Translate this page into:
Neurology-Psychiatry Interface: Uncommon Presentation of Moyamoya Disease
Shipra Singh, MD Room No. 27, Psychiatry OPD, Dr. R.M.L. Hospital and PGIMER, Delhi India ssomvanshi27@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Moyamoya disease (MMD) is a rare arteriopathy associated with cerebral ischemia, due to stenosis or occlusion of the internal carotid artery and its branches and primarily presenting with stroke. However, neuropsychiatric symptoms such as acute psychosis, manic symptoms, attention deficits, and behavioral problems are reported in relation to MMD. We describe here a case of an adult female, who presented with headache, easy irritability, and suspiciousness against family members, inability to identify familiar objects and faces, and inability to perform activities easily done earlier. This case appears informative as the presence and excessive importance given to behavioral symptoms lead to substantial delay in her diagnosis.
Keywords
moyamoya disease
psychosis
vascular headache
Introduction
Moyamoya disease (MMD) is a rare cause of stroke, characterized by progressive stenosis of the terminal parts of the bilateral internal carotid artery (ICA) and the proximal trunks of the anterior cerebral artery (ACA) and middle cerebral artery (MCA). Subsequently, there is a development of dilated basal and cortical perforating arteries representing compensatory mechanisms for the reduced cerebral blood flow or the aberrant active neovascularization before the vascular occlusion, appearing as “puff of smoke” on neuroimaging.1 The most common acute presentations in this population are ischemic stroke, in the setting of large-vessel stenosis, and hemorrhagic stroke, typically involving friable collateral vessels.2
Behavioral and psychiatric manifestations are rather uncommon in MMD, either in the presence or absence of symptoms suggestive of cerebrovascular accident, and are mostly reported as isolated cases. Taksande et al reported in a patient of MMD, symptoms of headache, loss of interest in surroundings, and intermittent alteration in the mood,3 whereas in another case, manic symptoms were reported in addition to facial palsy and other neurological signs.4 Mohapatra and Sahoo reported behavioral symptoms such as hyperactivity and inattention with focal seizures.5 Considering psychotic symptoms with MMD, a case of acute transient psychosis and another with predominant delusion, hallucination, fatuous affect, and occasional disinhibited behavior with marked sensitivity to extrapyramidal symptoms have been described.6 7 We here present a case with delusion of persecution and agnosia and apraxia without any sensorimotor symptoms, which lead to a substantial delay in diagnosis and prompted detailed evaluation.
Case Report
A 22-year-old female patient presented with a history of persistent and severe headache in the parieto-temporo-occipital region, occurring nearly daily, lasting for half an hour to 2 to 3 hour, not associated with aura, nausea, vomiting, neck pain, lacrimation, photophobia, or phonophobia for the past 3 years, and the quality had remained consistent all these years. After 3 months, she was noticed gradually of not doing routine household chores, not maintaining appropriate grooming, easy irritability, and suspiciousness toward male members at in-law's place. Due to these reasons, the husband had left her at her maternal home 1 year back. She was seen by multiple physicians and psychiatrists in this duration, and based on the last prescription, she was taking tablet olanzapine 20 mg, tablet haloperidol 20 mg, and tablet trihexyphenidyl 2 mg for the last 4 months but had perceived no improvement.
The patient was admitted for detailed evaluation and diagnostic clarification. On history, it was found that the patient along with headache had inability to identify known objects (she specifically mentioned fruits and vegetables; as a result, she had difficulty in preparing the meals), difficulty in identifying the correct side of clothes, accessories, and other things (resulting in her inadequate grooming), and difficulty in using objects, the usage of which was known to her earlier. She even had problems in identifying familiar people and would often misidentify them. She was suspicious toward the male members of the family and said that the brother-in-law has approached her inappropriately. Family members were unable to understand her problem, which lead to interpersonal conflicts, and she would become irritable and on an occasion had hit the mother-in-law. There was no significant medical or family history. The patient was an average built, with average body mass index with clear consciousness and normal general physical examination. On neurological examination, sensory and motor system, reflexes, and cerebellum were found normal. However, errors were noticed in the higher mental system examination. Neuropsychological assessment (NIMHANS Neuropsychological Battery and Mukundan battery) revealed the following findings:
1. Temporal lobe: Dysfunction in visual integration, verbal and visual learning and memory, and test of comprehension.
2. Parietal lobe: dysfunction in visuospatial perception, visuoconstructive ability, ideomotor apraxia, constructional apraxia, spatial apraxia, visual recognition, reading, writing, and arithmetic.
3. Occipital lobe: dysfunction in visual object agnosia, color agnosia, asteregnosis, and prosopagnosia.
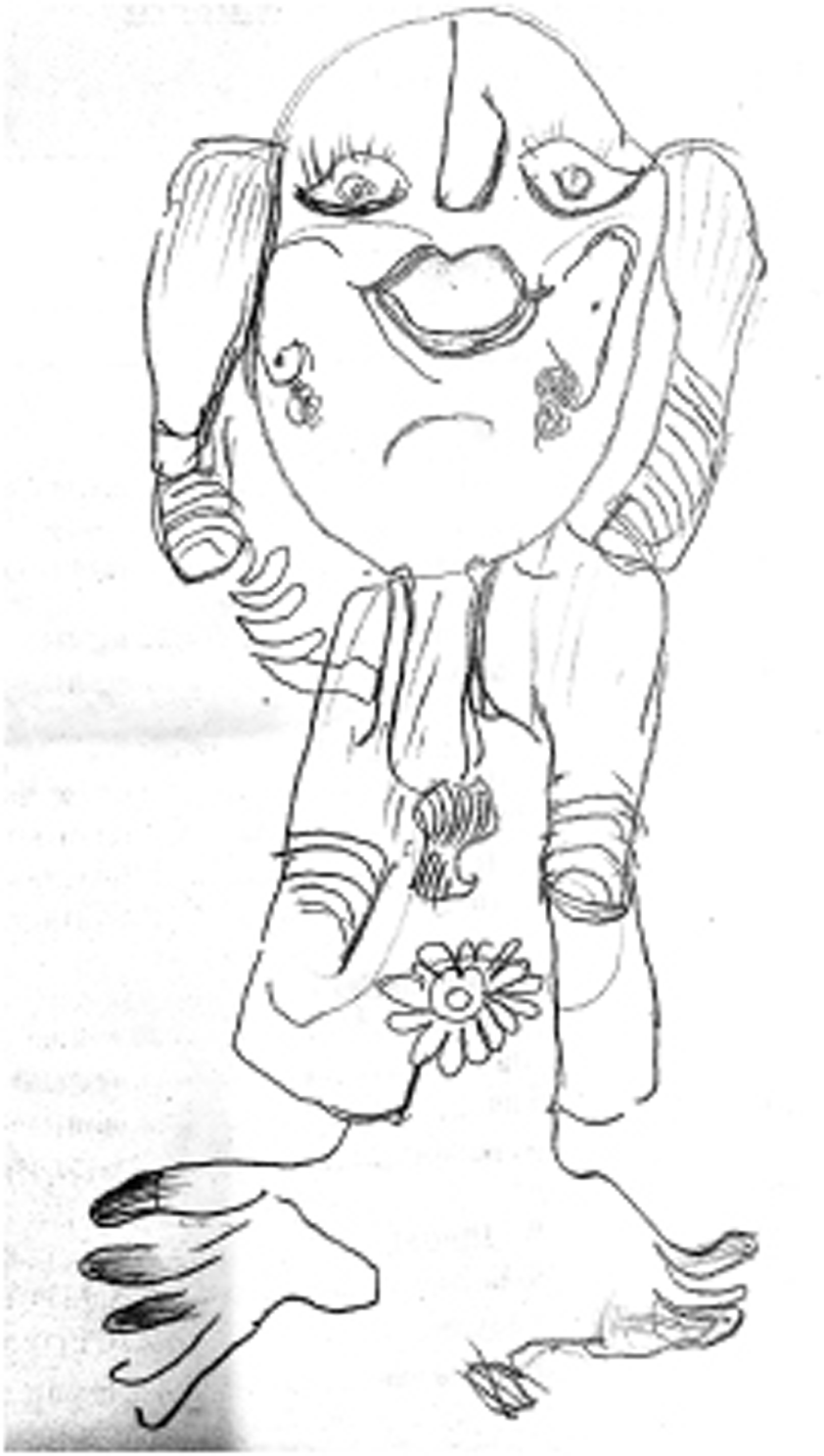
Based on this, computed tomography brain was done, which showed hypodense lesion in the left parieto-temporo-occipital region suggestive of infarct (Fig. 1). Investigations were done to explore the cause of such massive infarct, which included blood sugar, lipid profile, serum homocysteine, coagulation profile, and electrocardiography. In addition, her complete blood count including erythrocyte sedimentation rate, liver and kidney function test, and thyroid function test was done. All these parameters were within normal limits. Her Draw-a-Person test sketch is shown in Fig. 2. Neurology opinion was sought and magnetic resonance angiography (MRA) was advised which showed occlusion of distal ICA, ACA, and MCA with “puff of smoke” appearance, which is classical of MMD.

-
Fig. 1 Computed tomography brain showing the infarct.
Fig. 1 Computed tomography brain showing the infarct.
-
Fig. 2
Patient’s drawing in “Draw A Person Test’.
Fig. 2 Patient’s drawing in “Draw A Person Test’.
The patient's ongoing psychiatric medications were stopped. Statins and antiplatelet drugs were initiated as advised by the neurologist. The patient's family members were educated about the illness and advised to follow-up in the neurology department and occupational therapy department. However, the patient's follow-up could not be tracked.
Discussion
MMD commonly presents as stroke, transient ischemic attack, seizure, headache, or movement disorders.2 However, there are few reports of neuropsychiatric manifestations in association with MMD with or without prominent symptoms suggestive of cardiovascular accidents. These are isolated cases of manic symptoms; behavioral disorders including hyperactivity, inattention, easy distractibility, inattention, over-talkativeness, poor academic performance, forgetfulness in daily activities, irritability, stubbornness, emotional lability, and temper tantrums; manic symptoms; and cognitive issues.3 4 5 6 7 8 Psychotic symptom description in context to MMD is scarce. Klasen et al reported the presentation of a 12-year-old boy who presented with acute-onset verbosity, persecutor beliefs, and auditory hallucinations, with no physical or neurological abnormalities. On radiological investigations, left-sided abnormalities were noticed. He responded to antipsychotics which were continued for 3 months, and the boy was having normal functioning till 1-year follow-up.6 The second case describes a 23-year-old male with diagnosis of schizophrenia having multiple episodes and increased susceptibility to develop extrapyramidal symptoms with antipsychotics. No apparent neurological deficit was observed; however, he revealed significant difficulties on high-level attention, reasoning, and problem-solving tasks on neuropsychological assessment. MRA showed flow void of the predominantly posterior cerebral artery. The patient was discharged on tablet risperidone with partial symptom improvement.7
Diagnosis in cases where presentation is mostly neuropsychiatric is often complicated and can be easily missed—due to the rarity of the disorder; second, due to rarity of neuropsychiatric symptoms in the disease; and third, due to much importance given to behavioral symptoms by the family members. MMD might be the primary pathology in such cases or it might just be coexistent with psychosis. Yet, it suggests that atypical presentations or nonresponse to treatment in psychiatry often mandates for detailed assessment and excluding organic pathology.
Conflict of Interest
None declared.
Funding None.
References
- Moyamoya: epidemiology, presentation, and diagnosis. Neurosurg Clin N Am. 2010;21(3):543-551.
- [Google Scholar]
- Mood disorder in association with moyamoya disease. Psychiatry Clin Neurosci. 2012;66(2):163-164.
- [Google Scholar]
- Neuropsychiatric manifestations in a child with moyamoya disease. J Neurosci Rural Pract. 2016;7(2):331-332.
- [Google Scholar]
- Moyamoya disease in a 12-year-old Caucasian boy presenting with acute transient psychosis. Eur Child Adolesc Psychiatry. 1999;8(2):149-153.
- [Google Scholar]
- Moyamoya disease in a patient with schizophrenia. J Int Neu-ropsychol Soc. 2003;9(5):806-810.
- [Google Scholar]
- Cognitive deficits presenting as psychiatric symptoms in a patient with Moyamoya disease. Psychol Rep. 2010;107(3):727-732.
- [Google Scholar]






