Translate this page into:
Neurodevelopmental assessment of children with congenital heart diseases using Trivandrum developmental screening chart
*Corresponding author: Punam Uke, Department of Pediatrics, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India. drukepunam@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Uke P, Gaikwad SB, Swarnkar K, Lamture V, Khartade P. Neurodevelopmental assessment of children with congenital heart diseases using Trivandrum developmental screening chart. J Neurosci Rural Pract 2023;14:692-7.
Abstract
Objectives:
Congenital heart diseases (CHDs) are one of the most important congenital anomalies in children which have high-risk for neurodevelopment delay. This study was conducted to determine the proportion of developmental delay in children with CHD and comparison of delay between acyanotic and cyanotic heart diseases in children.
Materials and Methods:
A cross-sectional study was conducted on children admitted in pediatric ward of rural hospital from 6 month to 6 years of age who are diagnosed with CHD by 2D ECHO and further classified into acyanotic congenital heart disease (ACHD) and cyanotic congenital heart disease (CCHD). Neurodevelopmental assessment was done using Trivandrum development screening chart (TDSC).
Results:
Out of total 50 children in study population, 24 children had TDSC delay, distribution as 11 (22%) ACHD and 13 (26%) CCHD. Out of 24 children in the age group of 0–3 years, 13 (54.2%) were ACHD and 11 (45.8%) were CCHD. Out of 26 children in the age group of 3–6 years, 15 (57.7%) were ACHD and 11 (42.3%) were CCHD. Among different ACHD included in the study population (0–3 years) children with ventricular septal defect (VSD) were maximum (n = 5) next in the decreasing order was atrial septal defect (ASD) (n = 3). ACHD included in the study population (3–6 years) children with VSD was maximum (n = 6) next in the order was ASD (n = 4). Proportion of delay in children with ACHD was 22% as compared to 26% in children with CCHD.
Conclusion:
There is a high proportion of neurodevelopmental delay in children with CHD which can be detected using TDSC which is a simple screening tool and can be used by any health-care professional without training for the assessment of neurodevelopmental outcome in these children. Delay was more in children with CCHD than ACHD.
Keywords
Congenital heart disease
Developmental delay
Trivandrum development screening chart screening
Acyanotic congenital heart disease
Neurodevelopmental assessment
INTRODUCTION
Congenital heart disease (CHD) is one of the most common congenital anomalies in children.[1] Approximately twenty-eight percent of children are suffering from all major congenital anomalies of heart defects. Worldwide, the incidence of CHD varies from 4/1000 to 50/1000 live births.[2] The prevalence of CHD was found to be 9/1000 live births.[3] In recent years, a lot of advancement happened in the field of surgical techniques, intensive care management, cardiac catheterization techniques, and medical therapies for the treatment of patients with CHD causing significant improvement in mortality rates among children with complex CHD. These advances have a positive impact in the form of increased life expectancy in these children but also causing adverse neurological outcome such as developmental delay, difficulty in activities of daily living, poor school performance, and other neurodevelopmental disorders. Children with CHD have more chances for neurodevelopmental delay as compared to normal children due to impact of CHD on overall development of the child.[4] Neurodevelopmental delay in these children is attributed to various events in intrauterine life, surgery, or while growth such as poor perfusion, shock, acid base disturbances, and episodes of hypoxia. Moreover, these adverse events are more pronounced in children with cyanotic congenital heart disease (CCHD).
CHD causes hampering of brain maturation either due to reduced flow of blood to the brain or decreased oxygen content of blood. Improved survival of children with CHD as a result of advance techniques in the management in the recent years shift focus to the enhancement of neurodevelopmental outcome of these children which in long-term improve the quality of life of these children.[5] Regular follow-up to a health facility which focuses primarily on the evaluation of nutritional status, developmental assessment, and neurological examination of these children is of prime importance. These children have increased chances to suffer from malnutrition, delayed milestones (Development Quotient, DQ), and impaired Social Quotient which can be picked up early with regular follow-up.[6] American Heart Association recommends periodic evaluation in early years of life till adolescent years even if no concerned to children. CHD affects neurodevelopment which will have lifelong impact on overall outcome of the child. CHD causes adverse effects on all different domains of development these are gross motor, fine motor, language, cognitive, and social. As the child gets older specifically in school-going age, these adverse neurodevelopmental outcomes present in the form of difficulty in the organization of tasks, poor memory, non-coordination in activities requiring visuospatial skills, slow in mathematical calculations along with delayed language, and socio communication skills in these children as compared to peers of same age.[7] Many researches were done all over the world and studies found that neurodevelopmental delay is profound in children with CCHD than in acyanotic CHD (ACHD).[8] The present study was undertaken in view of paucity of studies on neurodevelopmental status and the proportion of developmental delay in patients with CHD in children. The objective of the study was to assess the proportion of developmental delay in patients with CHD using Trivandrum development screening chart (TDSC) and to compare the neurodevelopmental status in children with ACHD and CCHD.
MATERIALS AND METHODS
It is a cross-sectional study conducted at Acharya Vinoba Bhave Rural Hospital, Sawangi (Meghe) Maharashtra in the Pediatrics Department from December 2019 to May 2020 in children with age group 6 month–6 years who are diagnosed with CHD. Children diagnosed to have heart disease after confirming by performing 2D ECHO which further classifies them into ACHD and CCHD heart diseases depending on finding on 2D ECHO. A total of 50 children were included in the study, out of which 22 were CCHD and 28 were ACHD. Neurodevelopmental assessment was done using TDSC charts. Age group was divided into 0–3 years and 3–6 years, and screening was done in respective TDSC charts according to age. Child fail to achieve single parameter for that particular age in TDSC labeled as TDSC Delay. Care was taken to include items for testing hearing and visual functions.
Statistical analysis
Descriptive and inferential statistical analysis was done using STATA software (Stata10, Stata Corporation Texas, USA). Quantitative data were analyzed using mean, median, and standard deviation. Qualitative data were summarized using percentage and differences in proportion were compared by the Chi-square test. Differences between means were compared by unpaired student’s “t” test. P < 0.05 was considered statistically significant.
RESULTS
Fifty patients with diagnosed CHD with no known neurological deficit were included in our study. 24 children from 0 to 3 years, whereas 26 from 3 to 6 years were included in the study. Out of 24 children in the age group of 0–3 years, 13 (54.2%) were male and 11 (45.8%) were female. Out of 26 children in the age group of 3–6 years, 15 (57.7%) were male and 11 (42.3%) were female. Different types of ACHD in the study group 0–3 years and 3–6 years are shown in [Table 1]. Similarly, the different types of CCHD in study group 0–3 year and 3–6 year are shown in [Table 2]. Proportion of delay in children with ACHD was 22% as compared to 26% in children with CCHD. Hence, neurodevelopmental delay was more in children with CCHD as compared to ACHD as shown in [Table 3].
| Diagnosis of ACHD | Number of children (0–3 years) | Percentage of children | Number of children (3–6 years) | Percentage of children |
|---|---|---|---|---|
| VSD | 5 | 20.83 | 6 | 23.08 |
| ASD | 3 | 12.50 | 4 | 15.38 |
| PDA | 1 | 4.17 | 2 | 7.69 |
| ASD with PDA | 1 | 4.17 | 0 | 0 |
| ASD with VSD | 1 | 4.17 | 1 | 3.85 |
| PDA with VSD | 1 | 4.17 | 0 | 0 |
| VSD with ASD with PDA | 1 | 4.17 | 2 | 7.69 |
| Total | 13 | 54.17 | 15 | 57.69 |
ACHD: Acyanotic congenital heart disease, VSD: Ventricular septal defect, ASD: Atrial septal defect, PDA: Patent ductus arteriosus
| Diagnosis of CCHD | Number of children | Percentage of children | Number of children | Percentage of children |
|---|---|---|---|---|
| TOF | 5 | 20.83 | 5 | 19.23 |
| TGA | 2 | 8.33 | 2 | 7.69 |
| TAPVC | 2 | 8.33 | 2 | 7.69 |
| Tricuspid atresia | 1 | 4.17 | 1 | 3.85 |
| Ebstein anomaly | 1 | 4.17 | 1 | 3.85 |
| Total | 11 | 45.83 | 11 | 42.31 |
CCHD: Cyanotic congenital heart disease, TOF: Tetralogy of fallot, TGA: Transposition of great arteries, TAPVC: Total anomalous pulmonary venous connection
| Type of CHD | Delay (%) | No delay (%) | Total (%) |
|---|---|---|---|
| Acynotic | 11 (22) | 17 (34) | 28 (56) |
| Cyanotic | 13 (26) | 9 (18) | 22 (44) |
| Total | 24 (48) | 26 (52) | 50 (100) |
CHD: Congenital heart disease
Neurodevelopmental outcome in children in CHD in age group 0–3 years: the gross motor milestones [Figure 1], fine motor domain [Table 4], language domain milestones [Table 5], and social and adaptive domain milestones [Figure 2] achieved in children with CHD are delayed as compared to expected age of attainment according to TDSC chart. 13 children were having ACHD of them 4 (16.67%) had TDSC delay and 9 (37.50%) had no delay. 11 children of CCHD were studied of them 7 (29.17%) had TDSC delay and 4 (16.67%) had no delay. Out of 24 children, 11 (45.83%) children had TDSC delay and 13 (54.17%) had no delay with P value being 0.10.

- Gross motor milestones in children age 0–3 years using Trivandrum development screening chart.

- Social and adaptive domain milestones in children age 0–3 years using Trivandrum development screening chart.
| Milestones | Expected age of attainment (months) | Actual age of attainment (months) | Mean Difference | % Difference |
|---|---|---|---|---|
| Transfer objects hand to hand | 7 | 8.08 | 1.08 | 15.42 |
| Fine prehension pellet | 11 | 12.42 | 1.42 | 12.90 |
| Throws ball | 16.5 | 17.84 | 1.34 | 8.12 |
| Brush teeth with help | 32 | 34.25 | 2.25 | 7.03 |
TDSC: Trivandrum development screening chart
| Milestones | Expected age of attainment (months) | Actual age of attainment (months) | Mean difference | % Difference |
|---|---|---|---|---|
| Turns head to sound of bell or rattle | 5.5 | 5.89 | 0.39 | 7.09 |
| Says to words | 19 | 21 | 2 | 10.52 |
| Uses words for personal needs | 27 | 28.62 | 1.62 | 6 |
| Answers at least half understandable to others | 35 | 36 | 1 | 2.85 |
| Asks simple questions | 36 | 36 | 0 | 0 |
TDSC: Trivandrum development screening chart
Neurodevelopmental outcome in children in CHD in the age group 3–6 years: the gross motor milestones [Table 6], fine motor domain [Figure 3], language domain milestones [Figure 4], and social and adaptive domain milestones [Table 7] achieved in children with CHD are delayed as compared to the expected age of attainment according to TDSC chart.

- Fine motor domain milestones in children age 3–6 years using Trivandrum development screening chart.
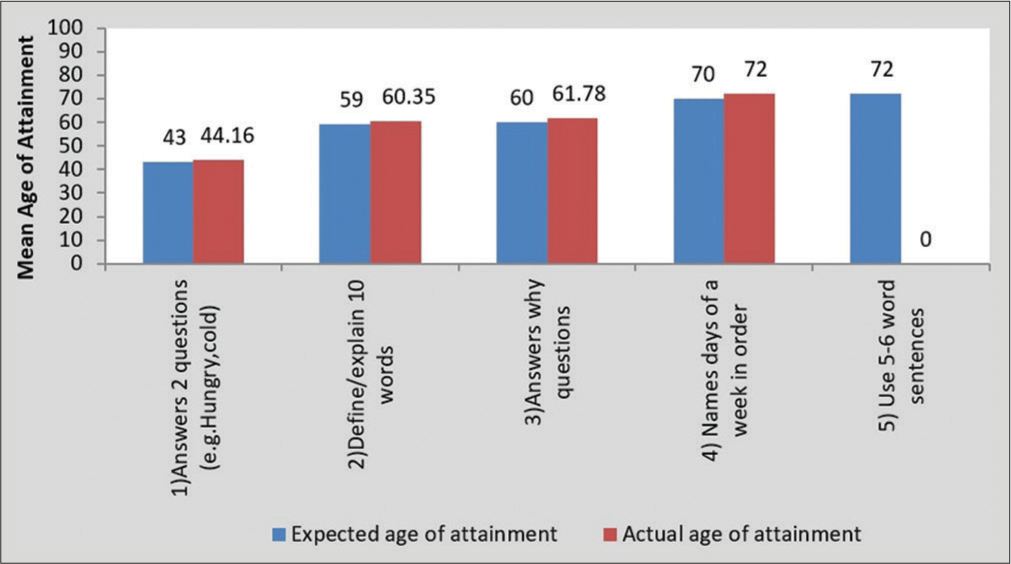
- Language domain milestones in children age 3–6 years using Trivandrum development screening chart.
| Milestones | Expected age of attainment (months) | Actual age of attainment (months) | Mean difference | % Difference |
|---|---|---|---|---|
| Broad jump (both legs) | 36 | 36.69 | 0.69 | 1.91 |
| Balance one foot one second | 40 | 41.30 | 1.3 | 3.25 |
| Hops continuously 3 steps | 52 | 53.35 | 1.35 | 2.59 |
| Heel to toe walk 4 consecutive steps | 60 | 62.14 | 2.14 | 3.56 |
TDSC: Trivandrum development screening chart
| Milestones | Expected age of attainment (months) | Actual age of attainment (months) | Mean difference | % Difference |
|---|---|---|---|---|
| Name one colour | 45 | 45.66 | 0.66 | 1.46 |
| Tells use of 2 objects (e.g. pencil, chair) | 45 | 46.33 | 1.33 | 2.95 |
| Concept of one (pick “I” from a group) | 46 | 47.41 | 1.41 | 3.06 |
| Plays near and talks with peers | 50 | 51.69 | 1.69 | 3.38 |
| Tells function of 3 body parts | 57 | 58.53 | 1.53 | 2.68 |
| Points to middle | 65 | 66.70 | 1.7 | 2.61 |
| Pick 5 objects from the group | 66 | 68.14 | 2.14 | 3.24 |
TDSC: Trivandrum development screening chart
15 children were having ACHD of then 7 (26.92%) had TDSC delay and 11 children of CCHD were studied of them 6 (23.08%) had TDSC delay. Out of total 50 children in study population, 24 children had TDSC delay, distribution as 11 (22%) ACHD, and 13 (26%) CCHD.
DISCUSSION
CHD is the one of the important causes of mortality in infants. Many studies were showing that children with CHD have more neurodevelopmental delays as compared to normal children.[9] The aim of our study was to study the neurodevelopmental outcome in children with CHD between 0 and 6 years with objectives of determining the prevalence of developmental delay in children with CHD and comparison of neurodevelopmental outcome in children with ACHD and CCHD. 400 cases were selected randomly from birth to 3 years of age who attended the Well baby clinic in a study conducted by Dewangan et al.[10] and Chauhan et al.[11] In another study done by Kishore et al.,[12] it was 100 between 0 and 3 years. In our study, sample size was much smaller than above studies as it was done during COVID pandemic period. In a study conducted on patients with pediatric, CHD by Ratanachu-Ek and Pongdara[13] delay was more pronounced in female as compared to male with ratio of 0.7: 1 which was similar to another study by Mitchell et al.[14] study including 48 cases with CHD with the M: F ratio of 0.9:1. In our study, M: F was 1.2:1. Lata et al.[6] found that the motor development was delayed in 75% children with cyanotic heart disease and 35.3% with ACHD (P = 0.001). The mean DQ in the motor domain was significantly lower in the cyanotic group than acyanotic group (P = 0.048). A study was conducted by Weinberg et al.[15] using Denver developmental screening test (DDST) found that, out of the 64 children, 64% children were developmentally normal and the remaining were classified as abnormal, questionable, or untestable. Yilmaz et al.[16] studied 75 children of CHD using Japanese Denver developmental screening test (JDDST) and observed that 18.7% of 75 infants had developmental delay in gross motor domain, and 4.0% in the language domain and fine motor-adaptive domain, respectively. The children with heart disease had more “suspicious” and “suspect/ abnormal” ratings as compared to normal children in a study conducted by Mari et al. using DDST.[17] Reduced mental level in approximately 10% along with at least one neurodevelopmental disorder in 25% children with CHD was found by Ozmen et al. where they used Bayley Development Scale-III and DDST-II.[18]
In our study, large age group was taken as study population as compared to many other studies. Male-to-female ratio in our study was 1.2:1. We divide our study group into two groups that is 0–3 years and 3–6 years. 24 children were of 0–3 years, of which 13 were ACHD and 11 were CCHD. Neurological delay was present in children with CHD as plotted on TDSC chart in all 4 developmental domains, i.e., gross motor, fine motor, language, and social adaptive. In comparison of neurodevelopmental outcome in ACHD and CCHD, children with CCHD were found to have more delay compared to ACHD. 4 (16.67%) children had delay and 9 (37.50%) had no delay in ACHD. 7 (29.17%) children had delay and 4 (16.67%) had no delay in CCHD.
In the second group, i.e., 3–6 years 26 children were included, of which 15 were ACHD and 11 were CCHD. Neurological delay was present in children with CHD as plotted on TDSC chart in all 4 developmental domains, i.e., gross motor, fine motor, language, and social adaptive. In our study of comparison of neurodevelopmental outcome in ACHD and CCHD, children with CCHD were found to have more delay as compared to children with ACHD. 7 (26.92%) children had delay and 8 (30.77%) had no delay in ACHD. 6 (23.08%) children had delay and 5 (19.23%) had no delay in CCHD. Proportion of delay in children with ACHD was 22% as compared to 26% in children with CCHD. Hence, neurodevelopmental delay was more in children with CCHD as compared to ACHD.
CONCLUSION
There is a high proportion of neurodevelopmental delay in children with CHD and TDSC is a simple screening tool which does not need special training for administration which helps to assess neurodevelopmental outcome in these children. Neurodevelopmental delay was present in all four developmental domains, i.e., gross motor, fine motor, language, and social adaptive. The proportion of developmental delay is more in children with CCHD as compared to ACHD. Screening of children with simple tool-like TDSC help to pick children with developmental delay at the earliest, especially from rural areas where medical facilities are very limited which will help children for early intervention and in long term lead to good neurodevelopmental outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Congenital heart defects in Europe: Prevalence and perinatal mortality, 2000 to 2005. Circulation. 2011;123:841-9.
- [CrossRef] [PubMed] [Google Scholar]
- Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241-7.
- [CrossRef] [PubMed] [Google Scholar]
- Heart disease and stroke statistics-2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Sub committee. Circulation. 2009;119:480-6.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital heart disease in India: A status report. Indian Pediatr. 2018;55:1075-82.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term and developmental outcomes of children with complex congenital heart disease. Clin Perinatol. 2005;32:1043-57, xi
- [CrossRef] [PubMed] [Google Scholar]
- Neurodevelopmental status of children aged 6-30 months with congenital heart disease. Indian Pediatr. 2015;52:957-60.
- [CrossRef] [PubMed] [Google Scholar]
- Neurodevelopmental outcomes in children with congenital heart disease: Evaluation and management: A scientific statement from the American Heart Association. Circulation. 2012;126:1143-72.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological evaluation and intelligence testing in the child with operated congenital heart disease. Ann Thorac Surg. 2000;70:575-81.
- [CrossRef] [PubMed] [Google Scholar]
- Neurodevelopmental abnormalities and congenital heart disease: Insights into altered brain maturation. Circ Res. 2017;120:960-77.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Trivandrum developmental screening charts against the standard Denver development screening test in children between 0-3 years. Int J Contemp Pediatr. 2020;7:2142-5.
- [CrossRef] [Google Scholar]
- Development and validation of Trivandrum developmental screening chart for children 0-3 years by TDSC. New Indian J Paediatr. 2016;5:137-43.
- [Google Scholar]
- To identify clinical utility of TDSC in screening of developmental delay in children (0-3 yrs.) as compared to DDST. J Evid Based Med Health Care. 2019;6:2146-50.
- [CrossRef] [Google Scholar]
- Nutritional status of pediatric patients with congenital heart disease: Pre-and post-cardiac surgery. J Med Assoc Thai. 2011;94(Suppl 3):S133-7.
- [Google Scholar]
- Nutritional status of children with congenital heart disease. Br Heart J. 1995;73:277-83.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental screening of children diagnosed with congenital heart defects. Clin Pediatr (Phila). 2001;40:497-501.
- [CrossRef] [PubMed] [Google Scholar]
- Neurodevelopmental evaluation of children with cyanotic congenital heart disease. Minerva Pediatr. 2018;70:365-70.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital heart disease and impacts on child development. Braz J Cardiovasc Surg. 2016;31:31-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of neurodevelopment and factors affecting it in children with acyanotic congenital cardiac disease. Iran J Pediatr. 2016;26:e3278.
- [CrossRef] [PubMed] [Google Scholar]







