Translate this page into:
Pitching for the hitch: Neodural tenting sutures to prevent post-cranioplasty collection in a sunken craniectomy site
*Corresponding author: Prasad Krishnan, Department of Neurosurgery, National Neurosciences Centre, Kolkata, West Bengal, India. prasad.krishnan@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Krishnan P, Maurya VP. Pitching for the hitch: Neodural tenting sutures to prevent post-cranioplasty collection in a sunken craniectomy site. J Neurosci Rural Pract. 2024;15:410-3. doi: 10.25259/JNRP_43_2024
Abstract
Post-operative epidural collection is a commonly encountered complication following cranioplasty (CP) in a patient with a sunken skin flap. While on most occasions, the collection is small and resolves spontaneously, on occasion, it may be large enough to warrant evacuation. Further, such collections may predispose to infection and bone flap resorption. Dural hitch sutures were once used routinely in all craniotomies by tacking up the dura at the margins of the craniotomy to the surrounding pericranium to prevent post-operative epidural collection but now several surgeons use them only when deemed absolutely necessary. We describe a variation (in cases where CP is performed in patients with a sunken flap) where several sutures are passed from the neodura through the center of the bone flap (as opposed to the peripherally placed conventional hitch sutures) to obviate the dead space and prevent any post-operative collection.
Keywords
Cranioplasty
Neodura
Hitch sutures
Tenting sutures
Decompressive craniectomy
Sunken skin flap
INTRODUCTION
Interval cranioplasty (CP) is a commonly performed operation in patients, who have had a decompressive craniectomy (DC) once the raised intracranial pressure has subsided.[1] One of the well-recognized complications of this procedure is an epidural collection below the replaced bone flap.[1] This complication is more common in patients, who have a sunken skin flap at the DC site, as there is often a significant space between the neodura covering the brain and the repositioned bone.[1] We had encountered these complications previously and now advocate placement of multiple central neodural hitch sutures through holes drilled in the CP flap and tied above the bone to eliminate this dead space.
TECHNIQUE
During CP in a patient with a sunken skin flap, after lifting the skin and galea off the neodura and defining the margins of the craniectomy defect, a few hitch sutures are taken through the neodura (at approximately the central part of the defect) with 3-0 absorbable braided polyglactin 910 sutures on a round-bodied needle. These needles are typically halfcircle and measure about 15 mm from tip to swage point (the point where the thread attaches to the needle). Care is taken to pass the needle superficially only so as not to damage the underlying brain or any vein. The flap that is to be replaced is then held a few centimeters over the defect. Visual estimations of points where the threads would come out (if they were to be drawn perpendicularly outward through a seated flap) are performed separately by both the operating surgeon and his assistant and are marked on the bone with monopolar cautery or using a sterile pen. If they are in concordance then corresponding pairs of holes are drilled in the bone flap that is to be replaced. This process is repeated for as many central neodural hitches that have been taken. Then, the threads are brought outside through the corresponding holes meant for them in the flap. Finally, after the flap is firmly fixed to the margins of the defect, these hitch sutures are tied over the flap [Figure 1] to lift the dura upward and eliminate dead space. The galea and skin are closed over a closed suction drain.
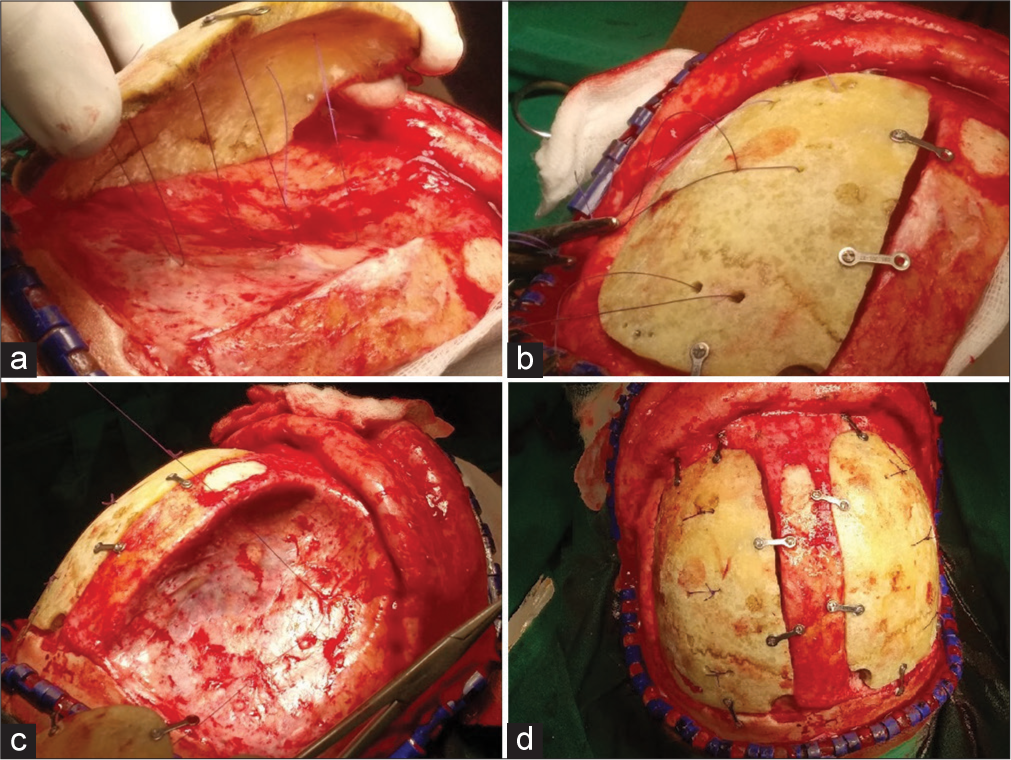
- Operative photographs in a case of bilateral frontal decompressive craniotomy showing (a) neodural tenting sutures after being passed through the bone flap to be replaced; (b) superior view of the bone flap with pairs of holes through, which the tenting sutures are coming out. Miniplates have been fixed on the bone flap but not yet affixed to the craniotomy margins; (c) dural tenting sutures are being taken on the contralateral side and (d) the final image after the flaps have been fixed, and the central hitch sutures have been tied over them.
DISCUSSION
Dural hitch (tenting) sutures were introduced by Walter Dandy by suturing dura at the margins of the craniotomy to adjacent pericranium to prevent post-operative epidural hemorrhage in an era where this complication occurred in up to 25% of intracranial surgeries.[2] Once considered an “ubiquitous and unquestioned neurosurgical routine,”[2] they have since become redundant as a routine prophylactic measure and are now used only when deemed necessary,[2] and several studies have questioned the utility of routinely tacking up the dural margins to prevent a post-operative hemorrhage.[3,4]
Post-operative collection below a CP flap (either as an epidural hemorrhage or an epidural fluid collection) is an undesirable event, as it may predispose to infection and delayed flap resorption[5] or on occasion even may cause a significant mass effect that needs resurgery.[5] We have encountered these collections in patients with a sunken skin flap where central neodural tenting sutures were not used [Figure 2], but in contrast, we have found that the post-operative computed tomography scan is invariably satisfactory when this technique is employed [Figure 3]. Further, we feel that (besides eliminating dead space by lifting up the neodura) another utility of this procedure is that the multiple holes drilled in the CP flap may help in the egress of any epidural collection to the subgaleal space from where they can be removed by the closed suction drain.
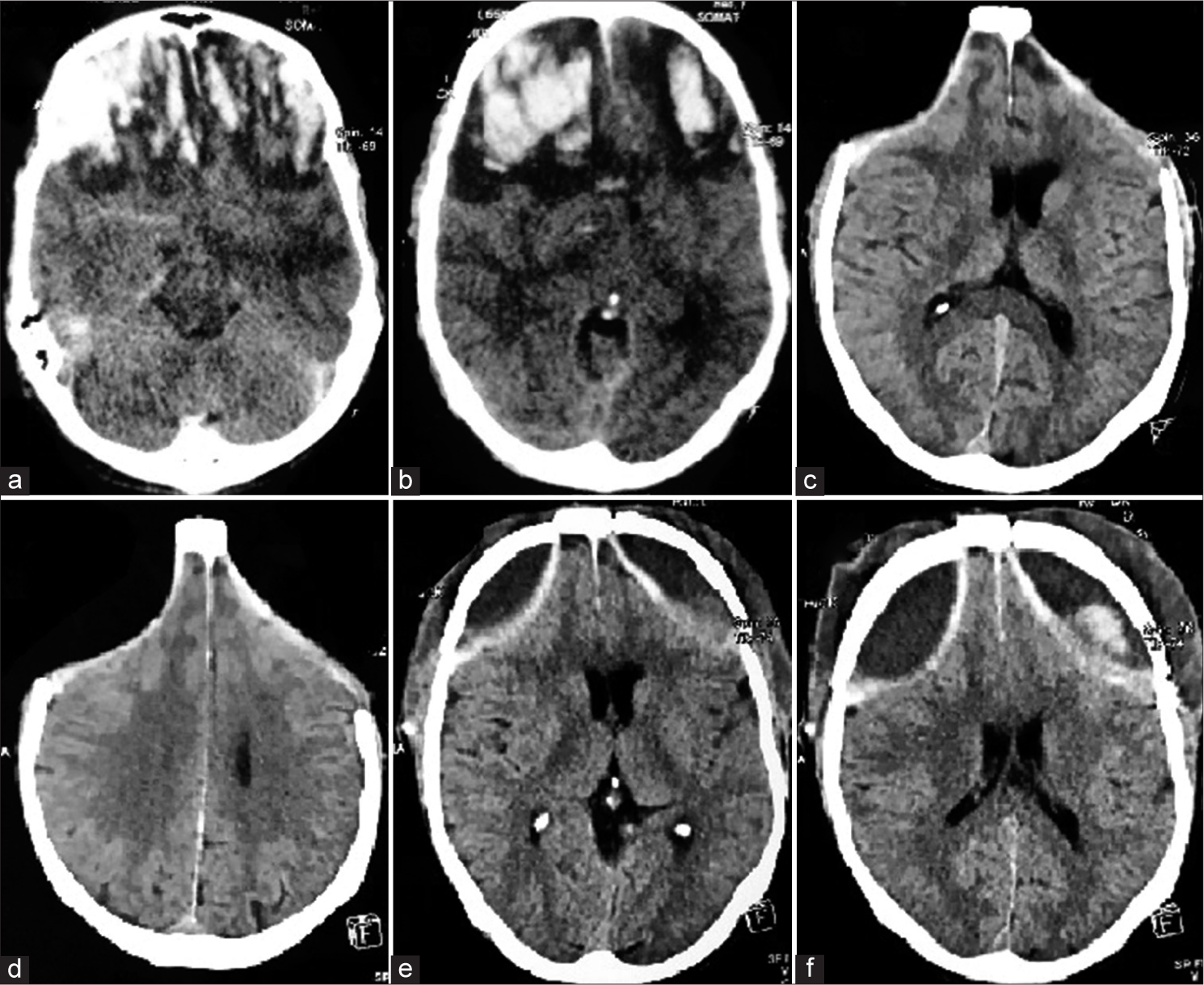
- (a and b) Axial computed tomography (CT) scan images of a patient with bifrontal contusions showing effaced cisterns and ventricles with significant perilesional edema, who subsequently underwent bilateral decompressive craniectomy. (c and d) Axial CT images show that precranioplasty the scalp flap was sunken bilaterally. In this patient, no neodural hitch sutures had been placed, and (e and f) axial CT images done on the morning after surgery show a significant post-operative collection below the replaced flap on both sides.

- (a and b) Axial computed tomography (CT) scan images of a patient with bifrontal contusions and bilateral acute subdural hematomas showing effaced cisterns and chinked ventricles. The patient underwent bilateral decompressive craniectomy, and (c and d) pre-cranioplasty axial CT images show that the scalp flap was sunken bilaterally. In this patient, central neodural hitch sutures had been placed while replacing the bone flap, and (e and f) axial CT images done on the morning after surgery show good brain expansion with no post-operative collection on either side below the replaced flap.
CONCLUSION
This variation of the hitch suture (passing through the bone flap and tied on the top of the same) serves the same purpose as the time-honored sutures placed from the dura at the margins of the craniotomy to the surrounding pericranium and is a useful tool to prevent a post-operative epidural collection following CP when performed in a patient with a sunken skin flap.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidural fluid collections after cranioplasty. Neurol India. 2022;70:1629-34.
- [CrossRef] [PubMed] [Google Scholar]
- The hitch stitch: An obsolete neurosurgical technique? Br J Neurosurg. 2002;16:541-4.
- [CrossRef] [PubMed] [Google Scholar]
- Is dural hitching necessary to prevent postoperative extradural haemorrhage in craniotomies and craniectomies. Sri Lanka J Surg. 2016;34:11-7.
- [CrossRef] [Google Scholar]
- Complications after cranioplasty: A pictorial narrative with techniques to manage and avoid the same. Indian J Neurotrauma. 2023;20:124-32.
- [CrossRef] [Google Scholar]







