Translate this page into:
Orbital Tuberculosis with Intracranial Extension
Address for correspondence: Dr. Batuk Diyora, Department of Neurosurgery, LTMMC and LTMG Hospital, Sion, Mumbai - 400 022, Maharashtra, India. E-mail: bddiyora@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of orbital tuberculosis (OTB) with intracranial extension without active tuberculosis in the rest of the body organs or a history of tuberculosis infection. A 29-year-male patient presented with left-sided painful periorbital swelling with pus discharging sinus and visual impairment. Orbital computed tomography revealed contrast enhancing cystic mass lesion in the left orbit with erosion of the lateral and superior orbital wall with intracranial extension. After the failure of 3 weeks’ course of oral antibiotics, the patient underwent left lateral orbitotomy, pus was drained out, and granulation tissues were excised. Histopathological examination confirmed OTB. The patient had received antituberculous treatment. Periorbital swelling completely disappeared and vision improved over a period of 2 weeks. OTB should be considered in differential diagnosis of periorbital swelling especially when it does not respond to oral antibiotics.
Keywords
Orbitotomy
sinus
tuberculosis
INTRODUCTION
Tuberculosis is one of the leading causes of morbidity and mortality in the developing countries. It can involve any organ in the body; orbit is no exception. Orbital tuberculosis (OTB) is rare, even in places where tuberculosis is endemic.[1] OTB is rare form of extrapulmonary tuberculosis. Infection can reach to the orbital periosteum or tissue either through hematogenous spread or as a result of direct extension from paranasal sinuses. OTB needs differentiation from Tolosa–Hunt Syndrome, orbital pseudotumor, and nontuberculous infection as they are other common inflammatory conditions of the orbit.[2] Diagnosis is usually based on tissue examination in the form of histopathological evidence granulomatous lesion or presence of acid-fast bacilli (AFB). Antituberculosis drugs remain the mainstay of treatment. Surgery usually required for tissue diagnosis. We present a case of OTB presented with orbital mass and treated with surgery followed by antituberculous medicine with good clinical outcome.
CASE REPORT
A 29-year-male presented with left-sided painful progressive periorbital swelling with pus discharging sinus [Figure 1]. He also complained of impaired vision in the left eye. Earlier he received 3-week course of oral antibiotic, but there was a reduction in the size of swelling or improvement in vision. Ophthalmic examination revealed swollen, red, edematous left eyelid with corneal and conjunctival congestion. Visual acuity was 6/24 and there was evidence of early mild papilledema on the left eye. There was restriction of left lateral rectus muscle movement. Right eye examination was normal. Computed tomography (CT) scan of the orbit revealed contrast-enhancing mass lesion of about 3 cm × 1.3 cm size over superolateral aspect of the left orbit [Figure 2a]. Lesion was eroding the lateral orbital wall and extending into cranium [Figure 2b].

- Clinical photograph showing left periorbital swelling
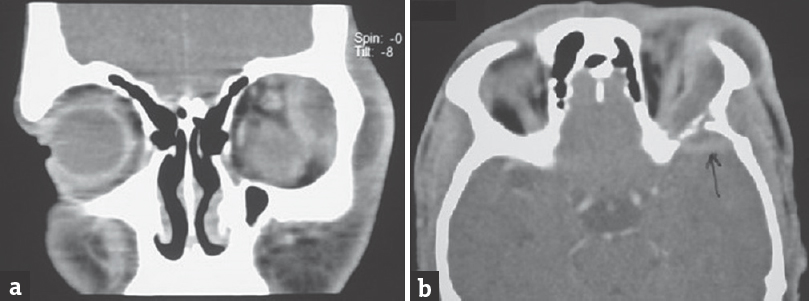
- Contrast enhancing computed tomography scan brain; coronal view (a), showing left lateral orbital mass displacing eyeball medially and downward and axial view (b) showing erosion of lateral orbital wall with extension of lesion in to cranial cavity
In view of medically non-responsive orbital swelling and visual impairment, decision was taken for exploration. The patient underwent left lateral orbitotomy under general anesthesia. Pus was drained out and sends for AFB staining and culture study. Necrotic bony and inflammatory tissues were excised and sent for histopathological examination. Wound thoroughly washed with antiseptic solutions. Pus culture as well as AFB stain were negative while histopathological examination of excised tissue showed the presence of chronic inflammatory cells along Langerhans giant cells suggestive of tuberculosis. His X-ray chest was normal, and Monteux test was negative, so the final diagnosis of primary OTB was made. Following the surgery, inflammation completely subsided, vision improved, and extraocular movements became normal [Figure 3]. The patient was kept on antituberculous treatment (ATT) for 18 months. At 3 years’ follow-up, there was no evidence of recurrence.

- Postoperative clinical photograph showing complete disappearance of left orbital swelling with normal movement of left lateral rectus
DISCUSSION
Tuberculosis most commonly presents as initial pulmonary disease which may disseminate to involve various organs. As tuberculosis is primarily an infection of lymphoid tissue, the bacilli are confined by the lymph follicles of the mucosa or by the regional lymph nodes. If the bacilli pass the lymph follicles and the lymph nodes, they may be carried to the eye through the bloodstream. Orbital involvement by tuberculosis may be in primary or secondary form.[3] In secondary ocular tuberculosis, infection results either from contiguous spread from adjacent structures or by the hematogenous route.[4] Intracranial extension of orbital tuberculoma is extremely rare, and it may occur in the form of extradural abscess and infra-temporal fossa extension.[1] Limited information is available about tuberculous disease eroding the lateral orbital wall and spreading to the temporal lobe.[5]
Earlier OTB classified into two broad group; periostitis and tuberculoma. However, Madge et al. reviewed the literature on the subject and divided these patients in five different groups (1) classical periostitis; (2) orbital soft-tissue tuberculoma or cold abscess, with no bony destruction; (3) orbital TB with evidence of bony involvement, not categorized as (1); (4) orbital spread from the paranasal sinuses; and (5) dacryoadenitis.[6] However, there was no detail about the extension of OTB into the cranium. In our case, orbital pathology not only involved lateral orbital bony wall but also extended into the bony cranium.
The clinical features of OTB are insidious and include progressive unilateral proptosis, conjunctival chemosis and hyperemia, restricted ocular movements, reduced visual acuity, and reduction in visual fields.[78910] The differential diagnosis includes medial orbital subperiosteal abscess, complication of the sinusitis which requires surgical decompression when not responding to conservative treatment; orbital pseudotumor, lymphoma, and cavernous hemangioma.[11]
Early diagnosis and prompt treatment of this clinical entity may prevent ocular morbidity and blindness.[12] Diagnosis of OTB can be delayed as in our case. Orbital imaging is recommended in patients with orbital swelling. CT will not only diagnose the presence of infection but also documents bony involvement. Although radiological features may be suggestive of OTB, tissue diagnosis is must. The presence of AFB, characteristic histopathology, and growth of Mycobacterium tuberculosis from such a specimen remains the gold standard for diagnosis.[11] Newer tests such as whole blood interferon-gamma immunological tests and polymerase chain reaction-based tests of pathological specimens have proven useful.[2]
Like management of pulmonary tuberculosis, OTB treatment is equally complex with the goal of cure of disease and prevention or minimization of transmission. It requires high levels of patient adherence due to long courses of multiple antituberculous medications. Standard ATT for 12–18 months completely resolves the lesion in most cases. Although medicine remains the mainstay of treatment, surgery is usually reserved on for tissue diagnosis. Surgical approach depends on exact location of the lesion in the orbit and includes lateral orbitotomy, medial orbitotomy, and superior orbitotomy.[6]
CONCLUSION
OTB is an uncommon ophthalmic disease and has the potential for serious complications which demands immediate and aggressive action. High index of suspicion is required while dealing with the orbital mass in an endemic region. Periorbital swelling associated with the conjunctival congestion and corneal chemosis not responding to the routine antibiotics should be explored to achieve good clinical results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Bilateral ocular scrofuloderma with orbital tuberculosis. Indian J Pediatr. 2006;73:361-3.
- [Google Scholar]
- Tuberculosis of the orbit and lacrimal gland: A clinical study of 14 cases. J Pediatr Ophthalmol Strabismus. 1980;17:232-8.
- [Google Scholar]
- Orbital tuberculosis diagnosed by immunohistochemistry: Case reports. Rev Inst Med Trop Sao Paulo. 2004;46:291-4.
- [Google Scholar]






