Translate this page into:
Percutaneous unilateral vertebro-stentoplasty for painful osteoporotic compression fracture of lumbar vertebra
*Corresponding author: Manish Vaish, Department of Neuroscience, Max Superspeciality Hospital, Vaishali, Uttar Pradesh, India. drmanishvaish@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Karki M, Rajpal G, Bundela YS, Vaish M. Percutaneous unilateral vertebro-stentoplasty for painful osteoporotic compression fracture of lumbar vertebra. J Neurosci Rural Pract. 2024;15:507-9. doi: 10.25259/JNRP_166_2024
Abstract
Osteoporosis is one of the common diseases in the elderly population which can cause compression fracture of the vertebral body due to loss of microarchitecture, loss of density, and deterioration of bone tissue leading to chronic pain, kyphotic deformity of the vertebra, and neurological complications. We report the case of a 68-year-old female, who presented to us with severe midback region pain for one year, which was increased over two months along with numbness in the right leg and difficulty in walking. The radiological investigation and magnetic resonance imaging spine revealed chronic compression fracture with the reduction in height of the L1 vertebra, which is seen with anterior wedging. The patient underwent vertebro-stentoplasty (VS) with bone cement, polymethyl-methacrylate. The patient was discharged well on third day of surgery. The VS for compression fracture of the lumbar vertebra demonstrated better results with improvement in pain and radiological finding in our patient.
Keywords
Back pain
Compression fracture
Lumbar vertebra
Osteoporosis
Stentoplasty
INTRODUCTION
Vertebral compression fractures (VCFs) are one of the most commonly encountered osteoporotic fractures in the world[1] and account for approximately 20% of individuals older than 70 years of age and 16 % of postmenopausal women.[2] Most VCFs may result in severe back pain, impairment in mobility, and impaired quality of life by decreasing in height, as well as kyphotic deformity of the vertebral body.[3] The main purpose of treatment of VCFs is to reduce pain, improve functional ability, and decrease the risk of vertebral fracture in the future. However, vertebroplasty (VP) and balloon kyphoplasty (BK) are well set up with minimally invasive treatment strategies for VCFs in osteoporotic patients, incomplete fracture reduction or reduction in vertebral height after deflation of balloon tamp or withdrawal of balloon before cement filling have been reported.[4] To overcome it, vertebro-stentoplasty (VS) has evolved using an expandable stent and has demonstrated satisfactory results by restoring vertebral height after balloon withdrawal.[5] There is limited study about treatment with VS for lumbar vertebra compression fracture. The purpose of this case report was to evaluate the safety and efficacy of VS for the treatment of VCF in our patient.
CASE REPORT
A 68-year-old female was admitted to the neurosurgery department with chief complaints of midback pain for one year, which increased since two months associated with right leg numbness and difficulty in walking. The patient had a history of psychiatric disorder and hypertension under medication. A physical examination was done. The power of upper limbs was 5/5 and lower limbs was 4/5. The straight leg raise test for the right leg was 30 and the left leg 60 with no extensor hallucis longus weakness and bilateral plantar flexor response. The visual analog scale for pain was 8/10. Magnetic resonance imaging spine was done for further investigation which revealed mild disc bulge in D12-L1 and L1-L2 with L1 chronic compression fracture with the reduction in height of L1 vertebra with anterior wedging (kyphotic deformity) [Figure 1a]. The patient was under conservative treatment from another hospital since one year, but no improvement was observed. Therefore, we decided to treat her with a new minimally invasive VS procedure. The procedure was performed in a prone position under general anesthesia. The unilateral transpedicular intraosseous route was enforced under a percutaneous approach and fluoroscopy assistance to the desired location within the vertebral body, by sequential use of Jamshidi needle, guide wire, access cannula, obtaining intraosseous tunnel from the pedicle of the vertebral body. A kyphoplasty balloon surrounded by a stent (JHONSON and JHONSON) was applied through the unilateral tunnel of the pedicle and inflated in a controlled manner. The balloon was removed after deflated, and the expanded stent remained in the vertebral body [Figures 1b and c]. At last bone cement, polymethyl-methacrylate (PMMA) was filled inside the stent [Figures 1d and e]. Post-surgical condition of the patient went uneventful. She was discharged on 3rd day of the procedure. The visual analog score was 5/10 during discharge and 0.5/10 at the first month of the follow-up period, and an x-ray of the D-L spine was done [Figure 1f].
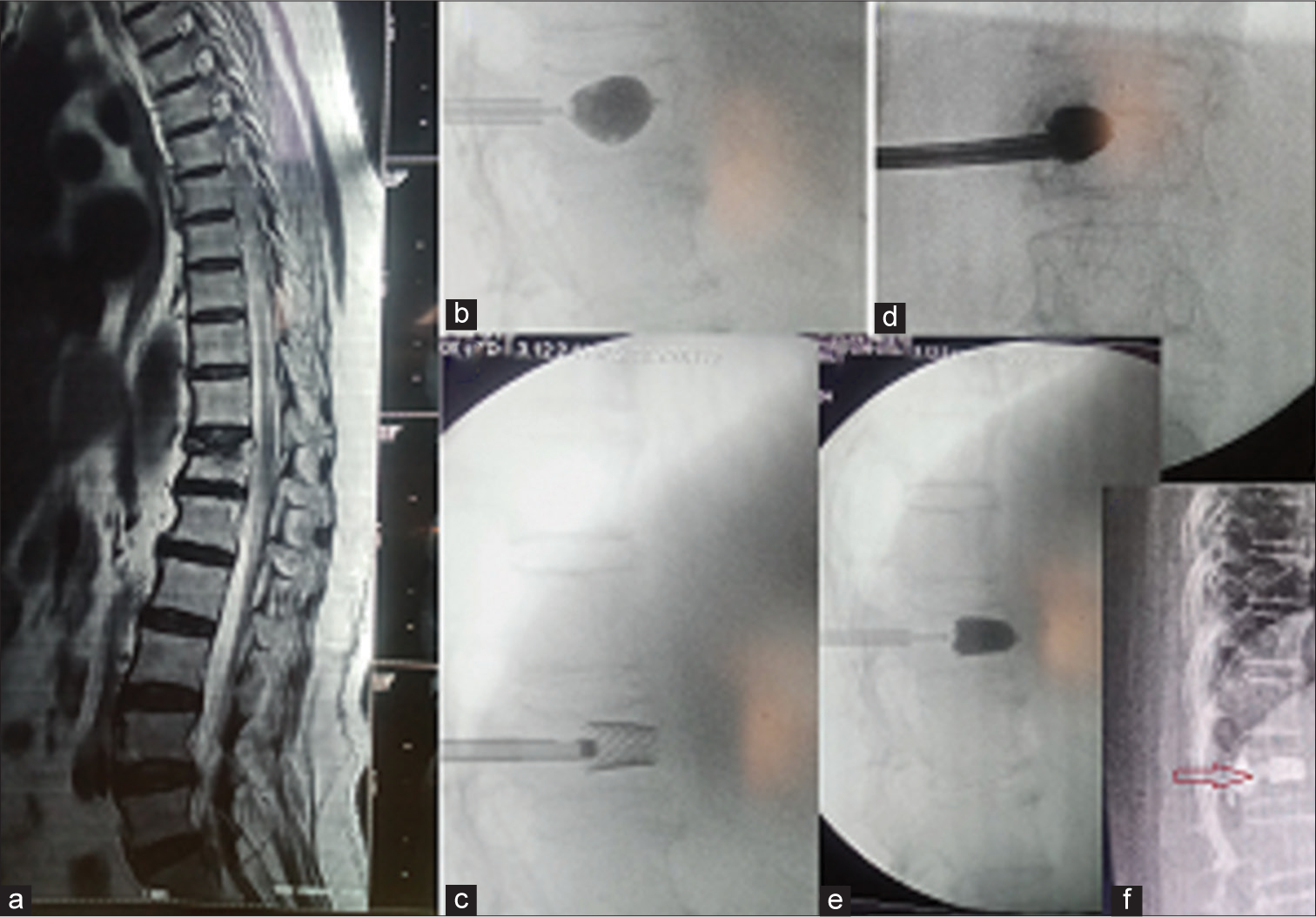
- (a) Lateral view of D-L spine magnetic resonance imaging showing compression fracture of L1 vertebra with anterior wedging, (b and c) lateral fluoroscopy images showing inflation of balloon and placement of stent after withdrawal of balloon with restoration height of L1 vertebral body, (d and e) anterior and lateral view of fluoroscopy images showing filling of bone cement, and (f) postoperative follow-up images showing stent in situ (arrow) with restored height of L1 vertebral body.
DISCUSSION
Osteoporosis is a common disease in the old-age population and a major health concern in the world, which may result in the impairment of strength and a relatively increased risk of spontaneous vertebral fracture due to loss micro-architecture, loss of density, and deterioration of bone tissue.[6] Severe back pain, kyphotic deformity, compromised respiration, and deterioration of quality of life with prolonged immobility periods and risk of vertebral collapse and neurological injury can be provoked by VCFs.[7] Reduction in pain, improvement in functional ability, and decreased risk of fracture are the major targets in the management of VCFs. Ordinarily, VCFs are managed conservatively with complete bed rest, analgesic medications, and a back brace.[8] In our case, the patient was under conservative treatment since one year, but we did not find any symptomatic improvement in back pain. Hence, early surgical interventions are necessary to stabilize the spine for those symptomatic patients who are older with impaired quality of life.[9]
With the revolutionization in new surgical techniques for VCF’s management, vertebroplasty was developed, which was mentioned by Galibert et al. in 1987.[10] Thereafter, VP has been broadly applied to treat VCFs caused by osteoporosis or malignancy, where injection of bone cement (such as PMMA) is used to fill in the vertebral body to restore height and eradicate pain. Despite that, bone cement leakage from the fractured vertebral body is one of the most commonly encountered problems, which may cause radiculopathy, paralysis, and even death.[11,12] To solve these procedural complications, BK was outlined by Tutton et al. in 2015, who explained balloon inflation by inserting through a percutaneous transpedicular approach to the vertebral body and injection of bone cement in the cavity made by balloon inflation after balloon withdrawal to adjust the height of the fractured vertebral body and kyphotic deformity.[13] However, correct restoration in height of the compressed vertebral body is not maintained by the BK technique; further, a minimally invasive technique was researched and evolved vertebral body stenting, also termed VS.[14] The principle of stentoplasty includes the placement of a stent in the fractured vertebral body after the inflation of the balloon surrounded by the stent and the injection of bone cement in the cavity surrounded by the stent after the withdrawal of the deflated balloon. The stent helps restoration of height after the removal of the balloon before injection of bone in contrast to BK. Decreased in the restored height of the compressed vertebral body, leakage of cement causing radiculopathy, spinal cord compression, pulmonary embolism, fat embolism, and wound infection were not noted in our case, similar to the result of another study.[15] The patient was noticed pain free completely at the first month follow-up period after the procedure. Our case report has some limitations. It is retrospective, and the number of cases are not enough because it is a case report and does not have long-term follow-up reports to evaluate the efficacy of this new novel technique for the management of compression vertebral fracture.
CONCLUSION
The VS is a safe and effective minimally invasive procedure to reduce pain, reduce disability, and improve quality of life by eliminating kyphotic deformity in osteoporotic compression fracture of the lumbar vertebra. However, the study of larger numbers of cases with longer follow-up period is needed to be done to validate the effectiveness of this new minimal invasive stentoplasty for compression fracture of vertebrae.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Osteoporotic thoracolumbar vertebral compression fractures: Clinical manifestations and treatment 2014. UpToDate
- [Google Scholar]
- The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone. 1995;17:505S-11.
- [CrossRef] [PubMed] [Google Scholar]
- An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726-33.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus. 2005;18:e5.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of the vertebral body stenting system for the restoration of vertebral height in acute traumatic compression fractures in a non-osteoporotic population. Cardiovasc Intervent Radiol. 2019;42:1579-87.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal aging and osteoporosis: Mechanisms and therapeutics. Int J Mol Sci. 2021;22:3553.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral fragility fractures (VFF)-Who, when and how to operate. Injury. 2018;49:1430-5.
- [CrossRef] [PubMed] [Google Scholar]
- Upper cervical spine injuries: Indications and limits of the conservative management in Halo vest. A systematic review of efficacy and safety. Injury. 2010;41:1127-35.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: Evaluation after 36 months. J Bone Joint Surg Br. 2009;91:379-84.
- [CrossRef] [PubMed] [Google Scholar]
- Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33:166-8.
- [Google Scholar]
- Risk factors for bone cement leakage in percutaneous vertebroplasty: A retrospective study of four hundred and eighty five patients. Int Orthop. 2016;40:1205-10.
- [CrossRef] [PubMed] [Google Scholar]
- Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine (Phila Pa (1976). 2004;29:E294-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Kiva system as a vertebral augmentation treatment-a safety and effectiveness trial: A randomized, noninferiority trial comparing the Kiva system with balloon kyphoplasty in treatment of osteoporotic vertebral compression fractures. Spine (Phila Pa (1976). 2015;40:865-75.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral body stenting: A new method for vertebral augmentation versus kyphoplasty. Eur Spine J. 2010;19:916-23.
- [CrossRef] [PubMed] [Google Scholar]
- Stentoplasty with resorbable calcium salt bone void fillers for the treatment of vertebral compression fracture: Evaluation after 3 years. Clin Interv Aging. 2021;16:843-52.
- [CrossRef] [PubMed] [Google Scholar]






