Translate this page into:
Neurobrucellosis Presenting as Acute Psychosis
Address for correspondence: Dr. Irfan Ahmad Shah, Residential Block, Government Psychiatric Diseases Hospital, Srinagar - 190 003, Jammu and Kashmir, India. E-mail: irfanskims@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 45-year-old female without any past or family history of psychiatric illness presented to the emergency department with complaints of abnormal behavior, irrelevant talking, restlessness, episodic crying, and decreased sleep of 2-day duration. On detailed interview, the attendants gave a history of an intermittent headache of 6-month duration and hearing impairment of 4-month duration. On investigation, her cerebrospinal fluid was reactive, and brucella titers were positive. She received appropriate treatment for 6 months and a short course of antipsychotics. Her symptoms settled, but she had persistent hearing loss. Psychosis as well as hearing loss is a very rare presentation of brucellosis. The case highlights the importance of considering neurobrucellosis as a differential diagnosis in patients with any unexplained neuropsychiatric symptoms such as acute psychosis or hearing loss.
Keywords
Brucella meningitis
brucella psychosis
neurobrucellosis
sensorineural hearing loss.
INTRODUCTION
Brucellosis is a zoonotic infectious disease, which can be transmitted to humans from infected animals mainly after consumption of unpasteurized milk and milk products. It can also be transmitted after direct contact with infected animals through inhalation, especially to slaughterhouse workers, farmers, and laboratory workers. Central nervous system involvement is rare but may cause serious clinical manifestations. Neurobrucellosis occurs in < 5% of patients. Subacute and chronic meningoencephalitis has been described as the most common neurologic presentations of neurobrucellosis.[1] Sensorineural hearing loss is an uncommon manifestation of brucellosis.[2] Psychosis as a presentation of neurobrucellosis is a much rarer condition. There are only a few previous reports of brucella psychosis in the literature. Herein, we report a case of neurobrucellosis presenting with acute psychosis and bilateral sensorineural hearing loss.
CASE REPORT
A 45-year-old female presented to the emergency department with complaints of abnormal behavior, irrelevant talking, and wandering away from bed of 2-day duration. There was also a history of restlessness, impulsivity, and episodic crying. There was also a history of decreased sleep and use of abusive language. There was no history of similar illness in the past. Family history of any such illness was not present, nor was any history of drug intake. On detailed interview, the attendants give a history of intermittent headache for the past 6 months. There was also a history of decreased hearing for the past 4 months, which was evaluated by a local practitioner and thought to be noise-induced high-frequency loss. Attendants also gave a history of exposure to cattle at home. On general physical examination, patient was afebrile, conscious, and oriented to time but not to place or person. Glasgow coma scale score was 15/15. Her speech was slurred and incoherent. Nervous system examination only revealed features of bilateral sensorineural type hearing loss which was later confirmed by pure-tone audiometry. There was no neck stiffness. Mental status examination revealed features of acute psychosis with delusions, hallucinations, suspiciousness, and agitation. Investigations revealed a normal hemogram, kidney, and liver function tests. Contrast magnetic resonance imaging of brain showed mild meningeal enhancement [Figure 1]. Lumbar puncture was done which revealed a reactive cerebrospinal fluid (CSF) with lymphocytic pleocytosis (220 cells, 78% lymphocytes), protein of 95 mg/dl, and glucose of 29 mg/dl. CSF was negative for gram staining, fungal stain, and acid-fast bacilli. Routine cultures were sterile and adenine deaminase was 04 IU/L. PCR was negative for tuberculosis. Brucella agglutination test of CSF was done which was positive with titers of 1: 320. The diagnosis of neurobrucellosis was proposed and she was started on injection ceftriaxone, oral doxycycline, and rifampicin. Psychiatric consultation was sought and the patient was started on olanzapine 10 mg once daily. Her symptoms of psychosis improved but would initially recur on omitting the antipsychotic. After 2 weeks, the psychosis resolved and olanzapine was slowly tapered off. At 3 months, she was doing well but hearing loss persisted. She received neurobrucellosis treatment for 6 months.
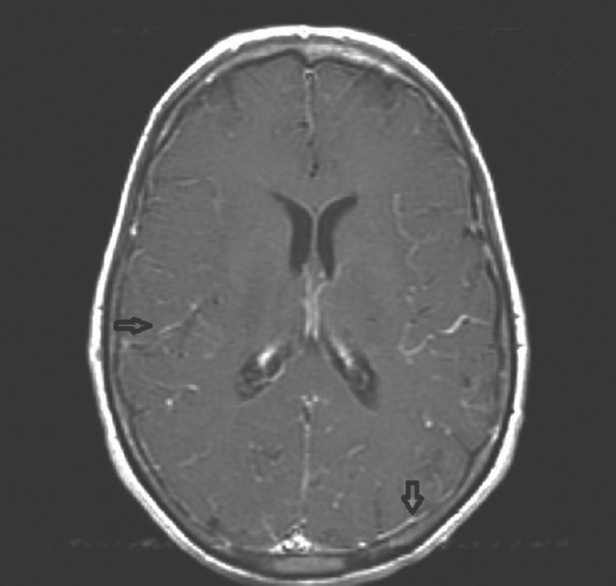
- Contrast magnetic resonance imaging of the brain showing diffuse meningeal enhancement
DISCUSSION
The nervous system can be involved at any stage of brucellosis. Both central and peripheral nervous systems can be affected by this condition. Acute or chronic meningitis are the most frequent nervous system complications of brucellosis. The diagnostic criteria of neurobrucellosis include (a) clinical findings compatible with neurobrucellosis; (b) pleocytosis with predominant lymphocytes and elevated protein concentration in CSF; (c) positive results of either blood or bone marrow or CSF culture or positive serologic tests; (d) clinical improvement following antibiotic therapy against brucellosis; and (e) no other alternative diagnosis.[3] The patient had all of these: clinical findings and serologic evidence of brucellosis, lymphocytic pleocytosis with high protein in CSF, response to therapy, and no alternative explanation.
Sensorineural hearing loss although rare has long been reported in patients with neurobrucellosis and if the disease is not treated early, permanent hearing loss can occur.[2] The finding can be overlooked if other features of neurobrucellosis are not prominent. In our patient, the hearing loss was wrongly thought to be noise induced and the associated headache was treated symptomatically. Consequently, the patient had a residual hearing loss due to delay in diagnosis and treatment.
Psychiatric symptoms are quite rare in neurobrucellosis. The reported psychiatric manifestations usually seen in brucella meningitis include depression, amnesia, agitation, personality changes, euphoria, and psychosis among which depression is the most common.[4] Delirium may also occur in acute brucellosis. Our patient had psychosis of only 2-day duration that was controlled with a good dose of antipsychotic. Drugs may be needed in some cases to control acute psychosis, although the symptoms usually improve with treatment of brucellosis.[5] We conclude that new-onset psychosis without fever with a history of hearing loss could suggest the diagnosis of chronic neurobrucellosis.
Our case highlights the importance of considering neurobrucellosis as a differential diagnosis in patients with unexplained neuropsychiatric symptoms such as acute psychosis or hearing loss. Early diagnosis and treatment of the disease will help in decreasing the morbidity, mortality, and sequelae of this condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Brucella species. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas and Bennett's Diseases. Philadelphia: Churchil Livingstone; 2000. p. :2386-92.
- [Google Scholar]
- Psychosomatic and somato-psychic aspects of brucellosis. J Psychosom Res. 1976;20:339-50.
- [Google Scholar]






