Translate this page into:
Penetrating head injury from angle grinder: A cautionary tale
Address for correspondence: Dr. S. Senthil Kumaran, Department of Accident, Emergency & Critical Care Medicine, Sri Gokulam hospital& Research institute, Salem, Tamil Nadu, India. E-mail: maniansenthil@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Penetrating cranial injury is a potentially life-threatening condition. Injuries resulting from the use of angle grinders are numerous and cause high-velocity penetrating cranial injuries. We present a series of two penetrating head injuries associated with improper use of angle grinder, which resulted in shattering of disc into high velocity missiles with reference to management and prevention. One of those hit on the forehead of the operator and the other on the occipital region of the co-worker at a distance of five meters. The pathophysiological consequence of penetrating head injuries depends on the kinetic energy and trajectory of the object. In the nearby healthcare center the impacted broken disc was removed without realising the consequences and the wound was packed. As the conscious level declined in both, they were referred. CT brain revealed fracture in skull and changes in the brain in both. Expeditious removal of the penetrating foreign body and focal debridement of the scalp, skull, dura, and involved parenchyma and Watertight dural closure were carried out. The most important thing is not to remove the impacted foreign body at the site of accident. Craniectomy around the foreign body, debridement and removal of foreign body without zigzag motion are needed. Removal should be done following original direction of projectile injury. The neurological sequelae following the non missile penetrating head injuries are determined by the severity and location of initial injury as well as the rapidity of the exploration and fastidious debridement.
Keywords
Angle grinder
Occupational accident
penetrating head injury
traumatic brain injury
Introduction
Occupational accident is an unexpected and unplanned one, and causes injuries in one or more workers. Angle grinders[1] are one of the most dangerous tools used around the world to cut stone, metal and concrete. Penetrating head injury from angle grinders is increasingly recognized due to their frequent use in the work place and at home. A series of two penetrating head injuries associated with angle grinder use are presented, as these are rarely reported in Indian literature.
Case Reports
Two construction workers were brought to the emergency room in an altered sensorium after an accident at their construction site. The history revealed that the first patient was cutting stone with an angle grinder without protective guard. The disc in the grinder shattered into four high velocity non missiles. Two busted disc embedded in the ceiling, the third hit on his fore head and the fourth hit in the occipital region of his co-worker, who was working at five meters away. Following the blow on his head from behind, the second case had a fall from a height of four meters. Both the patients were immediately shifted to a nearby healthcare center, where the impacted broken disc was removed and the wound was packed. As there was an increased amount of bleeding from the wound site and declining level of consciousness, both the patients were referred for further management.
Case 1
A 35-year-old right-handed healthy male, without any significant past medical history, was brought to the emergency room following the above said mishap. On examination he was hemodynamically stable and maintaining adequate saturation in room air. He was also drowsy and responding to deep painful stimuli with a Glasgow coma scale score of 10. Both pupils were equally reacting to light. There was no focal or lateralizing neurological deficit or evidence of seizure episode.
There was a lacerated wound of 11 X 4 cms over the forehead with tissue loss [Figure 1]. The wound was grossly contaminated with sand, mud and burnt cloth pieces with tobacco which was used for haemostatic purpose in folk medicine. There was no active bleed from the wound site. After an initial assessment, the wound was irrigated with normal saline.

- Clinical photograph showing lacerated wound in the fore head
The trauma series X-rays were normal and focused abdominal sonogram for trauma (FAST) was negative. A non enhanced computerized tomography (CT) serial axial section of 5 mm thickness of the skull revealed bilateral frontal and ethmoid comminuted depressed fracture. There was bilateral anterio inferior frontal lobe hemorrhagic contusion with focal cerebral edema. The subarachnoid pneumocephalus and hemosinus of frontal and ethmoid were also noted [Figures 2 and 3]. The ventricular system and the posterior fossa were normal with no midline shift.
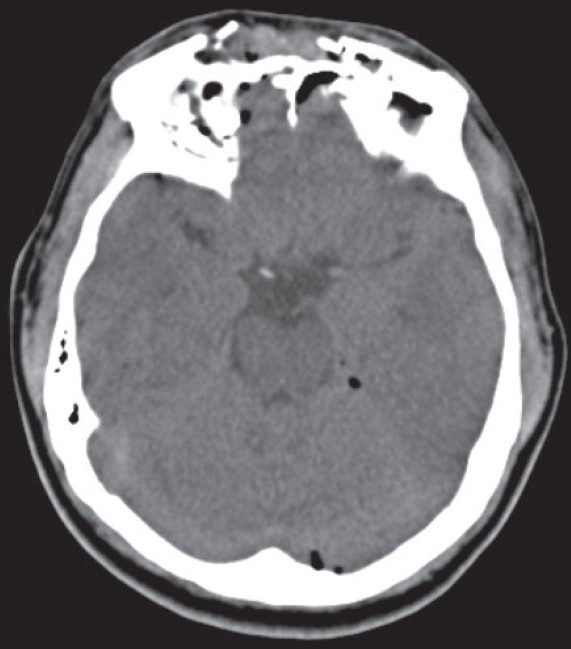
- NCCT of the head showing bilateral frontal and ethmoid comminuted depressed fracture
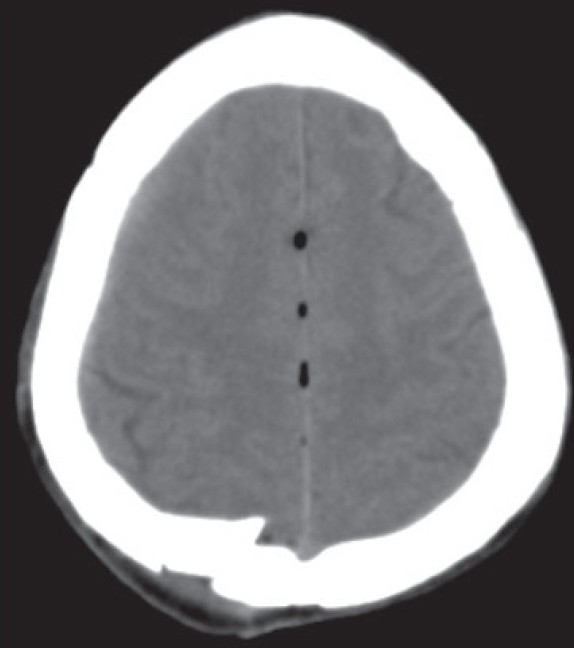
- Computerized tomography of the head demonstrated bilateral cerebral multiple hemorrhagic contusion, acute sub arachnoid hemorrhage and pneumocephalus
The patient was subjected to surgery to elevate the depressed segment, debridement and for dural repair. Dural tear was present in right frontal region and brain matter was herniating through it. The site of injury was irrigated and cleaned with limited local debridement and the dura was then closed in a watertight fashion. Depressed fontal bone fragments were elevated, the wound closed in layers and a compression dressing was applied. He was given broad spectrum antibiotics, analgesics and tetanus vaccination along with fosphenytoin as antiseizure prophylaxis. The postoperative course was uneventful and the patient was discharged on day seven without any neurological deficit and wound infection.
Case 2
A 55-year-old right-handed euglycemic and normotensive male was brought to the emergency room following the above said accident. On examination he was unconscious and responding to deep painful stimuli with a Glasgow coma scale (GCS) score of 7. Both pupils were equally reacting to light. In view of poor GCS and to protect airway, he was intubated and mechanically ventilated. His hemodynamics was stabilized and adequate saturation was maintained. During the secondary survey, the patient was found to have fracture neck of humerus and rib fracture involving three to six ribs on right side which were radiologically confirmed. There were no clinical and radiological evidences of pneumo or hemothorax. The FAST scan was negative.
There was a lacerated wound of 12 X 3 cms over the right occipital region with particulate matter. Multiple abrasions were noted on the right side of the body. There was no active bleed from the wound sites. The CT of the head demonstrated bilateral cerebral multiple hemorrhagic contusion, acute sub arachnoid hemorrhage and pneumocephalus. A linear fracture was noted at right parieto-occipital bone. His wounds were debrided and closed in layers. His humerus fracture was fixed and splinted. He was started on mannitol, antiepileptics, broad spectrum antibiotics, analgesics and tetanus vaccination. He was electively ventilated for five days and gradually weaned off from the ventilator. The postoperative course was uneventful and the patient was discharged on day 7.
Discussion
Traumatic brain injury (TBI) occurring at the workplaces, comprises about seven per cent of all TBI population,[2] and carries major economic upshot in terms of loss of wages and medical expenses. Penetrating head injuries constitute only a small part of the total number of traumatic head injuries seen in an emergency room. Non missile high-velocity penetrating brain injuries are unusual among civilian population which results in high mortality and morbidity.[3]
In civilian setup, the most common non missile penetrating cranial wounds are due to low velocity type caused by knives, nails, scissors, iron rod, fishing harpoon, electrical plug, fan blade, pencil and ceramic stone.[4–6] Similar to this case series, Abdoli and Amirjamshidi[7] reported the penetrating head wounds caused by industrial grinder tool among the construction workers. When the disc rotating at a rate of 10,000 to 15, 000 revolutions per minute is shattered, the pieces gain sufficient momentum to travel far as a missile and cause havoc. The pathophysiological consequence of penetrating head injuries depends on the kinetic energy and the trajectory of the object into the brain.[8] In the injuries with high impact velocity, the underlying traumatic damage may be severe than presumed as observed in the first case of this report. At times injuries can happen while handling he gun in a wrong manner.[9]
The local variations in thickness and strength of the skull and the angle of the impact determine the severity of the fracture and injury to the brain.[10] Impacts striking the skull at nearly perpendicular angles may cause bone fragments to travel along the same trajectory as the penetrating object, to shatter the skull in an irregular pattern, or to produce linear fractures that radiate away from the entry defect. The most appropriate management in the field is to leave the transcranial object in situ and transport the patient to the trauma center carefully. Tan and Choudhari[11] suggested that in the presence of an obvious penetrating injury with an imbedded foreign body, no attempt should be made to remove the object until the patient has had a thorough clinical and radiological evaluation. Sudden removal can cause loss of tamponade effect and subsequent catastrophic intracranial hemorrhage.
Thurner and Pollak[12] demonstrated the morphology of the wounds sustained using angle grinders that tend to follow the shape of the cutting disc; most often curvilinear but may vary slightly depending on the angle of skin entry. Tissue loss is a common feature. The volume of tissue loss is directly dependent on the size of the disc used. Finding fragments of disc and the material being cut in the wound is pathognomic of angle grinder injuries. Following the primary injury or impact, secondary injuries may occur similar to the second case. A thorough secondary survey should be performed following the initial resuscitation as per Advanced Trauma Life Support (ATLS) guidelines in order to avoid missed injuries and medico legal consequences.
Expeditious removal of the penetrating foreign body and focal debridement of the scalp, skull, dura, and involved parenchyma are the goals of surgical treatment. Watertight dural closure has long been a mainstay of the surgical management of penetrating brain injuries and serves to prevent cerebral fungus, reduce the instance of CSF leak, and provide another important barrier to infection.[13] If seizures are not evident in the acute phase, anticonvulsants may be discontinued at the end of seven days. The duration of use of antiepileptics remains somewhat controversial, but long-term use does not seem to be beneficial.[14] Despite the effectiveness of hyperventilation in rapidly reducing intracranial pressure (ICP) in some patients, its use is not recommended in view of significant reduction in cerebral blood flow which may worsen long-term neurological outcome.[15] The neurological sequelae following the non missile penetrating head injuries are determined by the severity and location of the initial injury as well as the rapidity of the exploration and fastidious debridement. The avoidance of the delayed secondary brain injury will provide a satisfactory functional outcome.
Injuries occur for a number of reasons,[16] firstly the disc itself may kick back from the surface it is cutting. This will send the rotating disc toward the operator, parallel to the axis at which it is being used. Face is more often at risk of a penetrating wound as happened in the first case since the guard has been removed while the machine was on. Our closed survey revealed that the workers were not informed well on the selection and correct fitting of the disc; and the importance of protective guard for the machine and personal protective equipments for individual operating these machines.
The shop owners surveyed said that the wrong type of disc was frequently used, increasing the likelihood of the disc shattering. Finally, shattering of the disc can occur when the disc has been incorrectly fitted. The discs rotate between 10,000 ± 15,000 rev/min, giving sufficient momentum to travel far and penetrate deeply as occurred in these cases.
As a preventive measure the users have to be taught and trained to use the correct disc size and type, wear appropriate personal protective equipments, use the angle grinder with protective guard and maintain the safety by standing perpendicular to the plane of the cutting wheel, and thereby can greatly reduce the occurrence of such injuries. Also, the supervisors in the field have to monitor the safety measures constantly. In addition the healthcare workers have to be oriented well to handle such cases carefully.
Dr. E. Ravi, M.D (Radiology) for his valuable suggestion in preparing this manuscript. Mr. V. Chakravarthy, Manager, IT & EDP, Sri Gokulam Hospital and Research Institute, Salem, for his secretarial assistance.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Early predictors of mortality in penetrating compared with closed brain injury. Brain Inj. 2001;15:801-10.
- [Google Scholar]
- Penetrating craniocerebral injury caused by a metal rod: An unusual case report. Injury. 1990;21:414-5.
- [Google Scholar]
- Penetrating craniocerebral injury from an underwater fishing harpoon. Childs Nerv Syst. 2000;16:117-9.
- [Google Scholar]
- Transorbital penetrating cerebral injury with a ceramic stone: Report of an interesting case. Neurol India. 2009;57:331-3.
- [Google Scholar]
- Work-related penetrating head trauma caused by industrial grinder tool. Arch Iran Med. 2009;12:496-8.
- [Google Scholar]
- Unusual mode of firearm injury from the recoiled rear end of gun barrel. Singapore Med J. 2008;49:e238-41.
- [Google Scholar]
- History of the management of craniocerebral wounds. In: Aarabi B, Kaufman HH, Dagi TF, George ED, Levy ML, eds. Missile Wounds of the Head and Neck. Vol 1. Park Ridge, Ill: American Association of Neurological Surgeons; 1999. p. :281-92.
- [Google Scholar]
- A national survey of neurosurgical care for penetrating head injury. Surg Neurol. 1991;36:370-7.
- [Google Scholar]
- Secondary insults associated with severe closed head injury. Contemp Neurosurg. 1992;14:1-8.
- [Google Scholar]
- Penetrating facial injury from angle grinder use: management and prevention. Head Face Med. 2008;4:1.
- [Google Scholar]






