Translate this page into:
Pneumocephalus in cerebellopontine angle and meningitis secondary to chronic otitis media in a child
Address for correspondence: Dr. Shailendra Ratre, Department of Neurosurgery, Netaji Subhash Chandra Bose Medical College, Jabalpur, Madhya Pradesh, India. E-mail: drsratre@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pneumocephalus is a rare complication of chronic otitis media. Despite its rarity intra-cranial air carries a potential risk of increased intra-cranial pressure or meningitis, which requires immediate therapy. A 10-year-old child presented to us with complaints of fever, headache, vomiting, and decreased hearing from left ear. He had history of left ear discharge since 2 years. Clinical examination revealed neck rigidity and left chronic otitis media. Contrast enhanced computed axial tomography scan of head [Figures 1 and 2] showed pneumocephalus in left cerebellopontine angle, opacification of left middle ear and nonpneumatisation of left mastoid. Child was immediately put on empirical intravenous antibiotics and decongestants. He showed clinical improvement in 3 days. Pneumocephalus secondary to chronic otitis media is extremely rare; we are reporting one such case in a child with review of literature.
Keywords
Meningitis
neurogenic complications
otitis media
pneumocephalus
Introduction
Otogenic infections rarely cause pneumocephalus. In 1884, Chiari reported the first case of pneumocephalus on an autopsy done in patient of ethmoiditis.[1] In 1926 Dandy reported the first case of otogenic pneumocephalus.[1] Review of literature by Andrew and Canalis.[1] revealed head trauma as the leading cause of otogenic pneumocephalus (36%). Other causes were otogenic infections (30%), mastoid surgeries (30%) and idiopathic (3%). The middle ear diseases lead to intra-cranial complications in 0.5–4% of cases.[23] Of these intra-cranial complications, pneumocephalus is very rare. Pneumocephalus secondary to chronic otitis media in a child is very rarely reported and ours is probably the first case in children below 12 years. We are reporting one such case with interesting imaging finding.
Case Report
Clinical presentation
A 10-year-old child was admitted in our hospital with chief complaints of left ear discharge and earache since 8 days; fever and headache since 5 days. He had history of left ear discharge 2 years back. On examination, he was febrile, neck rigidity was present. He was fully conscious and oriented. There was purulent discharge from left ear. Otological examination revealed pus discharge from 2 to 6 O’clock position of left tympanic membrane and a reddish polypoid mass at 6–10 O’clock position. Mastoid tenderness and conductive deafness was present on left side.
Investigations
Routine laboratory investigations were normal. Cerebrospinal fluid (CSF) examination was suggestive of pyogenic meningitis. CSF culture was sterile. Ear swab culture yielded heavy growth of Staphylococcus aureus. Contrast enhanced computed tomography (CECT) head [Figures 1 and 2] revealed pneumocehalus in left cerebellopontine angle with mild compression at brainstem. There was opacification of left middle ear and nonpneumatisation of left mastoid. Interestingly the air pockets showed there path of entry from middle ear through Trautman's triangle/sinodural angle.
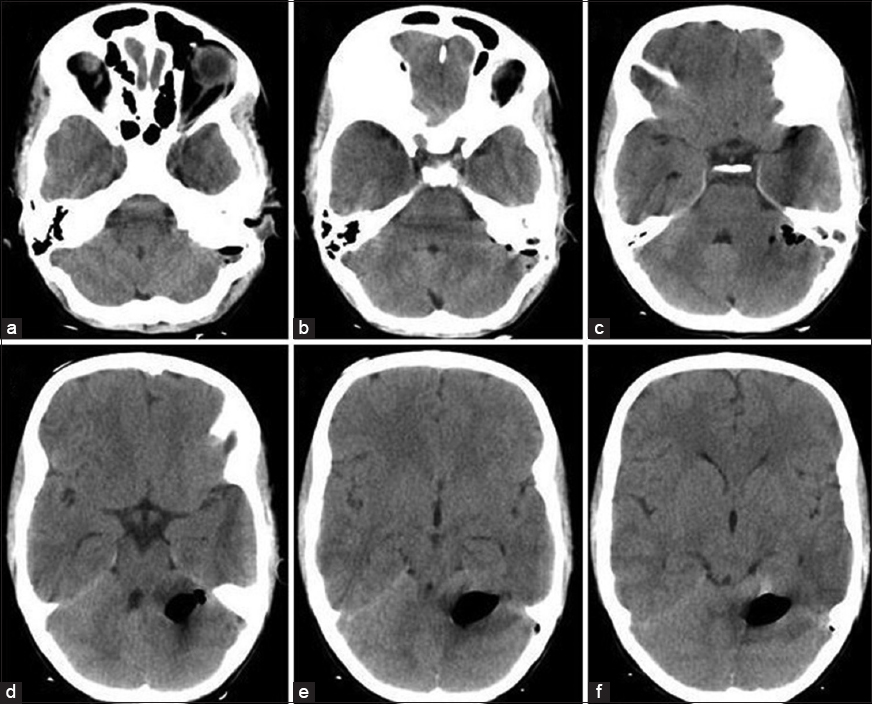
- (a-f) Computed tomography head plain axial cuts showing pneumocephalus in left cerebellopontine angle with mild effacement of fourth ventricle. Small air pockets showing the site of entry from sinodural angle
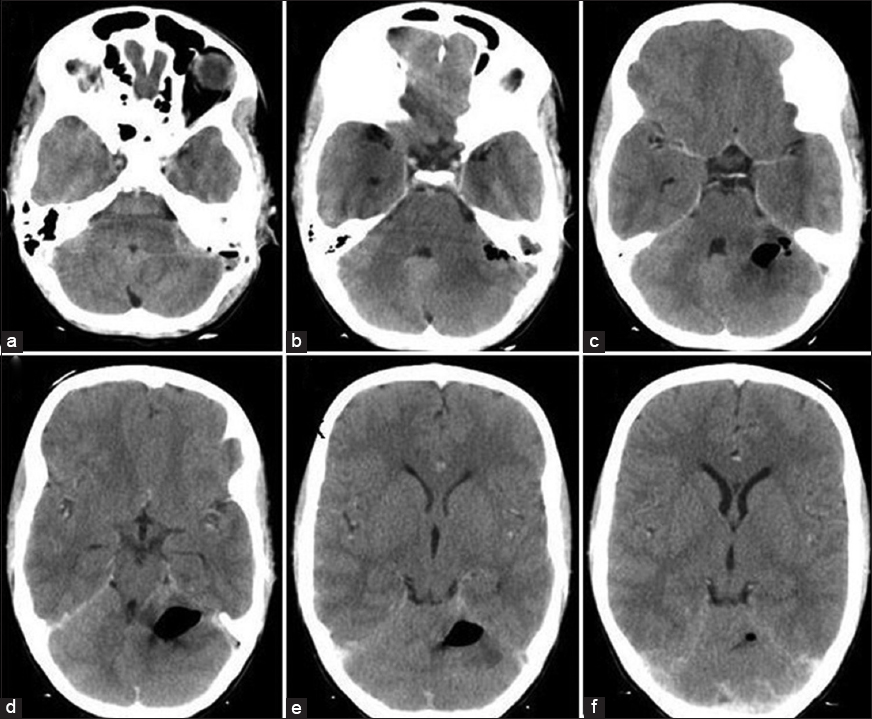
- (a-f) Contrast enhanced computed tomography head axial cuts to rule out any abscess
Management
Child was immediately started on emperical intravenous (i.v.) antibiotics-pipracillin/tazobactum, amikacin and metrogyl with decongestants. Child improved clinically in terms of control of fever and headache in 3 days. Repeat CECT brain was planned but patient left hospital against medical advice.
Discussion
Pneumocephalus implies air inside the cranial vault, which usually results from cranio-facial trauma. It may be as a result of erosion of the skull due to neoplasm or infection, neurosurgical procedures or fistulous tract formation.[4] Spontaneous pneumocephalus is currently a rare manifestation of chronic otitis media.
The reported rate of intra-cranial complications related to middle ear diseases ranges from 0.5% to 4%.[23] Review of literature of last 35 years yielded only 21 cases of pneumocephalus secondary to chronic otitis media.[145678] and this is probably the first case in children below 12 years of age.
The physio-pathologic mechanism that can explain the genesis of pneumocephalus is a break between the middle ear and either middle or posterior cranial fossa, which allows air to enter. In addition, an increase in middle ear pressure over the intra-cranial pressure must be present to permit air to enter the cranium. This may be explained by two mechanisms:
-
Ball valve effect: The intra-cranial contents may act as a ball valve allowing air to enter through a fistula[9] especially during sneezing or coughing
-
Inverted bottle effect: When a CSF leak is present; a negative intra-cranial pressure is built up, leading to the replacement of fluid with air.[9]
In our patient, the imaging suggests leak of air between the middle ear and posterior cranial fossa.
In the clinical picture of otogenic pneumocephalus and meningitis, headache is one of the earliest symptoms, together with fever. Vomiting may be present, as well as agitation and irritability. Rigor nucalis is another early sign, as well.
As lethargy and poor oral intake. Signs of increased endocrinal pressure can also include papilledema and cranial nerve palsies.[3] Otologic symptoms are frequently present, and may include otorrhea, postauricular edema and otalgia.
Management depends on the degree of tension, symptomatology, and the underlying cause. When associated with trauma or surgery, bed rest and close monitoring may suffice, although needle aspiration or re-exploration may be needed. When secondary to otitis media or a congenital defect, control of any infection and repair of the defect are mandatory. Once the defect is identified and has been located, cartilage, free fascia, or temporalis muscle-fascia flap are best used to plug the site, depending on its size.[1]
Recommendations for the management of otogenic meningitis with pneumocephalus include a third-generation cephalosporin, either i.v. cefotaxime (75 mg/kg every 6 h) or ceftriaxone (50 mg/kg every 6 h), and vancomycin (15 mg/kg every 6 h). The need to add vancomycin to the therapeutic regimen is a consequence of the escalating prevalence of strains of germs resistant to penicillin and cephalosporins. Adding rifampin (20 mg/kg as a single daily dose, i.v.) or meropenem (40 mg/kg every 8 h) may be taken into consideration.[210] The usefulness of adding dexamethasone to the therapeutic regimen has been controversial; patients receiving steroids have been shown to have a 50% reduction of neurological sequelae, without improvement regarding the audiological outcome.[10]
We were not able to do complete management in this case as a child left the hospital. We are still reporting the case because otogenic pneumocephalus is very rare especially in children, it needs immediate therapy to prevent complications and this case has interesting imaging findings.
Conclusion
Pneumocephalus is a very rare complication of chronic otitis media, especially in children. In spite of its rarity, the diagnosis must be considered when a patient has neurologic complaints and chronic otitis media. Immediate therapy is required as it carries a potential risk of increased intra-cranial pressure or meningitis. Although neurosurgical complications of chronic otitis media need priority management, we stresses the need of treatment of ear disease in same admission period of the patient to prevent further complications.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Intracranial complications of otitis media: 15 years of experience in 33 patients. Otolaryngol Head Neck Surg. 2005;132:37-42.
- [Google Scholar]
- Management of elevated intracranial pressure in patients with Cryptococcal meningitis. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:137-42.
- [Google Scholar]
- Spontaneous otogenic pneumocephalus. Case report and review of the literature. J Neurosurg. 1998;89:1036-9.
- [Google Scholar]
- Otogenic pneumocephalus secondary to chronic otitis media. Arch Otolaryngol. 1980;106:437-9.
- [Google Scholar]
- Pneumocephalus presenting as a complication of chronic otitis media - A case report. Indian J Otolaryngol Head Neck Surg. 2008;60:390-2.
- [Google Scholar]
- Pneumocephalus at the cerebellopontine angle secondary to chronic otitis media. Clin Neurol Neurosurg. 1990;92:155-7.
- [Google Scholar]
- A case of pneumocephalus and meningitis as a complication of silent otitis media. Ear Nose Throat J. 2004;83:50-2.
- [Google Scholar]






