Translate this page into:
Neurosurgical Emergencies at a Tertiary Referral Center in a Sub-Saharan African Country
Thierry Alihonou Department of Surgery, Departmental Teaching Hospital of Ouémé–Plateau, Faculty of Health Sciences, University of Abomey-Calavi, Cotonou 01BP5226 Porto-Novo Benin alihonouthierry@yahoo.fr
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background The practice of neurosurgery in a teaching hospital requires modern diagnostic tools and a rigorous organization of care.
Objectives To present and discuss the management of neurosurgical emergencies in a teaching hospital in poor and low-income country.
Patients and Methods This is a retrospective and descriptive study from April 2015 to March 2017 and includes traumatic and nontraumatic neurosurgical emergencies. Epidemiological, diagnostic, operative, and outcome data were evaluated.
Results During the study period, 397 cases of neurosurgery were admitted. One hundred seventy-five of them were emergencies (43%), including 168 (96%) of traumatic origin. The average age was 32.5 years (1–80 years) with a male predominance: 149 men for 26 women, the sex ratio was 6.68. The cause of the neurotraumatological emergency was mostly road accidents with 143 cases (85.1%). The trauma was brain injury in 155 patients (92.3%) and spine injury in 13 patients (7.7%). In 64.3% of cases, diagnostic imaging was done beyond 48 hours. Surgery time was more than 48 hours when it was performed (21 cases). Outcome was good for 19 patients. Overall and postoperative mortality were, respectively, 34.5% (58 cases) and 9.5% (2 cases).
Conclusion Neurosurgical emergencies care at the Departmental Teaching Hospital of Ouémé–Plateau has become a common activity with encouraging operating results despite difficult practice conditions.
Keywords
trauma
spine
emergencies
neurosurgery
Introduction
The practice of neurosurgery requires the use of essential diagnostic tools. Neurosurgery at teaching tertiary referral center, Departmental Teaching Hospital of Ouémé–Plateau, in Porto-Novo, like other countries in the subregion,1 2 is fairly recent and still suffers from the lack of material resources and qualified personnel for the management of neurosurgical emergencies.3 4 5 We suggest reporting an overview of this management in this center.
Patients and Methods
It was a descriptive study with retrospective data collection from April 1, 2015, to March 31, 2017, at the teaching tertiary referral center of Ouémé–Plateau, in Benin Republic. This hospital located in South-East Benin and serves two departments, Ouémé and Plateau, for a population of nearly 1,700,000 inhabitants. It was created in 1906 and has become a university hospital by decree since August 2014 as a result of the extension of the university hospital space in Benin. Care, teaching, and research activities are therefore performed. Its capacity is currently 334 beds. The study involved all patients admitted to the Departmental Teaching Hospital of Ouémé–Plateau for a traumatic or nontraumatic neurosurgical emergency. A survey form was completed for this purpose for each patient. The evaluated parameters were epidemiological, diagnostic, therapeutic, and outcome. The collected data were entered in the form of a database with the software EPI data 3.1. The analysis was made by software SPSS version 21.0, and the tables and graphs for the organization of the results by Microsoft Excel 2013. Outcome was considered favorable when the patient left hospital without neurological aftereffect which could cause dependence toward their circle.
Results
During the study period, 397 patients were treated for neurosurgical pathology. Among them, 175 cases constituted emergencies or 43% of admissions for neurosurgery. The origin was traumatic in 96% of cases (168 patients). The average age of patients was 32.5 years with extremes ranging from less than 1 year to 80 years. There was a male predominance with a sex ratio of 5.73 (149 men/26 women). Accidents on the public highway were at the forefront of traumatic etiologies (143 cases, 85.1%). A two-wheeled vehicle was involved in 88 cases (61.53%). The site of the trauma was cranial in 92.3% of the cases (155 patients) and spine in 7.7% of the cases (13 patients). Among the cranial trauma victims, 73 patients had a serious trauma (47.09%). The average delay to admit these emergencies was 6 hours in 14% of cases (Table 1); in 33% of cases, this delay was not specified. Diagnostic imaging was performed more than 48 hours on average after admission in 63.4% of the cases. The brain scan was performed on 52 cranial trauma victims (33.54%). The traumatic lesions were essentially a cerebral contusion (32 patients, 61.53%), a cranial fracture (30 patients, 57.69%), and an intracranial blood collection in 20 patients, that is, 38.46% of the cases. In the spine, it was a vertebral fracture (eight patients) and/or a dislocation (six patients). These lesions are listed in Table 2.
|
Delay |
Frequency |
Percentage (%) |
|---|---|---|
|
< 6 h |
25 |
14.28 |
|
6–24 h |
56 |
32 |
|
> 24 h |
37 |
21.14 |
|
Not specified |
57 |
32.57 |
|
Lesions |
Frequency |
Percentage (%) |
|---|---|---|
|
Skull fracture |
30 |
57.69 |
|
Brain contusion |
32 |
61.53 |
|
Cranial hematoma |
20 |
38.46 |
|
Subarachnoid Hemorrhage |
5 |
9.61 |
|
Vertebral fracture |
8 |
61.53 |
|
Vertebral dislocation |
6 |
46.15 |
Seven patients (4%) were admitted for a nontraumatic neurosurgical emergency (Table 3). Among them, three cases of cerebral convexity meningioma, only of women, presented on admission a deterioration of consciousness, a state of convulsive disease, or a malignant HTIC.
|
Nature |
Frequency |
|---|---|
|
Meningioma |
3 |
|
Hydrocephalus |
2 |
|
Spinal cord compression |
2 |
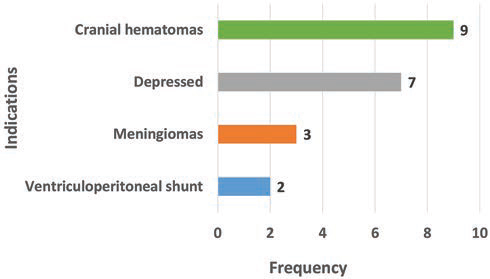
Therapeutically, 85 patients (48.57%) were put in intensive care with an average stay of 5 days (1–60 days). Twenty-eight patients were operated on (16%): 21 for a cranial pathology (Fig. 1) and 7 for a spinal pathology (Table 4). The average operating deadline was 10 days. Surgery was performed beyond 48 hours for all emergencies operated on. Three patients received orthopaedic treatment.
|
Indications |
Frequency |
|---|---|
|
Laminectomy |
3 |
|
Spine fusion |
4 |
|
Total |
7 |
-
Fig. 1 Distribution of surgery indications for emergencies in cranial pathology.
Fig. 1 Distribution of surgery indications for emergencies in cranial pathology.
The outcome was favorable for 98 patients (56%). Among patients operated on meningioma, two had a recovery without aftereffect and resumed their activities; the third died 72 hours after surgery. The overall mortality of the series was 33.71% (59 patients). Postoperative mortality was 14.28% (4 patients). The average hospital stay was 11.5 days.
Discussion
Difficulties of the Study
Due to its retrospective nature, this study was not without pitfalls. Nearly a hundred files were unexploited due to insufficient data and due to weaknesses in files archiving policy within the Departmental University Hospital Center of Ouémé-Plateau (lack of staff and facilities, storage conditions, and absence of electronic archiving).
Epidemiology
The young age of patients and the male predominance of neurotraumatic emergencies admitted to the Departmental Teaching Hospital of Ouémé–Plateau are constantly reported by the literature. The same applies to the predominant etiology of road accidents.6 7 8 9
Neurotrauma Due to Two-Wheeled Vehicles
The phenomenon of taxis is widespread in Benin and in the subregion. This partly explains the increasing number of road accidents involving the motorcyclists. Rabiou et al2 and Tidjani et al10 reported, respectively, a rate of 70.28 and 57.9% compared with 61.53% in our series. The cost of wearing a helmet was 5.15 and 3.5%, compared with 9.1% for our study and no patient for Nwadiaro et al.11 Compliance with traffic rules by users has greatly favored the occurrence of these accidents. In addition, risky behaviors can be aggravating factors of traumatic lesions. A recent study performed on a population of 310 cranial trauma victims, drivers or passengers of two-wheeled motorcycles, reported that only 11 were wearing a helmet at the time of the trauma.10 It also mentioned that the primary cranial lesions were more serious in patients without a helmet and the frequency of these primary lesions requiring surgery. In this regard, it should be noted here the reluctance of users of two-wheeled vehicles in Benin to comply with wearing a helmet despite the promulgation of the law. Even we notice a “forced” awareness in Cotonou after the repressive phase, it is not the same yet in Porto-Novo.12 The corollary is high percentage of severe cranial trauma that results from it: 47.09% in our series against 29.42% for Rabiou et al2 and 25.9% for Fatigba et al.7 This absence of helmet use is a recurring problem in the subregion; the impact of wearing a helmet on the seriousness of cranial injuries is no longer to be demonstrated.10 12 13 14 15 Accidents on the public highway are also causes of spinal cord injury. Even if standard radiography was sufficient in the majority of cases for their diagnosis, their management remains essentially confronted with the financial inaccessibility of implants for the stabilization of the spine.
Prehospital and Hospital Care
Prehospital management of neurotrauma in developed countries helps reduce morbidity and mortality.2 This remains a thorny issue in an African context where resources are limited. The delay for admission to neurosurgical emergencies was beyond 24 hours for more than half of the patients in this study. This delay remains high and can be superimposed on that reported by the majority of African series where the organization of treatments and the prehospital and hospital care of emergencies still encounters many difficulties.2 16 17 18 19
Regarding the diagnosis of neurotraumatic emergencies, the difficulties remain the same in terms of availability and accessibility to modern neuroimaging tools. Lesions due to cranial and/or spine injury are also superimposable in the various studies.18 19 20 21 22 23
The difficulties to provide quality care (management delay, availability of staff, and the appropriate technical platform) are the same in West and Central African subregion. Added to this is the absence of universal health insurance for populations who are required to insure their own health expenses.24 25 An outline by Dechambenoit published in 2002 gave a good account of this situation.26
Nontraumatic Emergencies
Three cases of cranial meningioma benefited from an emergency Simpson I resection despite difficult working conditions (lake of operating room consumables and resuscitation). Among the cases of hydrocephalus, there was a 14-year-old girl, who underwent emergency ventriculoperitoneal shunt for a rapidly progressive decompensating hydrocephalus due to a known Dandy–Walker malformation. Her outcome was good. The management of nontraumatic neurosurgical emergencies at the Departmental Teaching Hospital of Ouémé–Plateau mainly suffers from the weakness of the technical platform, the unavailability of consumables and poor accessibility to diagnostic neuroimaging. This results in a biased assessment of the reality of these emergencies and a poorer provide care to the population.
Treatment and Outcome
Surgery rate, the type of surgical procedure, the delay, and the outcome parameters are usually reported in many sub-Saharan African studies. Surgery perform ranged from 16% (our series) to 75.8%9 19 and hospital mortality from 3.3%2 9 19 to 37.71% (our series). The high mortality rate in our study reflects the efforts that remain to be made to reduce it and offer better chances of survival to our populations.
Conclusion
This work presents an overview of the management of neurosurgical emergencies which has become a common activity at teaching tertiary referral center of Ouémé–Plateau in Porto-Novo. Despite encouraging operating results in difficult practice conditions, the essential improvement in the technical platform would contribute to more efficient care of these neurosurgical emergencies.
Conflict of Interest
None declared.
References
- Epidemiological patterns of head injury in a newly established neurosurgical service: one-year prospective study. Afr J Med Med Sci. 2008;37(4):383-388.
- [Google Scholar]
- Traumatismes crânio-encéphaliques à l’Hôpital National de Zinder: étude rétrospective à propos de 153 cas. Ann. l’Université Abdou Moumouni Niamey Série A Sci. exactes, Nat. Agron. la santé. 2016;2(11):143-151.
- [Google Scholar]
- African neurosurgery: current situation, priorities, and needs. Neurosurgery. 2001;48(6):1344-1347.
- [Google Scholar]
- African neurosurgery, the 21st-century challenge. World Neurosurg. 2010;73(4):254-258.
- [Google Scholar]
- Trauma cranien: Quelle prise en charge dans un milieu neuro-chirurgical sous equipe?: Cas de l’hôpital Gabriel toure de Bamako –Mali. Med Afr Noire. 2007;54(2):73-77.
- [Google Scholar]
- Épidémiologie des traumatismes crânio-encéphaliques à Parakou (Bénin) AJNS. 2010;29(1):25-33.
- [Google Scholar]
- Aspects cliniques et radio-anatomiques des traumatismes crânio-encéphaliques par accident de la circulation dans un centre hospitalier au Bénin. Tunis Med. 2011;89(11):837-840.
- [Google Scholar]
- Epidemiology of traumatic brain injury in eastern China, 2004: a prospective large case study. J Trauma. 2008;64(5):1313-1319.
- [Google Scholar]
- Profil des traumatismes crânio-encéphalique et vertébro-médullaire liés aux accidents de la voie publique en Guinée. Neurochirurgie. 2012;58(5):287-292.
- [Google Scholar]
- Helmet wearing and traumatic brain injuries among motorcyclists in Cotonou. J Surg (Northborough). 2018;6(3):73-77.
- [Google Scholar]
- Motorcycle injuries in North-Central Nigeria. Niger J Clin Pract. 2011;14(2):186-189.
- [Google Scholar]
- Impact de la loi portant sur l’obligation du port du casque à Cotonou sur les traumatismes crânio-encéphaliques (Bénin) Med Afr Noire. 2017;6409:423-429.
- [Google Scholar]
- Motorcycle helmet-use laws and head injury prevention. JAMA. 1992;267(12):1649-1651.
- [Google Scholar]
- [Skull injuries resulting from motorcycle accidents, Benin] Mali Med. 2011;26(4):60-64.
- [Google Scholar]
- Incidence et impacts des accidents de la voie publique chez les conducteurs de taxi-moto en milieu tropical. Rev Chir Orthop Traumatol. 2016;102(2):211-214.
- [Google Scholar]
- Motah M, Ndoumbe A, Kuate C, Youngui BT, Ngonde C, Djientcheu VdP. Prise en charge pré-hospitalière des patients victimes de traumatisme vertébro-médullaire en milieu africain. Heal Sci Dis 2014;15(2)
- Prehospital transport of patients with spinal cord injury in Nigeria. J Spinal Cord Med. 2011;34(3):308-311.
- [Google Scholar]
- The clinical profile and acute care of patients with traumatic spinal cord injury at a tertiary care emergency centre in Addis Ababa, Ethiopia. Afr J Emerg Med. 2016;6(4):180-184.
- [Google Scholar]
- Surgical management of head trauma: problems, results, and perspectives at the Departmental Teaching Hospital of Borgou, Benin. World Neurosurg. 2013;80:246-250. (3-4)
- [Google Scholar]
- Traumatismes du rachis à l’hôpital Principal de Dakar (HPD): à propos de 126 cas. Neurochirurgie. 2013;59(6):256.
- [Google Scholar]
- Pattern and outcome of management for traumatic closed cervical spine injuries at the national orthopaedic hospital, Enugu, Nigeria. Niger Heal J. 2011;11(1):27-31.
- [Google Scholar]
- Apport de l’imagerie medicale dans le bilan des traumatismes craniens au niger: à propos de 311 cas à l’Hôpital National de Niamey. J Afr Imag Méd. 2012;4(1):4-11.
- [Google Scholar]
- Apport de la tomodensitométrie dans la prise en charge des traumatismes crânio- encéphaliques à Bamako. Mali Méd. 2005;20:1-2.
- [Google Scholar]
- The direct cost of treatment of traumatic brain injury in a sub-Saharan African Country (Benin) World Neurosurg. 2017;99:210-213.
- [Google Scholar]
- Neurosurgical development in the East, Central, and Southern African (ECSA) regions: past, present, and future. World Neurosurg. 2017;99:782-783.
- [Google Scholar]
- Stratégie de développement de la neurochirurgie en Afrique: une esquisse. Af J NeurologicalSci.. 2002;21(1):1.
- [Google Scholar]






