among other things, healthcare professionals should actively disseminate sleep knowledge to help parents interpret infant sleep behaviors and consider multiple intervention and assessment strategies to improve not only their practices but also parental sleep-related knowledge.[11] However, research has shown that professionals including pediatricians, who are responsible for children with sleep disorders, have limited knowledge and training in this field. It is essential to provide training for professionals in charge of children in neonatology or pediatrics. These professionals should be given specific information on the organization of sleep as well as the elements of screening, diagnosis, and treatment of sleep problems.[30]
In this study, practices surrounding sleep and wakefulness reported significant improvement between the three intervention periods. (14.35 ± 0.22 vs. 18.10 ± 0.35 vs. 19.90 ± 0.35; P < 0.001; CI = 4.647–2.853) for sleep and (13.25 ± 0.48 vs. 22.27 ± 0.59; P < 0.001; CI = 10.563–7.471), for wakefulness. In addition, statistically significant correlations were marked between knowledge and practices relating to the development of the sleep-wake condition, with a progression between the pre- and post-intervention steps. (0.426**) for sleep and (0.606**) for wakefulness. This confirms the positive impact of the training program on improving professional attitudes toward respecting the sleep-wake of hospitalized newborns.[10] Of course, intervention evaluation involves at least four dimensions: participant satisfaction, learning (knowledge and skills), behavior change (transfer of knowledge and skills to the workplace), and outcomes (impact on patients).[21,31]
Moreover, the organization of the sleep-wake cycle is an essential component of the interaction between staff and the newborn. A calm, non-harmful environment, and individualized care practices can play an active role in the newborn’s development.[24,32] However, it is wise for professionals to look for factors that could contribute to the organization of a child’s sleep, and to be aware of the harmful effects of irregular or poor-quality sleep, which can have risks on the child’s development.[33]
Limitations and recommendation
The study was limited by the small number of participants and the fact that it was conducted in a single NICU. Thus, following the COVID-19 pandemic, changes were made to the planning of the training sessions while respecting the regulations assigned by the hospital. This had an impact on the extension of the data collection period as well as on the quality of the expected results. It is recommended that further studies, under more normal conditions, be carried out into the various aspects of Developmental Supportive Care and related to the results of this study.
CONCLUSION
This study demonstrated the positive impact of a professional training program on sleep-wake cycle compliance in the NICU. Significant cognitive, behavioral, and procedural improvements were recorded. On the other hand, preventing or reducing sources of stress in newborns and respecting their sleep-wake cycle can be a challenge. Implementing this sleep management and assessment program requires reinforcement of the efforts of both professionals and managers using a combination of environmental and behavioral interventions aimed at individualized care in neonatology.
Acknowledgment
The researchers would like to thank all the staff of the NICU department of the Hassan II University Hospital of Fez- Morocco for their commitment and involvement throughout this study.
Authors’ contributions
This study was carried out in collaboration between all authors. The lead author (Faez Naima) conceived the idea of the title, developed the proposal, analyzed the data, interpreted the result, and prepared the manuscript for publication in your journal. The 2nd author (Hmami Fouzia) participated approved the idea of the title, participated in the comments, assisted in the analysis of the data, and interpretation of the result. The 3rd author (Boujraf Said) participated in the comments, assisted in the analysis of the data interpretation of the result and finalizing work for submission. The 4th author (Kojmane Widade) participated in the comments and assisted in the analysis of the data and interpretation of the result. The 5th author (Atmani Samir) participated in the comments and editing of the manuscript, assisted in the analysis of the data and interpretation of the result and sending for publication in your journal provenance and peer review.
Disclaimer
This paper is part of the researcher’s PhD study, and the contents are allowed to be mentioned in the thesis.
Ethical approval
The approval has been obtained from the Hassan II University Hospital Ethics Committee under reference number 21/19.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Sleep and sleep disturbances In: Sameroff AJ, Lewis M, Miller SM, eds. Handbook of developmental psychopathology. United States: Springer; 2000. p. :309-25.
- [CrossRef] [Google Scholar]
- Infant sleep and paternal involvement in infant caregiving during the first 6 months of life. J Pediatr Psychol. 2010;36:36-46.
- [CrossRef] [PubMed] [Google Scholar]
- Waking up too early-the consequences of preterm birth on sleep development: Preterm birth and sleep development. J Physiol. 2018;596:5687-708.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effect of nesting and swaddling on sleep duration and arousal frequency among preterm neonates: A randomized clinical trial. J Caring Sci. 2022;11:126-31.
- [CrossRef] [PubMed] [Google Scholar]
- How to improve sleep in a neonatal intensive care unit: A systematic review. Early Hum Dev. 2017;113:78-86.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding sleep. The letter from childhood and adolescence. 2008;. ;71:25-32.
- [CrossRef] [Google Scholar]
- Is it possible to protect the preterm infant brain and to decrease later neurodevelopmental disabilities? Arch Pediatr. 2008;15:S31-41.
- [CrossRef] [PubMed] [Google Scholar]
- Les soins du développement: Des soins sur mesure pour le nouveau-né malade ou prématuré Montréal (Québec): Editions du CHU Sainte-Justine; 2006. p. :194.
- [Google Scholar]
- Behavioral interventions for infant sleep problems: A randomized controlled trial. Pediatrics. 2016;137:e20151486.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of a developmental care training course on the knowledge and satisfaction of health care professionals in neonatal units: A multicenter study. Pediatr Neonatol. 2016;57:97-104.
- [CrossRef] [PubMed] [Google Scholar]
- Infant sleep problems: The sleep characteristics of the “Don't Know” response. J Adv Nurs. 2018;74:181-9.
- [CrossRef] [PubMed] [Google Scholar]
- The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232-46.
- [CrossRef] [PubMed] [Google Scholar]
- Toward a synactive theory of development: Promise for the assessment and support of infant individuality. Infant Ment Health J. 1982;3:229-43.
- [CrossRef] [Google Scholar]
- Are neonatal units an inhospitable environment? Perceptual abilities and sensory expectations of preterm infants in the hospital. Rev Méd Périnatale. 2016;8:141-8.
- [CrossRef] [Google Scholar]
- Effect of procedure light on the physiological responses of preterm infants: Effects of procedure light on neonates. Jpn J Nurs Sci. 2010;7:76-83.
- [CrossRef] [PubMed] [Google Scholar]
- Light reduction capabilities of homemade and commercial incubator covers in NICU. ISRN Nurs. 2013;2013:502393.
- [CrossRef] [PubMed] [Google Scholar]
- Nonnutritive sucking and facilitated tucking relieve preterm infant pain during heel-stick procedures: A prospective, randomised controlled crossover trial. Int J Nurs Stud. 2012;49:300-9.
- [CrossRef] [PubMed] [Google Scholar]
- Program theory evaluation: Logic analysis. Eval Program Plann. 2011;34:69-78.
- [CrossRef] [PubMed] [Google Scholar]
- Continuing the education of health workers: A workshop manual, Geneva: World Health Organization, 1988, 185 pp. J Continuing Educ Health Profess. 1990;10:285-6.
- [CrossRef] [Google Scholar]
- Staff opinions regarding the newborn individualized developmental care and assessment program (NIDCAP) Early Hum Dev. 2007;83:425-32.
- [CrossRef] [PubMed] [Google Scholar]
- Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325:1338-41.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing light and noise levels before and after a NICU change of design. J Perinatol. 2021;41:2235-43.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived timing of vestibular stimulation relative to touch, light and sound. Exp Brain Res. 2009;198:221-31.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of nursery environment on state regulation in very-low-birth-weight premature infants. Infant Behav Dev. 1990;13:287-303.
- [CrossRef] [Google Scholar]
- Iatrogenic environmental hazards in the neonatal intensive care unit. Clin Perinatol. 2008;35:163-81.
- [CrossRef] [PubMed] [Google Scholar]
- Rest-activity patterns of premature infants are regulated by cycled lighting. Pediatrics. 2004;113:833-9.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of a noise reduction quality improvement project upon sound levels in the open-unit-design neonatal intensive care unit. J Perinatol. 2010;30:489-96.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of the effect of the efficiency of noise at different intensities on the DNA of the newborns. Noise Health. 2016;18:7.
- [CrossRef] [PubMed] [Google Scholar]
- Sustaining a “culture of silence” in the neonatal intensive care unit during nonemergency situations: A grounded theory on ensuring adherence to behavioral modification to reduce noise levels. Int J Qual Stud Health Wellbeing. 2014;9:22523.
- [CrossRef] [PubMed] [Google Scholar]
- Staff perception one year after implementation of the the newborn individualized developmental care and assessment program (NIDCAP) J Pediatr Nurs. 2010;25:89-97.
- [CrossRef] [PubMed] [Google Scholar]
- Necessary resources and barriers perceived by professionals in the implementation of the NIDCAP. Early Hum Dev. 2013;89:649-53.
- [CrossRef] [PubMed] [Google Scholar]
- Decreased arousals among healthy infants after short-term sleep deprivation. Pediatrics. 2004;114:e192-7.
- [CrossRef] [PubMed] [Google Scholar]
- Childhood sleep disorders in premature infants that hospitalized in neonatal intensive care unit in neonatal period. Ann Med Res. 2020;27:69.
- [CrossRef] [Google Scholar]






