Translate this page into:
Posterior approach for giant S1 neurofibroma in Von Recklinghausen's disease: Is total resection realistic?
Address for correspondence: Dr. Ashish Kumar, Department of Neurosurgery, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad, Andhra Pradesh - 500 082, India. E-mail: drashishmch@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bilateral sacral neurofibromas are uncommonly seen in neurofibromatosis type 1 (NF1) also known as Von Recklinghausen's disease. They often grow to enormous dimensions before detection owing to bone scalloping. Resections of “giant” S1 neurofibromas are difficult due to the limitations of operative window in sacrum and critical functions associated with S1 nerve root. We report a case of bilateral S1 neurofibromas in a patient of NF1 where she had a giant left-sided neurofibroma with extensive bone erosion and a small fusiform neurofibroma on the right side. The tumor was excised completely on the left and near totally on the right side via posterior approach. There were no postoperative neurological deficits and the patient recovered well. Usually, complete excision harbors the chances of postoperative neurological deficits due to the eloquence of the nerve root involved and complete resection without significant morbidity seems unrealistic. However, excision of giant ones may not result in grave deficits always if the patient is neurologically intact before surgery. Also, in selected patients, only posterior approach may suffice for giant neurofibromas with extensive bone scalloping and complete removal can be attempted successfully despite narrow corridors.
Keywords
Complete resections
giant sacral neurofibromas
posterior approach
Introduction
Neurofibromatosis type 1 or Von Recklinghausen's disease is one of the common autosomal dominant diseases characterized by multiple neurofibromas along with cutaneous manifestations. It occurs due to mutations in NF1 gene located on chromosome 17 responsible for overexpression of neurofibromin protein. Multiple central and peripheral nervous system tumors are commonly encountered in NF1. Sacral tumors are rare and they account for only 7% of all the intraspinal neoplasms. Sacral neurofibromas deserve special mention as they frequently present late in the presacral space after growing to enormous sizes. Giant sacral neurofibromas are still uncommon and anterior/posterior approaches have been described in the literature for their excision. However, complete resections may remain difficult in certain cases while employing only posterior approach. Also, S1 root is considered to be an eloquent root chiefly responsible for foot plantar flexion. Hence, complete resectibility remains doubtful. We report a 15-year-old girl with NF1 presenting with bilateral S1 neurofibromas (one giant and one small) and discuss its management strategy in terms of approach and completeness of resection.
Case Report
A 15-year- old female presented with insidious onset progressive low backache with pain radiating to left lower limb for past 1 year. The pain used to aggravate on walking and relieved on lying down. There was no history suggestive of parasthesias or weakness in the limbs. There was no sphincteric involvement too. On general examination, multiple swellings were found to be present over the back and limbs suggestive of subcutaneous neurofibromas. Also, there were multiple café-au-lait spots of various sizes ranging from 5 mm to more than 15 mm over the low back and the left leg. No other features suggestive of NF1 were detected. No focal neurological deficits were elicited during examination especially foot plantar flexion. Reflexes were normal and plantars down going. Magnetic resonance imaging (MRI) of lumbosacral spine revealed a well-defined lobulated homogenously enhancing mass extending from L5 to S2, involving S1 nerve root bilaterally and encroaching the neural foramina along with significant paraspinal extension on left and scalloping of posterior S1 and S2 vertebral body. The lesion was isointense on T1-weighted images, hyperintense on T2-weigheted images, and showed homogenous contrast enhancement [Figure 1]. Computed tomography (CT) scan showed extensive scalloping of sacrum [Figure 2]. Usually, it would seem impossible to reach the anterior pre-sacral space from posterior approach. However, if a long standing benign lesion scallops the bone, only laminectomy up to the sacral foramina posteriorly suffices and also, the tumor gives additional space once debulking is commenced. Nonvascular pathologies like schwannomas with relatively lesser anterior extensions are perfect for this type of approach where the anterior part of residual tumor may be pulled back in the bony cavity once the posterior half is excised. Our patient underwent laminectomy from L5 to S3 up to the sacral foramina bilaterally. The lamina was thin and a large lesion was seen on the right side. A giant, capsulated, firm, mild to moderately vascular tumor was arising from left S1 nerve root. There was another smaller fusiform swelling arising from the right S1 nerve root extending into the paraspinal region through the S1–S2 neural foramina. Complete excision was performed on the left side as no viable fascicles were encountered while subcapsular partial resection was done on the right, leaving behind continuing nerve fascicles. Anatomical contiguity was not observed on the left side while it was preserved on the right after the procedure. The tumor was completely retrieved from the anterior presacral space via this posterior approach. Scalloped vertebral bodies were forming the ventral wall of the postoperative cavity following tumor excision. Microscopic examination revealed cells showing elongated nuclei, arranged in spindles and fascicles. Tumor lacked atypia or mitosis. The histological picture was characteristic of neurofibroma. The patient made uneventful recovery and is doing well at 8 months follow up. Postoperative imaging has been deferred due to financial constraints.
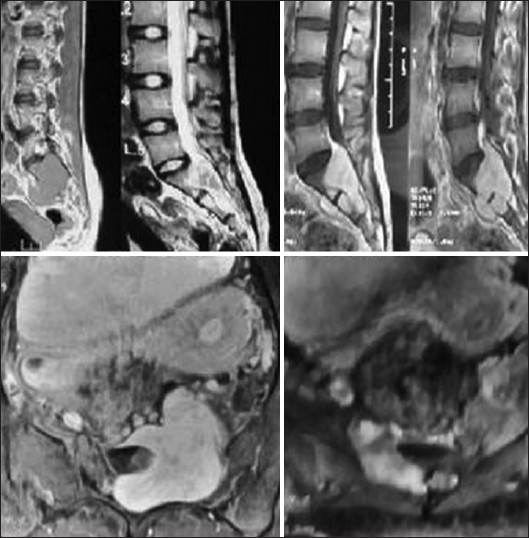
- MRI showing the lesion on sagittal plain and contrast images. There was “lateral” anterior extension of the tumor. The contrast axial sections reveal giant left and small right sided bilateral neurofibromas of S1 root encroaching the foramina
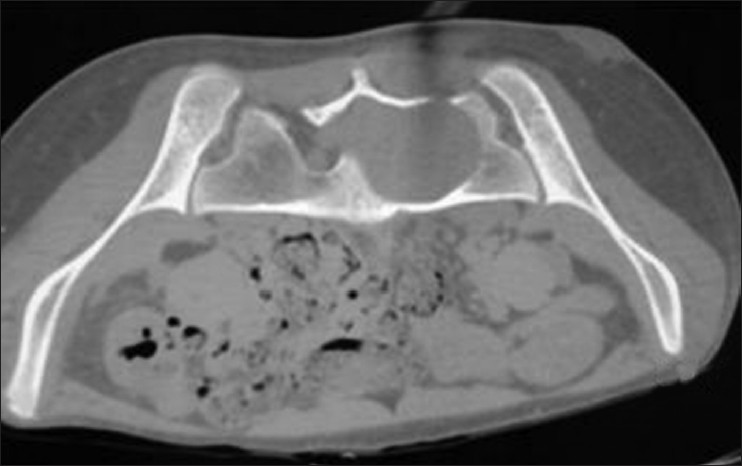
- CT bone window showing extensive scalloping of bone with papery thin lamina
Discussion
Intraspinal neurofibromas occur in approximately 2% of patients with NF1. The tumors arise generally from the dorsal roots in the cervical and lumbar regions of the spine, and can cause radicular symptoms, the most common of which is pain. Most of those lesions are intracanalicular and intraforaminal and demonstrate extension into the spinal canal with growth. Over time, enlargement of the spinal canal and widening of the interpedicular distance can occur, resulting in instability and scoliosis. Sacral neurofibromas are still uncommon and they manifest late until they acquire large proportions in size due to their slow growth. Klimo et al. have classified sacral neurofibromas into three categories.[1] Type I are limited to the sacrum only. Type II originate within sacrum but extend through the intervertebral foramina into the presacral space. Type III are the ones which are essentially in the presacral space only. The authors advocate posterior, anterior-posterior, and only anterior approaches, respectively, for Type I, II, and III subtypes. Ours was Type II sacral neurofibroma which was tackled only by posterior approach owing to the space provided by the expansion of the tumor. They may have varied clinical presentations although pain is the most common symptom, which is often radicular in nature.[2] They can also present with motor weakness, saddle anesthesia, and/or sphincteric disturbances, although this was not seen in our patient. MRI and CT of pelvis demonstrate the expansion of the bones due to the tumor and help in surgical planning.[3] They may not present with the typical imaging features of neurofibromas and nerve root may not be separately visualized in giant ones.[4] If the corridor has been widened by the lesion itself, almost complete tumor can be retrieved by posterior approach. Previously, Abernathy et al. had operated ten such patients by posterior approach and provided gross total removal in four patients.[5] Similarly, Dominguez et al. have operated upon six patients of giant sacral neural sheath tumors, with four requiring posterior and two requiring anterior approach.[6] More importantly, during surgery, giant neurofibromas do not demonstrate separate nerve fascicles, as seen in smaller tumors. The nerve fascicles are completely replaced by a mass which can be excised completely. Similar experience was observed by Rieckman et al. when there sectioned L2 nerve root for complete excision of a nerve sheath tumor.[7] Also, Levy et al. hypothesized that the affected nerve root in neurofibromas does not have any function left usually.[8] This may be due to functional compensation by epispinal axons or overlapping innervation.[9] However, they also opined that eloquent roots like L5 or S1 may be difficult to section after all.[8] On the other hand, Ahmed et al. in a study of sacral tumors have found that usually fusion is not required for instability in sacral tumors and only when more than 50% of sacroiliac joints were involved, they had to fuse two of their patients of sacral tumors with modified Galveston technique.[10] Our case was typical in two ways. Surgical excision of bilateral S1 neurofibromas in a patient of NF1 was possible by using posterior approach only (although type II). And, patient did not experience any neurological deficit after sectioning an eloquent S1 root. Hence, especially in giant neurofibromas, if intact fascicles are not observed during surgery, one should attempt a complete excision and minimize the chances of recurrence in future.
Excision of giant sacral neurofibromas may not result in grave deficits always if the patient is neurologically intact before surgery. Also, in selected patients, only posterior approach may suffice for giant neurofibromas with extensive bone scalloping and complete removal can be attempted successfully despite narrow corridors.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Nerve sheath tumors involving the sacrum: Case report and classification scheme. Neurosurg Focus. 2003;15:E12.
- [Google Scholar]
- MR imaging of spinal tumors in children with neurofibromatosis 1. AJR Am J Roentgenol. 2003;180:413-7.
- [Google Scholar]
- MR imaging features of giant pre-sacral schwannomas: A report of four cases. Eur Radiol. 2002;12:2365-9.
- [Google Scholar]
- Giant intrasacral schwannomas: Report of six cases. Acta Neurochir (Wien). 1997;139:954-60.
- [Google Scholar]
- Giant plexiform neurofibromas: An intraspinal dumbbell tumour with a huge retroperitoneal portion. Arch Neurocien (Mex). 2006;11:18-21.
- [Google Scholar]
- Spinal neurofibromas: A report of 66 cases and a comparision with meningiomas. Neurosurgery. 1986;18:331-4.
- [Google Scholar]
- Lumbosacral intersegmental epispinal axons and ectopic ventral nerve rootlets. J Neurosurg. 1987;67:269-77.
- [Google Scholar]
- Sacral tumours: Postoperative clinical and radiological outcomes. Pan arab J Neurosurg. 2011;15:42-5.
- [Google Scholar]






