Translate this page into:
Effects of COVID-19 on Neurosurgical Service: Perspective from a Tertiary Medical Center in Nigeria
Ankit I. Mehta, MD, FAANS Department of Neurosurgery, University of Illinois at Chicago 912 South Wood Street, 451-N, Chicago, Illinois 60612 United States ankitm@uic.edu
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background The outbreak of COVID-19 caused a significant impact on neurosurgical case volume in Nigeria due to the widespread recommendation to minimize elective procedures and redistribute healthcare resources to support COVID-19 patients. This study aims to analyze the effect of COVID-19 in one tertiary care Nigerian hospital on the demographic characteristics, diagnostic classes, and elective/non-elective procedure statuses.
Methods A retrospective single-center chart review study was conducted to review all patients undergoing a neurosurgical procedure between March to June in 2019 and 2020. Descriptive data on patient age, gender, sex, diagnosis, surgical procedure, elective/non-elective surgery status, and month and year of admission were recorded. Diagnoses were categorized into one of seven types by author review. Pearson's Chi-Square and Fisher's Exact Tests were utilized to test for independence of the categorical variables to the year of patient admission, and a Welch two-sample t-test was used to test for a significant difference in mean age between the two cohorts.
Results A total of 143 cases were reviewed. There was a 59.8% reduction in overall neurosurgical case volume with an 82% reduction in elective procedures (39 vs. 7, p = 0.017, 95% CI: 1.15 – 8.77) between 2019 and 2020. No significant differences were noted in patient cohorts when comparing demographic characteristics, diagnosis type, or month of admission between the two years.
Conclusion There was a significant reduction in elective neurosurgical procedures during the early months of COVID-19 in Nigeria. Further studies should consider examining the effects of COVID-19 into 2021.
Keywords
COVID-19
neurosurgery
demographic
Nigeria
elective
emergent
Introduction
Due to the rising case numbers of coronavirus disease 2019 (COVID-19) patients, the American College of Surgeons recommended postponing or canceling nonemergent surgeries in mid-March 2020, with similar recommendations made worldwide.1 2 3 4 5 The consequences of these recommendations led to significant decreases in the volume of neurosurgical cases, as many neurosurgical and neurointensive care beds were rationed to support COVID-19 patients.3 5 6 7
Nigeria, too, was affected by a rising number of COVID-19 cases4 8 and to cope with the difficulties posed by the pandemic, the health care system appropriately shifted attention and resources to treating patients with COVID-19. As a result of restructuring, modifications were made to streamline operations, and a 60-bed block was dedicated to patients with COVID-19. All departments, including neurosurgery, temporarily closed in-person outpatient clinics, and all elective surgeries were suspended. With this halt on elective procedures, there is a growing concern that many patients are currently living with unaddressed or underaddressed neurosurgical disease.9
Although several studies have examined the effects of the COVID-19 pandemic on neurosurgical case volume, few studies have examined the effects in Nigeria.2 10 The purpose of this study was to compare the demographic characteristics, diagnostic classes, and surgical elective/nonelective statuses of those patients undergoing neurosurgery during the COVID-19 pandemic in 2020 with those prepandemic in 2019 in one tertiary-care Nigerian hospital.
Methods
Data from 143 neurosurgically treated patients at Lagos University Teaching Hospital (LUTH), Lagos, Nigeria between March and June 2019 and 2020 were retrospectively collected via chart review. Ethical approval to conduct the study was granted by the Health Research Ethics Committee (HREC) at LUTH (HREC number: ADM/DCST/HREC/APP/3738). Age, sex, diagnosis, surgical procedure, elective/nonelective surgery status, and month and year of admission were recorded. For analysis, the pediatric population was defined by age younger than 18 years and the adult population was defined by an age of 18 years or older. Diagnoses were then organized into one of seven categories (congenital malformation/condition, cranial tumor, adult hydrocephalus, pediatric infection, spine, trauma, vascular, and cerebrospinal fluid leak) based on review by the authors. This information is summarized in Supplementary Table S1, available in the online version only.
|
Total |
2019 |
2020 |
p-Value |
95% CI |
|
|---|---|---|---|---|---|
|
N |
143 |
102 (71.3%) |
41 (28.7%) |
||
|
Age |
|||||
|
Mean (y) |
30.6 |
31.29 |
28.89 |
0.622 |
−7.26 to 12.05 |
|
25th %–75th % (y) |
4.5–54 |
6.25–54 |
0.33–47 |
||
|
Range (y) |
0.014–76 |
0.027–76 |
0.014–75 |
||
|
Population |
|||||
|
Pediatric |
61 (42.7%) |
43 (42.2%) |
18 (43.9%) |
0.854 |
0.48–2.37 |
|
Adult |
82 (57.3%) |
59 (57.8%) |
23 (56.1%) |
||
|
Sex |
|||||
|
Male |
94 (65.7%) |
65 (63.7%) |
29 (70.7%) |
0.56 |
0.59–3.32 |
|
Female |
49 (34.3%) |
37 (36.3%) |
12 (29.3%) |
||
|
Elective/nonelective |
|||||
|
Elective |
46 (32.2%) |
39 (38.2%) |
7 (17.1%) |
0.017 |
1.15–8.77 |
|
Nonelective |
97 (67.8%) |
63 (61.8%) |
34 (82.9%) |
||
|
Diagnosis type |
|||||
|
Congenital malformation/condition |
33 (23.1%) |
21 (20.6%) |
12 (29.3%) |
0.4377 |
N/A |
|
Cranial tumor |
38 (26.6%) |
29 (28.4%) |
9 (22.0%) |
||
|
Adult hydrocephalus |
5 (3.5%) |
4 (3.9%) |
1 (2.4%) |
||
|
Pediatric infection |
14 (9.8%) |
10 (9.8%) |
4 (9.8%) |
||
|
Spine |
14 (9.8%) |
13 (12.7%) |
1 (2.4%) |
||
|
Trauma |
12 (8.4%) |
7 (6.9%) |
5 (12.2%) |
||
|
Vascular |
26 (18.2%) |
17 (16.7%) |
9 (22.0%) |
||
|
CSF leak |
1 (0.7%) |
1 (1.0%) |
0 (0%) |
||
|
Month |
|||||
|
March |
41 (28.7%) |
28 (27.5%) |
13 (31.7%) |
0.8055 |
N/A |
|
April |
32 (22.4%) |
25 (24.5%) |
7 (17.1%) |
||
|
May |
39 (27.3%) |
27 (26.5%) |
12 (29.3%) |
||
|
June |
31 (21.7%) |
22 (21.6%) |
9 (22.0%) |
||
Abbreviations: CI, confidence interval; CSF, cerebrospinal fluid; N/A, not available.
Descriptive statistics for the total population and two subgroups were calculated. Pearson's chi-square and Fisher's exact tests were utilized to test for independence of the categorical variables to the year of patient admission. Similarly, a Welch two-sample t-test of unequal variance was used to test for a significant difference in mean age between the 2019 and 2020 patient cohorts. The α level utilized was 0.05. Statistical analysis was performed using R Studio (Version 1.4.1717, Boston, Massachusetts, United States). This information is summarized in Table 1.
Results
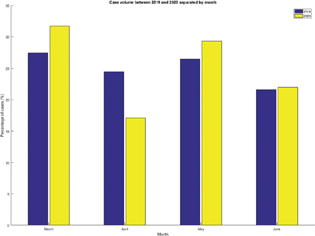
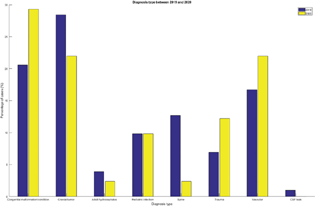
A total of 143 patients required neurosurgery during the 4-month (March–June) span of 2019 and 2020, of which 102 underwent surgery in 2019 and 41 underwent surgery in 2020. The mean age of the 2019 and 2020 cohorts were 31.29 and 28.89, respectively. Adults comprised 57.8 and 56.1% of the 2019 and 2020 cohorts, respectively. Males comprised 65.7 and 63.7% of the 2019 and 2020 cohorts, respectively; 61.8% of 2019 patients and 82.9% of 2020 patients underwent neurosurgery for nonelective indications. The distribution of patients treated in March, April, May, and June 2019 and 2020 was similar (p = 0.8055) (Fig. 1). Cranial tumors (28.4%), congenital malformations/conditions (20.6%), and vascular conditions (18.2%) were the most common diagnostic categories of patients surgically treated in 2019. Similarly, congenital malformations/conditions (29.3%), cranial tumors (22.0%), and vascular conditions were the most common diagnostic categories of patients surgically treated in 2020 (Fig. 2). There was a significantly larger proportion of patients treated nonelectively (emergently/urgently) in 2020 compared with 2019 (82.9 vs. 61.8%, p = 0.017, 95% confidence interval = 1.15–8.77). There were no other statistically significant differences between the 2019 and 2020 patient cohorts.
-
Fig. 1 Case volume between 2019 and 2020 separated by month.
Fig. 1 Case volume between 2019 and 2020 separated by month.
-
Fig. 2 Diagnosis type between 2019 and 2022.
Fig. 2 Diagnosis type between 2019 and 2022.
Discussion
The rising cases of the COVID-19 pandemic caused widespread recommendations to limit the number of elective neurosurgical cases worldwide. In Nigeria, the number of neurosurgical operations at LUTH saw a reduction of nearly 60% from 2019 to 2020, 82% of which were elective procedures. Overall, this reduction is consistent with available literature with a reported 50 + % reduction of neurosurgical cases during this time.1 3 Similarly, in a cross-sectional survey given to African neurosurgeons, 54.7% of responders reported that elective surgeries were not being performed, with an overall median reduction of 80% of elective cases per clinician.4 The overall significant reduction in elective procedures likely reflected the widespread recommendation to reduce and postpone the number of elective procedures and the reallocation of health care workers to manage COVID-19 patients.
Despite this reduction, the demographics of the two cohorts treated (age, population type, and sex) did not differ, which is consistent with the experiences of other institutions.3 5 Although the diagnosis type did not differ significantly between years, the proportion of trauma and vascular cases increased in 2020, while the proportion of cranial tumor and spine procedures decreased in this time frame. This trend of a decreased proportion of spine and cranial tumor procedures is similar to the experiences at other institutions,1 3 5 6 7 likely reflecting a reduction in elective surgeries to prioritize emergent procedures. It is also possible that the increased proportion of vascular cases seen in 2020 partially reflects the increased incidence of stroke seen in COVID-19 patients.11
The response of the Nigerian government to the coronavirus outbreak consisted of an initial lockdown in late March with the partial lifting of restrictions in early May.4 8 Despite measures to reduce transmission, the number of cases steadily rose from March to June 2020.8 Interestingly, our data did not demonstrate significant differences in number of procedures performed by month between 2019 and 2020. Specifically, the proportion of case numbers per month remained relatively consistent in 2019, while the number of procedures in 2020 fluctuated.
This study had several limitations. First, as the study represents a retrospective chart review analysis, data mis-entry and omission are possible. Second, the authors could not always define if specific vascular diagnoses were traumatic or nontraumatic based on the available information, which confounded the ability to categorize the few cases into the vascular or traumatic diagnosis type. For instances in which an acute cerebrovascular diagnosis was documented, the authors decided that the case would be categorized as vascular if no other fractures or signs or symptoms of trauma were listed.
Future studies should consider expanding this study to include all months in the year and assess trends into 2021 and 2022 to better characterize the effects of COVID-19 on the neurosurgical service.
Acknowledgment
The authors are grateful for the support of the Department of Neurosurgery, Lagos University Teaching Hospital for allowing them to conduct the study.
Conflict of Interest
None declared.
References
- The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien). 2020;162(6):1229-1240.
- [Google Scholar]
- The impact of COVID-19 on neurosurgical services in Africa. World Neurosurg. 2021;146:e747-e754.
- [Google Scholar]
- Neurosurgery and coronavirus: impact and challenges-lessons learnt from the first wave of a global pandemic. Acta Neurochir (Wien). 2021;163(2):317-329.
- [Google Scholar]
- Nigeria's public health response to the COVID-19 pandemic: January to May 2020. J Glob Health. 2020;10(2):20399.
- [Google Scholar]
- Case volumes and perioperative coronavirus disease 2019 incidence in neurosurgical patients during a pandemic: experiences at two tertiary care centers in Washington, DC. World Neurosurg. 2020;143:e550-e560.
- [Google Scholar]
- Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. World Neurosurg. 2020;139:e877-e884.
- [Google Scholar]
- Sheltered neurosurgery during COVID-19: the Emory experience. World Neurosurg. 2020;144:e204-e209.
- [Google Scholar]
- Descriptive epidemiology of coronavirus disease 2019 in Nigeria, 27 February-6 June 2020. Epidemiol Infect. 2020;148:e208.
- [Google Scholar]
- COVID-19 nonessential surgery restrictions and spine surgery: a German experience. Spine. 2020;45(14):942-943.
- [Google Scholar]
- The effect of the COVID 19 pandemic on elective surgical services in Jos, North Central, Nigeria. J Biosci Med (Irvine). 2021;9(7):29-37.
- [Google Scholar]
- Acute ischemic stroke and COVID-19: an analysis of 27 676 patients. Stroke. 2021;52(3):905-912.
- [Google Scholar]






