Translate this page into:
Methodology for the early identification of neurodevelopmental disorders in the primary and preschool children in rural India by applying intervention module developed for teachers
*Corresponding author: Shantaraman Kalyanaraman, Department of Pathology, Tirunelveli Medical College, Tirunelveli, Tamil Nadu, India. shantaraman_kal@tvmc.ac.in
-
Received: ,
Accepted: ,
How to cite this article: Esakki B, Kandasamy S, Mahadevan R, Subbiah P, Jayaraman Y, Gopal M, et al. Methodology for the early identification of neurodevelopmental disorders in the primary and preschool children in rural India by applying intervention module developed for teachers. J Neurosci Rural Pract 2023;14:165-9.
Abstract
Objective:
Neurodevelopmental disorders NDD are neurologic processing problems that interfere with learning in children. Primary and preschool teachers who are essential links in public health reach out to such children do not receive any formal training to identify these disorders. Hence, a primary and preschool level intervention addressing the issue is proposed.
Materials and Methods:
Primary and preschool teachers of government and government-aided schools and Anganwadi/preschools in the Model Rural Health Research Unit Tirunelveli field practice area will be assigned into two groups. The training module will be developed and validated using neurodevelopmental screening tool (NDST). Before identifying the students using the NDST, the teachers in Group A will get training using the module. Group B is the control group, in which untrained teachers administer the NDST to the children and then will be trained. Neurologists will assess the same children over 1 year.
Results:
The effectiveness of teacher training for the early detection of children with NDD will be assessed. Thus, the validity of the screening for NDD by the teachers will be estimated.
Conclusion:
If successful, the module can be incorporated into the Rashtriya Bal Swasthya Karyakram program of India for the early identification of children with NDD.
Keywords
Learning disabilities
Child development disorders
Attention-deficit/hyperactivity disorder
Training teachers
Elementary school teachers
Preschool-teachers
Early intervention
BACKGROUND AND RATIONALE
Cognition is the mental processes such as thinking, learning, remembering, abstraction, judgement, problem-solving, language, imagination, perception, planning, and carrying out plans that help us learn about ourselves and our surroundings. Neurodevelopmental disorders NDD are neurological processing problems that make it hard to learn basic skills such as reading or writing.[1] Most NDD is classified by the Diagnostic and Statistical Manual V, the most recent classification for cognitive and learning deficits.[2] NDD includes intellectual disability disorders, communication disorders, autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), specific learning disorders, motor disorders, and tic disorders.
According to the 2011 Indian census, 1.1% of 0–4 years old and 1.5% of 5–9 years old were disabled.[3] The prevalence of NDD in India ranges between 7.5% and 18.5%.[4] NDD constitutes a significant cause of learning disabilities (LDs) in the primary school students. About 5% of all students in United States public schools have LD.[5]
India’s reported prevalence of LD ranges from 1.6% to 15%, depending on the region, age group studied, and methodologies used.[6-8] Studies conducted in South India revealed a frequency of 15.17%, including 12.5% with dysgraphia, 11.2% with dyslexia, and 10.5% with dyscalculia.[9] Low maternal education, very low birth weight, and poor APGAR score are associated with LD.[10-12] ADHD prevalence ranges from 1% to 20% worldwide[13] and 1.6 % to 17.9% in India.[7,14-18] Approximately 4.1% of primary school children in Mauritius have a tic disorder, predominantly boys.[19] The prevalence of ASD varies from 0.7% to 48% globally.[20-22]
NDD has psychological, social, and economic effects on the child, family, and society. This is worsened by parents in rural regions who are uneducated. A “cognitive watch” strategy must be implemented to prevent cognitive impairments and LD in young children. Screening for child health and promoting early intervention services will reduce the severity of the disability, improve the quality of life, and give everyone the chance to reach their full potential.
Teachers, who are an essential link in the public health system for reaching out to primary school children, receive no formal training to identify these conditions. Their knowledge, attitudes, and practices regarding identifying children with NDD need assessment.
Similarly, a basic training module for teachers in identifying these children is essential and lacking. The National Rural Health Mission of India started Rashtriya Bal Swasthya Karyakram (RBSK) to identify and intervene in congenital defects, disabilities, disorders, and diseases in school children. [23,24] Training teachers in identifying NDD in preschool and primary school children would assist the RBSK team in identifying intervention targets and managing the unique needs of these children. Studies on the role of teachers in assisting the identification of NDD are sparse in this part of the country. Capacity building of teachers and utilizing their services for case identification in NDD will be beneficial. Hence, we designed the study to develop and validate a training module (intervention) for pre- and primary school teachers to identify children with NDD. The sensitivity and specificity of teachers in identifying children with NDD compared to that of the neurologists will be assessed. Also, the prevalence of NDD among pre and primary school children will be estimated.
METHODOLOGY
Study design
This study design is an quasi–experimental study.
Study setting
Department of Health Research, Government of India, has established one of the Model Rural Health Research Unit (MRHRU) in Tirunelveli District, South India. This unit is linked to Tirunelveli Medical College and is mentored by the National Institute of Epidemiology, Chennai. The field practice area of this unit is the study setting with 30 government and government-aided primary schools, 46 Anganwadi Centres (AWC)/preschools, 2892 children, and 107 primary and 46 preschool teachers.
Inclusion criteria
All primary (107) and preschool teachers (46) from government and government-aided primary schools and AWCs in the study setting who are willing to participate will be included in the study. In addition, all 2892 children enrolled in the same schools with parental permission will be included in the study.
Exclusion criteria
We exclude teachers on transfer, on a 3-month leave such as maternity leave, or teaching in private schools and children with severe NDD who cannot attend school.
Methods
We will conduct the study in two phases. In the first phase, we will develop and validate a training module and train the teachers as per the groups assigned to identify the children with NDD over 2 months. In the second phase, the neurologists will assess the children over 1 year.
To train the teachers, the investigators will develop a module in the vernacular (Tamil), based on the neurodevelopmental screening tool (NDST) of the National Institute of Epidemiology (NIE). The training module will comprise of a booklet with an introduction, clinical features of NDD, identification using the NDST, early detection advantages, and teachers’ directions on completing the NDST. Tirunelveli Medical College and NIE will peer-review and validate the module.
After obtaining administrative approval from the District Chief Education Officer and Project Officer of Integrated Child Development Services, we will initiate the study. Line listing of the government and government-aided primary schools and AWCs, teachers, and children will be done.
We randomly assign the teachers into two groups: before identifying the students using the NDST, the teachers in Group A will get training using the module. Group B is the control group, in which untrained teachers administer the NDST to the children and then will be trained. The scheduling of training sessions will consider the teachers’ feasibility. The teachers will be communicated, and written informed consent will be obtained.
The principal investigator (neurologist) will conduct a 1-day interactive training session at Model Rural Health Research Unit for Group A teachers utilizing a power point presentation based on the module and clarify their queries. Pre- and post-session questionnaires will be collected. The training module booklet, informed written consent forms for parents, and NDST assessment tools will be provided to the teachers to identify children with NDD. After the session, Group A teachers will screen each child under their direct supervision over 2 months. Meanwhile, the Group B teachers will assess the children under supervision for 2 months using the same NDST without training. At the end of 2 months, the investigator will train Group B teachers using the same module as Group A. The investigators will randomly supervise teachers in both groups to see how they use NDST.
After 2 months of screening by teachers, investigators will examine children for NDD over 1 year at the respective schools and Anganwadi centers. Children with NDD will be referred to Tirunelveli Medical College [Flow Charts 1 and 2].

- Proposed activities.
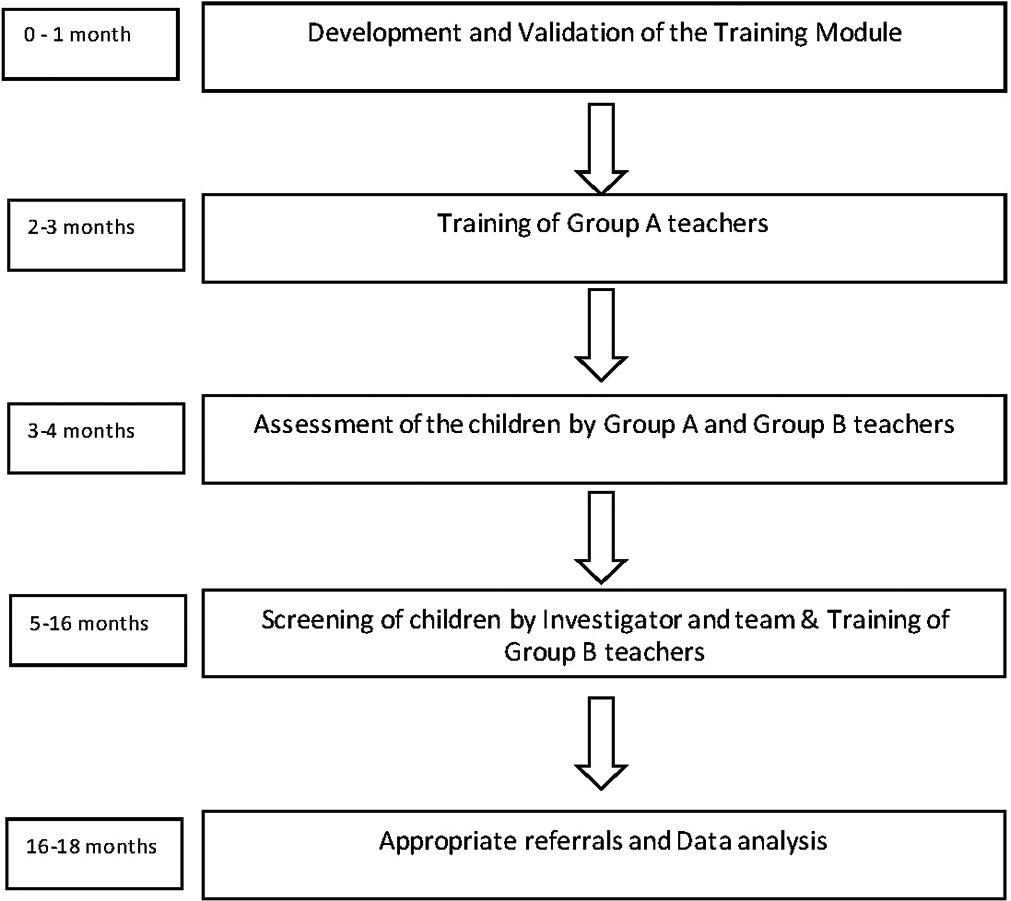
- Time line of proposed activities.
All ethical guidelines will be followed at each phase of the study. As indicated, we will get administrative approval. Teachers’ written informed consent will be obtained. The teachers will get the parents’ written informed consent before assessing the children for NDD. As the children are vulnerable, the study permits timely and appropriate rehabilitation referrals.
Data collection and analysis
The data will be captured using the individual paper-based NDST forms filled by the teachers and the investigators. The data will be entered in a Microsoft Excel worksheet and analyzed using SPSS software version 23.0. The prevalence of NDD among pre and primary school children in the study area will be estimated. Pre- and post-test scores will assess the teachers’ existing knowledge of NDD and the same imparted by the intervention, respectively. The significance of the session on imparting knowledge to teachers will be calculated by paired student t-test.
Outcome
The study is the first of its kind to assess the prevalence of NDD among rural India’s pre- and primary school children. As a result of the study, the effectiveness of teacher training for early detection of NDD will be assessed. Thus, the validity of the screening for NDD by the teachers as a result of the training will be estimated.
Implications
We propose the study as a potentially cost-effective strategy for the timely identification of children with NDD. Early diagnosis of NDD will aid in determining the most appropriate disorder-specific intervention and rehabilitation for children. With the help of trained teachers, the parents will be informed and made aware of the problems their children face due to NDD.
Thus, we have the opportunity to channel children based on their strengths and limitations, which increase the children’s well-being and has a positive effect on the family and society.
Limitations
Children with severe NDD who cannot attend school will represent a limitation. Since only government and government-aided schools are included in the study, the results may not be applicable beyond the setting.
CONCLUSION
The effectiveness of teacher training for the early detection of children with NDD will be assessed. If successful, the module can be incorporated into the Rashtriya Bal Swasthya Karyakram (RBSK) program of India for the early identification of children with NDD.
Acknowledgments
We are grateful to Medical Social Workers – Mr. V. Lakshmikandhan and Miss. A. Santhiya Devi, Mr. Mobein, Statistician Miss. Maryam Jamila Sibqathula and Mrs. Sankareswari Assistant (Admin), MRHRU, Kallur, Tirunelveli for their support.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) (5th ed). Washington: American Psychiatric Association; 2013.
- [CrossRef] [Google Scholar]
- Office of the Registrar General and Census Commissioner of India. 2011. New Delhi: Ministry of Home Affairs, Government of India; Available from: https://www.censusindia.gov.in/2011census/disability_data/India/C_20-India.xls [Last accessed on 2021 Dec 28]
- [Google Scholar]
- Neurodevelopmental disorders in children aged 2-9 years: Population-based burden estimates across five regions in India. PLoS Med. 2018;15:e1002615.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and patterns of learning disabilities in school children. Indian J Pediatr. 2016;83:300-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and pattern of learning disabilities in school children. Delhi Psychiatry J. 2013;6:386-90.
- [Google Scholar]
- Prevalence of attention deficit hyperactivity disorder in primary school children. Indian J Psychiatry. 2013;55:338-42.
- [CrossRef] [PubMed] [Google Scholar]
- An epidemiological study of child and adolescent psychiatric disorders in urban and rural areas of Banglore, India. Indian J Med Res. 2005;122:67-79.
- [Google Scholar]
- Prevalence of specific learning disabilities among primary school children in a South Indian city. Indian J Pediatr. 2012;79:342-7.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of early risk factors for learning disabilities. J Early Interv. 2001;24:193-206.
- [CrossRef] [Google Scholar]
- The effects of biological and social risk factors on special education placement: Birth weight and maternal education as an example. Res Dev Disabil. 1998;19:281-94.
- [CrossRef] [PubMed] [Google Scholar]
- Obstetric factors and different causes of special educational need: Retrospective cohort study of 407503 schoolchildren. BJOG. 2013;120:297-307.
- [CrossRef] [PubMed] [Google Scholar]
- The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942-8.
- [CrossRef] [PubMed] [Google Scholar]
- A study of comorbidities in attention deficit hyperactivity disorder: A retrospective analysis of case records. AP J Psychol Med. 2014;15:206-10.
- [Google Scholar]
- Prevalence of attention deficit hyperactivity disorder in an urban school of a developing country. Int J Res Med Sci. 2015;3:3759-62.
- [CrossRef] [Google Scholar]
- Prevalence of attention deficit hyperactivity disorder among urban school children. Int J Contemp Pediatr. 2016;3:240-2.
- [CrossRef] [Google Scholar]
- Attention-deficit hyperactive disorder among primary school children in menoufia governorate, Egypt. Int J Family Med. 2014;2014:257369.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and correlates of attention deficit hyperactive disorder (ADHD) risk factors among school children in a rural area of North India. J Family Med Prim Care. 2020;9:115-8.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of tic disorder in primary school children in an electoral district of Mauritius. J U S China Med Sci. 2016;13:13-8.
- [CrossRef] [Google Scholar]
- Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics. 2011;127:1034-42.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and characteristics of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65:1-23.
- [CrossRef] [Google Scholar]
- Child disability screening, nutrition, and early learning in 18 countries with low and middle incomes: Data from the third round of UNICEF's multiple indicator cluster survey (2005-06) Lancet. 2009;374:1831-9.
- [CrossRef] [PubMed] [Google Scholar]
- National Health Programs of India (11th ed). New Delhi: Century Publishers; 2014. p. :661-70.
- [Google Scholar]
- Operational guidelines Rastriya Bal Swasthya Karyakram (RBSK) Child Health Screening and Intervention Services under NRHM New Delhi: Ministry of Health and Family welfare; 2013.
- [Google Scholar]






