Translate this page into:
Neuro-Ophthalmology at the Bedside: A Clinical Guide
Address for correspondence: Prof. Josef G. Heckmann, Department of Neurology, Municipal Hospital Landshut, Robert-Koch-Street 1, Landshut-84034, Bavaria, Germany. E-mail: josef.heckmann@klinikum-landshut.de
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neuro-ophthalmological signs and symptoms are common in the emergency department but are a frequent source of diagnostic uncertainties. However, neuro-ophthalmological signs often allow a precise neuro-topographical localization of the clinical problem. A practical concept is presented how to perform a neuro-ophthalmological examination at the bedside and to interpret key findings under the aspect of emergency medicine with limited resources.
Keywords
Blurred vision
diplopia
headache
Horner's syndrome
neurological emergencies
neuro-ophthalmological examination
INTRODUCTION
W. F. Hoyt, a pioneer of clinical neuro-ophthalmology, is cited: “Neuro-ophthalmology is like a harp, every orchestra needs one, but not all the time.”[1] Regarding the clinical daily work this should be assented. However, basic knowledge and skills in neuro-ophthalmology are necessary to care for a patient with neuro-ophthalmological signs as these can be index symptoms of acute and severe cerebral and ocular diseases. With this competency, a rational rapid and straightforward diagnostic procedure can be initiated. In addition, neuro-ophthalmological findings are of high neuro-topographical value, so to speak they allow a view in the brain through the window of clinical neuroanatomy. A typical example is the internuclear ophthalmoplegia which indicates a lesion of the medial longitudinal fasciculus (MLF).[23] Some neuro-ophthalmological findings are highly indicative or even pathognomonic for systemic diseases such as impaired vertical saccades in Niemann–Pick disease.[4]
Thus, the basal neuro-ophthalmological examination is very important comparable to the basal neuro-otological examination[5] supplementing the general clinical neurological examination where necessary. The aim of this paper is to present a practical concept of such a basic neuro-ophthalmological examination which can be performed easily in the accident and emergency unit and medical practice without being time-consuming or requiring expensive technical equipment. This contribution replaces in no way the current excellent reviews and standard books of clinical neuro-ophthalmology.[1678910]
Search strategy and selection criteria
We searched selectively PubMed from 1970 to 2017 for articles with the keywords “neuro-ophthalmological examination,” the “bedside and office neuro-ophthalmology examination,” “test on neuro-ophthalmological disorders,” “neuro-ophthalmic emergencies,” and “clinical neuro-ophthalmology.” We also searched the reference list of selected articles, the authors’ personal libraries including classic textbooks. Emphasis has been put on conditions that typically present to the practicing neurologist on duty in the office or the primary hospital service.
History taking
Neuro-ophthalmological history may be very complex and difficult, but some rules may make it easier. At the beginning, the question on “what is wrong with your eyes and your vision” may be very useful.[11] Then, begin and course of visual disturbances should be analyzed. Which was the first symptom and how did it develop? With which velocity did the symptoms progress [Figure 1].
![Neuro-ophthalmological history focusing on symptom onset and duration[7]](/content/150/2018/9/4/img/JNRP-9-561-g001.png)
- Neuro-ophthalmological history focusing on symptom onset and duration[7]
Is there any pain? Is the disorder monocular or binocular? Beside the neuro-ophthalmological symptoms do other symptoms persist such as headache? Do other neurological findings prevail, for example, a monocular vision loss combined with a contralateral hemiparesis.[12] A general neurological history should also be taken with questions about previous symptoms, for example, migraine or epilepsy. The circumstances of the onset of symptoms should be asked, or the medication taken (visual disturbances associated with medications). It should always be specified, what the patient means by “blurred vision.” Has he difficulties in seeing details, an impairment of central vision or an impairment of vision in the outer visual fields?[13]
Examination of visual acuity
A proposal for the course of the neuro-ophthalmological examination is given in Table 1.

In the emergency situation, the visual acuity can be easily tested using a visual card [Figure 2].
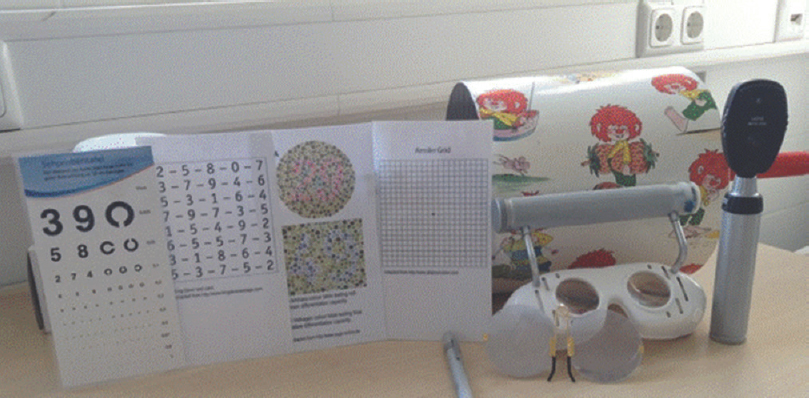
- Armamentarium for the clinical neuro-ophthalmological examination at the bedside, in the emergency room or the office (from left to right: test cards - vison card, King-Devic test, colour tables, Amsler grid -, flashlight, nystagmus drum, Frenzel and Munich glasses, ophthalmoscope)
With good lightening, the visual card is presented at a distance of about 35 cm. Care should be taken that adequate spectacle correction is worn in presbyopic or highly ametropic patients. Each eye is examined separately. The patient should read the optotypes (e.g., numbers or Landolt rings) he can see. If he cannot see and read the numbers or rings, he should be asked whether he is able to recognize and count fingers or the movements of a hand in 1 m distance. Is this not possible, the perception of light is tested. It is prudent to use a bright penlight, while the fellow eye has to be occluded carefully (e.g., with the use of a patch or the examiner's (not the patients!) hand. For a detailed analysis of the visual acuity, an ophthalmologist is requested.[14]
Examination of the pupil
When examining the pupils, it should be taken into account that about 20% of healthy individuals reveal a slight difference of pupil width of up to 0.5 mm in diameter. Notably, the elderly show frequently a diminished pupil size. The width, the form and a difference of the pupils should be noted followed by reaction to light and convergence. The examination of the pupils is easier in a dimmed room.[1516]
As a standard, the direct light reaction and the near reaction are tested. The consensual light reaction is necessary in a case of an anisocoria of 0.4 mm and more. In the swinging-flashlight test, the eyes are alternately illuminated by a penlight. In a healthy individual, both pupils show the same size and show an equal direct light reaction. In case of a disturbance of the afferent visual system, the direct light reaction on the affected side will be reduced or even absent. As the swinging flashlight test allows a comparison of the direct light reactions of both eyes, a reduced constriction of the pupil on the affected side is easy to detect. It is recommended to test 5–6 reactions for each eye with an illumination for 2–3 s. In case of an “absolute” afferent defect not only a reduced constriction but a “paradoxical” dilation of the pupil is seen despite the illumination of the eye. Differences in the light distance, illumination angle, illumination durance, too intensive and too weak light and too bright a room can lead to misinterpretation. It is important that a unilateral disorder of the cornea, the lens and the vitreous body do not lead to an afferent pupil disorder whereas a unilateral optic nerve lesion regularly goes along with a disturbed swinging-flashlight test. Due to the crossing of the afferent fibers at the chiasma and the double innervation of the Edinger–Westphal nuclei by the nuclei of the area pretectalis direct and consensual pupil reactions are equal.[15] However, in case of an efferent dysfunction (oculomotor nerve, ciliary nerve, and iris) an anisocoria occurs, and direct and consensual pupil reactions are different. At this point, it has to be differentiated which pupil is the affected one. Is the background, a mydriatic pupil due to a lesion of the oculomotor nerve, the ciliary nerve or the iris, or is the miotic eye the affected one due to a Horner's syndrome.[15]
An isolated mydriatic pupil in the context of an oculomotor nerve lesion is rare.[17] In virtually all patients, additional signs of a third nerve lesions are present, such as ptosis and dysfunction of the muscles innervated by the oculomotor nerve. In case of an oculomotor nerve lesion beside a compressive space-occupying process, inflammatory, tumorous, and vascular processes have to be considered.[1617181920]
Horner's syndrome with miosis
In Horner's syndrome, the sympathetic innervation of the pupil is impaired leading to an insufficiency of the pupil dilator muscle. Thus, the capacity to dilate is impacted.[1621] Mostly in case of Horner's syndrome, a slight ptosis can be observed due to an impairment of the lid lifting Müller's muscle, and sometimes, a diminished sweating in the face. In the dimmed room a Horner's syndrome can be recognized easier. The pharmacological test using sympathomimetic apraclonidine drops can be very helpful and is easier to perform than the traditional cocaine test (Apraclonidine 0.5%, Iopidine, Alkopharma). The effect of these drops is based on a rapidly developing hypersensitivity of the alpha-1-receptors of the dilator muscle in case of a Horner's syndrome. The drops provoke no change in the healthy pupil but lead to a marked increase of the pupil size at the Horner's side and this within 15 min after application of the drops. Thus, in case of a Horner's syndrome, a reversal of the pupil difference can be observed. About 15 min after application of apraclonidine drops the previous smaller pupil will be the wider one.[21] In general, the clinical finding of an acute Horner's syndrome is an emergency case. Beside central disorder (brainstem ischemia such as Wallenberg syndrome), dissection of the carotid artery and spinal causes have to be considered.[212223]
Adie's tonic pupil (pupillotonia)
Pupillotonia typically describes a dissociation of the light-near-reaction of the pupil with a strongly delayed and diminished reaction to light but less impaired near reaction. This phenomenon can be seen as the reverse of a Horner's syndrome as in pupillotonia the parasympathetic innervation (constriction) is disturbed.[24] Typically, the pupils are dilated and do not or only sparsely react to light, yet better to a near stimulus. A positive test with cholinergic pilocarpin drops (0.1%) and constriction of more than one-third of the initial diameter is strongly suggestive of pupillotonia as it demonstrates a hypersensitivity of the sphincter of the iris.[16] Often pupillotonia is accompanied by missing muscle reflexes (Adie's syndrome) and other vegetative disturbances such as hypohidrosis (Ross syndrome)[25] or orthostatic hypotension (Shy-Drager syndrome). Such a parasympathetic dysfunction is mostly localized in the parasympathetic plexus behind the eyeball (e.g., ganglion ciliare) and can occur following a virus infection.[24] The typical patient is a middle-aged women, the patients usually do not have complaints, and do not notice the impaired accommodation in the affected eye. In case of a missing constriction in the pilocarpin test, a pharmacological blockade of the iris sphincter has to be assumed. Long-standing pupillotonia exhibits a miotic pupil, smaller than the nonaffected side; the condition may also occur in the fellow eye.
Botanic and cosmetic mydriasis
In patients with a unilateral wide and unreactive pupil, a pharmacological blockade has to be discussed (botanic and cosmetic mydriasis). By contact with alkaloids of plants (Angel's trumpet, jimson weed, and deadly nightshade) the anticholinergic can locally affect the pupil and cause mydriasis and other anticholinergic symptoms.[15] This information usually is not volunteered by the patient and should be specifically asked for. Similarly, the contact with some types of cosmetics, medical patches with anticholinergics, or even flea spray can cause a unilateral wide pupil.[26] In this case, the pilocarpine test (0.1%) is negative and does not lead to constriction of the pupil.
Ptosis
At first, it should be elaborated which eye is the affected one and in which time frame the ptosis developed. Often a look on previous photographs (identity card and driving license) can be helpful. In case of acute neurological care, three scenarios should be cleared rapidly: palsy of the oculomotor nerve, Horner's syndrome, and myasthenia-related ptosis.[2728] In case of an oculomotor nerve lesion, further disturbances such as mydriasis and dysfunction of extraocular muscles leading to diplopia should be searched for. A Horner's syndrome is easier detected in the dimmed room, and the pharmacological test using apraclonidine can confirm it (see above). For differentiating myasthenia the Simpson test, tests of “peek sign” and “Cogan lid twitch,” icepack-test or sleep-test and edrophonium- or pyridostigmine-test can be applied.[2930] The motility impairment in myasthenia may be extremely variable, from cases mimicking childhood strabismus, to paresis or supranuclear motility disorders. Therefore, the further neurological examination, observation of fluctuating symptoms during daytime with improvement after rest, analysis of autoantibodies, and neurophysiological studies after repetitive stimulation contribute markedly to the diagnosis.[2930] By history taking rare causes of ptosis can be identified such as (rarely) thyroid disease, orbital, ear, nose, and direct lid processes. Ptosis due to primary muscle diseases (myotonic dystrophia, chronic progressive external ophthalmoplegia, and mitochondrial cytopathies) are mostly identifiable by history. Often simple dermatochalasis – predominantly in the elderly – with insufficiency of the skin can be mistaken as ptosis. However, dermatochalasis is characterized by redundant skin, while the position of the lid margin and the motility of the levator muscle is correct. Under the term of the neurogenic cause of ptosis Miller-Fisher syndrome, a variant of Guillain–Barré syndrome, can manifest itself with ptosis first.[27] In rare cases, a cortical lesion, predominantly stroke of the nondominant hemisphere can cause cerebral ptosis.[28] In this situation, the finding has to be differentiated from lid apraxia, for instance in the context of a progressive supranuclear palsy where the patient has difficulties to open the lid although he is able to keep the eyes open when successfully opened. Ptosis should not be mistaken for an overactive muscle activity of the orbicular muscle in case of blepharospasm or hemifacial spasm or even after aberrant facial reinnervation.[27]
Acute visual loss
First, it should be ascertained whether the visual loss is monocular or binocular and in which temporal course the symptoms developed or how long symptoms persisted. In case of amaurosis fugax, the symptoms are typically short-lasting. In the emergency case, three clinical conditions have to be elaborated rapidly: Occlusion of the retinal and optic nerve vessels (ischemic optic neuropathy), arteritic process and neuritis of the optic nerve.
The visual impairment in ischemic optic neuropathy ranges from moderate to severe, sudden and painless without signs of a red-eye combined with edema of the optic disc.[31] Standard workup consists in identifying possible risk factors for cardiovascular disease and initiation of the treatment if appropriate. Whether or not acute ischemic optic neuropathy should be additionally treated by 6-week course of oral steroids, is a matter of debate.[32] Treatment with platelet aggregation inhibitors is usually recommended for up to 2 years (also in view of the fact of a risk for the fellow eye). However, treatment effects are generally poor. As an off-label therapy, a systemic thrombolysis can be undertaken in the first hours.[33] In this case, the diagnostic workup is necessary like in the stroke unit care, in particular, a sonography of the ipsilateral carotid artery is mandatory. In case of a vasculitic background (giant cell arteritis), systemic clinical symptoms often occur such as fatigue, pain, myalgia, masticatory claudication, and other. In addition, erythrocyte sedimentation rate and level of C-reactive protein are usually elevated. A steroid therapy has to be initiated without delay. Even then however, substantial loss of vision usually cannot be prevented; the therapy thus mainly aims at preservation of vision in the fellow eye. Risk of arteritic optic neuropathy in the second eye fortunately decreases over time/months.
In optic neuritis, the visual impairment usually is not so dramatic and is characterized by a visual loss developing over a period of 1–2 weeks. It is more often described as a type of fogging and diminution of color vision. Typically, however, the patient reports on painful ocular movements. Sometimes, the disease process is at the papilla and can be seen on fundoscopy (papillitis), mostly, however, the disease process is located in the retrobulbar space (retrobulbar neuritis). Thus, it is described as “the patient sees nothing and the doctor sees nothing (abnormal).” A mnemonic TYPICAL (T = Transient visual loss, “down in days, up in months;” Y = Young adults, 20–50 years;P = Pain with eye movements; I = Inconspicuous ophthalmoscopic findings; C = Central scotoma; A = Afferent pupillary defect; and L = Leber's hereditary optic neuropathy does not run in the family) summarizes the typical signs of optic neuritis.[34] A steroid therapy is generally recommended as this should support the healing.[3536] Always neuritis of the papilla and the optic nerve due to lues, sarcoidosis, tubercular and cryptococcal meningitis, complicating cavernous sinus thrombosis, collagenosis or cytomegalic viral infection or even optic compression by a tumor should be differentiated.[3738] Transient monocular visual disturbances sometimes can be caused by vasospasm and treated with calcium antagonists.[39]
Diplopia
In the emergency department, patients usually present with acute onset of diplopia. However, often patients have difficulties to describe their visual disturbances and in particular the pattern of diplopia. Often additional signs and symptoms are complained about such as blurred vision, unsteadiness, dizziness, and lightheadedness. For taking the history of a patient with diplopia a number of questions are quite useful such as: Is the diplopia monocular or binocular (this should be tested by proper monocular investigation, as patients usually do not discern monocular or binocular phenomena)? Is the diplopia constant, intermittent or variable? In which direction is diplopia worsening? Is it worse at distance (car driving, looking outside the window) or near viewing (reading and eating)? Is the diplopia associated with pain, headache, or neurologic symptoms?[404142]
Monocular diplopia persisting after covering the healthy eye is typically caused by an uncorrected refractive error. This may be long-standing, like uncorrected astigmatism but also acquired such as a corneal lesion or a disorder of the lens (cataract). In this case, a thorough ophthalmological examination is mandatory. Binocular diplopia occurs when the fusion of the images from both eyes is disturbed in particular due to ocular misalignment and ophthalmoparesis.[4344] The topic of nonparetic and longstanding or pediatric strabismus is described elsewhere.[4546] Ocular myasthenia typically shows a number of characteristic features but can cause considerable diagnostic problems.[2930]
The examination of ocular movements is tested in nine directions and documented adequately [Figure 3].[47]
![(a) H-shape for test of ocular motility; (b) Usual range of ocular motion in millimeters (modified according to Biller et al., 2011)[47]](/content/150/2018/9/4/img/JNRP-9-561-g004.png)
- (a) H-shape for test of ocular motility; (b) Usual range of ocular motion in millimeters (modified according to Biller et al., 2011)[47]
The patient's eyes are observed for possible misalignment, and the patient is asked for diplopia. Horizontal misalignment is described in terms of exodeviation (exotropia and exophoria) indicating an outward deviation of the nonfixing eye and esodeviation (esotropia and esophoria) indicating an inward deviation of the nonfixing eye. In general, a tropia is a manifest ocular misalignment, and a phoria is a latent one which manifests after interruption of fusion.[46] Hyperdeviations indicate an impaired ocular depression or elevation, whereby a hypertropia means a vertical deviation, in which the nonfixing eye is higher. Thus, in hypotropia the nonfixing eye is lower.[46] In concomitant strabismus, the misalignment is constant in all directions, in nonconcomitant strabismus the degree of misalignment depends on the direction of view. In most neurological disease, a strabismus is nonconcomitant.
After testing the ocular movements in the nine directions, the next step is to test the capacity to stabilize the gaze. The patient is requested to look ahead, to look near and far and then excentric for at least 2 min to detect gaze-evoked nystagmus. By using an ophthalmoscope, the Frenzel glasses or the Munich Fresnel glasses fixation is suppressed, and spontaneous nystagmus due to a vestibular disorder can be detected.[5] Furthermore, the different functional classes of ocular movements are tested (optokinetic movements, vestibular induced movements, vergence, smooth pursuit, and saccades).[44849]
By keeping some rules in mind and recognizing common patterns of ophthalmoparesis, the most frequent disturbances of ocular misalignment can be evaluated clinically at the bedside. The four rules to identify a weak extraocular muscle are as follows: (I) the false image is usually the less sharp and the more peripheral one, (II) diplopia occurs in positions which depend on the contraction of the affected muscle, (III) the false image is projected into the usual direction of the affected muscle, and (IV) the distance between the two images increases in the direction of action of the affected muscle.[50]
A diagram for a differential diagnosis of diplopia concerning acute neurogenic, myogenic (orbital), and central processes is presented in Figure 4.[51]
![Diagram to analyze acute diplopia[51]](/content/150/2018/9/4/img/JNRP-9-561-g005.png)
- Diagram to analyze acute diplopia[51]
Abducens nerve palsy
This pattern is usually easy to recognize. The separated images are horizontally side by side, and the distance increases in the direction of action of the lateral rectus muscle. A diminished abduction can be observed. The patient complains about double vision when looking into distance (e.g., driving car), but has no double vision for near tasks. Sometimes, double vision is avoided by a head tilt to the affected side (avoiding abduction the paretic eye). Thus, during examination, a proper head position has to be maintained. It should always be kept in mind, that the etiology of an impaired lateral rectus muscle can be neurogenic, mechanical, myogenic, or neuromuscular.[50]
Oculomotor nerve palsy
In full oculomotor nerve palsy, the parasympathetic function and the levator function are impaired, thus a pronounced ptosis is present and the pupil is wide and without reaction. In this case, as a rule the eye is “out and down.” Diagnosis is much more difficult if the pupil function is intact and the ptosis is only mild. Thus, mainly adduction, elevation, and depression in abduction are impaired.[52] Etiologically also nuclear lesion, mostly vascular, has to be considered (e.g., Achard-Lévi-syndrome).[19] In vascular nerve lesion (diabetes, arterial hypertension), mostly the parasympathetic part is spared while in compressive condition (space-occupying process, elevated brain pressure, and compression by aneurysm) the parasympathetic dysfunction is marked leading to a wide nonreacting pupil.
Trochlear nerve palsy
This condition is most difficult to identify. The double vision is most prominent looking down (going downstairs) or during reading (near viewing). The images are twisted with one image at an angle to the other image or rarely vertical.[52] A simple test is to ask the patient to look down a horizontally held pointer resulting in recognition of a horizontally “V” whereby the tip of this letter indicates the affected eye.[51] Moreover, the patient often keeps the head tilted to avoid double vision (the head is inclined toward the contralateral shoulder, which reduces the need of incyclorotation). Looking to the opposite side of the affected nerve and tilting, the head ipsilateral to the affected site hyperdeviation is more prominent and increasing. This can be elicited by the Bielschowsky head tilt test. A squint is usually not visible.[50]
Saccades, smooth pursuit movements, convergence, internuclear ophthalmoplegia
Saccades
Saccades represent rapid, targeted eye movements. They are tested by asking the patient to look straight ahead to the outstretched index finger of the examiner and then rapidly to look to the other index finger which is placed laterally so that the patient has to move his eyes about 30°. The patient should look alternately with a frequency of 1 Hz from the mid-positioned outstretched index finger to the 30° laterally outstretched finger. The clinician observes the saccades whether they are possible at all, too slow, hypometric, and hypermetric or accurate. This test is followed by the test of vertical saccades in a similar way.[49] The generation of saccades is quite complex.[53] Beside cortical areas, the paramedian pontine reticular formation and the upper colliculi are very important. In addition, the cerebellum has a modulating effect. Therefore, in a cerebellar disorder, often a saccadic smooth pursuit is encountered. For clinical testing of saccadic function, the King-Devick-test can be applied [test card, Figure 2]. In this test, the examined person has to read loudly the numbers of a demonstration card from left to right and from above to below. Then, the person has to read three standardized test cards. The results of required time and of mistakes are noted. By this method, the capacity to generate saccades is tested whereby alertness, speech function, and additional neurocognitive functions contribute to the competency. In patients with traumatic brain injury, Parkinson's disease or multiple sclerosis, in whom often neuro-ophthalmologic complaints occur, this test reveals significant impairments.[545556] Recently, a variant, a rapid picture naming test, has been piloted.[57] In general test on saccades are very useful in hyper- and hypo-kinetic movement disorder patients.[58]
Smooth pursuit movements
In testing the smooth pursuit, the patient is asked to fix an object (stethoscope, reflex hammer, or finger of the examiner) which is moved smoothly horizontally and vertically. It is important to move the object not too quickly (maximal 30°/s) and not too laterally.[49] In order to perform a physiological smooth pursuit intact cerebellar, cortical, and retinal function is necessary. In particular, the projections from the temporo-parieto-occipital cortex and the frontal eye fields to the pons are essential as well as the function of the abducens nerve.
Convergence
Testing convergence is best done by requesting the patient to look down to his outstretched thumb which is slowly moved to the nose. It is judged whether this is possible without problems or at which distance the fusion is insufficient, and exotropia occurs. Physiologically, the constriction of the pupil should be recognized whereby the neuronal mechanism of this pathway is not fully understood. The normal near point of convergence is between 5 and 10 cm. Disorders of convergence are frequently encountered in patients with traumatic brain injuries.[56]
Internuclear ophthalmoplegia
This pattern of eye movement disorder is caused by a dysfunction of the MLF, a connection between the oculomotor nuclei. The criterion is a dysconjugate horizontal eye movement with incomplete and/or slowed adduction on the side of the affected MLF. Often the disorder is accompanied by a nystagmus on the abduction of the contralateral eye.[3] In the emergency situation, most causes are vascular [Figure 5].
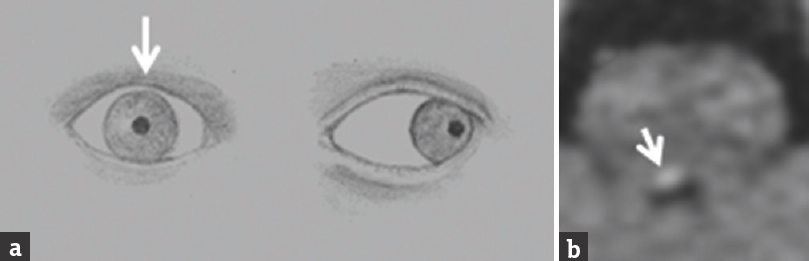
- (a) Drawing of a patient's eye postion revealing right-sided internuclear ophthalmoplegia (white arrow) (b) Corresponding diffusion weighted MRI demonstrating small infarction at the level of the pons and affecting the medial longitudinal fasciculus (white arrow) (Courtesy of PD Dr. H.P. Dinkel, Department of Radiology, Municipal Hospital Landshut, Germany)
If this pattern is combined with a horizontal gaze paralysis the 11/2 syndrome persists, a severe pontine eye movement disorder, which enables the patient only the movement of one eye to the side.[59] As a rule horizontal eye movement disorders topographically point to the pons whereas vertical eye movement disorders point to the midbrain [Figure 6].

- 84-year-old woman with acute onset of visual disturbances. (a) Vertical gaze (up and down) is markedly impaired while the horizontal gaze is intact. (b) Diffusion weighted MRI demonstrating infarction at the level of the midbrain and thalamus (white arrow) (Courtesy of PD Dr. H.P. Dinkel, Department of Radiology, Municipal Hospital Landshut, Germany)
Vestibulo-ocular reflex
The vestibulo-ocular reflex connects the vestibular system with the ocular system. Following a rapid head impulse, the position of the eyes is held physiologically stable. To detect a peripheral vestibular disorder, the head impulse test is quite useful. The test, introduced by Halmagyi was described recently in a review in this journal.[5]
Visual field
Slowly developing visual field defects are typically not noted by the patient, at least not before disturbances in daily life occur such as getting stuck in a door frame, causing a traffic accident or problems with reading. The “missing” areas of the visual field are compensated by a “filling in” of visual information. In diseases with shorter duration, the disturbances may be described as a type of fog or dark spots. To test the visual fields clinically at the bedside, the confrontation test is used. The examiner stands at a distance of about 1 m to the patient with the eyes at the same height as the patient. The patient is asked to look with both eyes at the nose of the examiner while the latter one is stretching the arms and hands at first into both upper quadrants and then into both lower quadrants. The examiner looks into the eyes of the patient and simultaneously moves one or both index fingers asking the patient which finger moves. This examination is of course only a very rough one. A visual field defect can be analyzed in more detail at the bedside by examining each eye separately. The examiner brings the moving outstretched index finger from the border of the visual field inwards and asks the patient to say “now,” when he recognizes the finger. This method can be supplemented by using red points such as the cap of a red biro.[60] In comatose patients, the blink-to-threat reflex can be done.[61] The examiner performs a rapid movement with the hand coming from the lateral visual field and observes whether the patient blinks or shows a type of defense reaction. A unilateral loss of such a reaction is a strong hint for hemianopia. With these clinical tests usually a homonymous hemianopia or quadrantanopia and a bitemporal hemianopia should be recognized. Bitemporal visual field deficits indicate a dysfunction of the optic chiasm, for example, due to a pituitary adenoma. Homonymous hemianopia or quadrantanopia indicates a dysfunction of the postchiasmal optic pathway and the visual cortex.
Visual field deficits in the upper quadrants are described as “pie in the sky” and result from a lesion of the lower retrochiasmatic visual pathway (Meyer's loop in the temporal lobe). A lower quadrantanopia is the result of a lesion at the upper retrochiasmatic visual pathway (Baum's loop in the parietal cortex). For exact analysis of the visual fields perimetry in the hands of the ophthalmologist is necessary. This method enables additional detection of circumscribed visual deficits and enlargement of the blind spot.[62] As a rule, the visual fields are described from the patient's perspective and divided into nasal and temporal fields.
Fundoscopy
Applying fundoscopy the ocular fundus and in particular the papilla can be inspected even without pharmacological mydriasis. The doctor's eye usually examines the same eye of the patient, i.e., the left eye examines the patient's left eye and vice versa. In the dimmed room, the patient is asked to look slightly upward and inward. The examiner nears slowly with the ophthalmoscope and sees through the pupil the ocular fundus, first catching vessels, and then following them to the papilla. By nearing from the temporal side, the constriction of the pupil is normally less intensive. For the neurologist in the emergency situation, the recognition of optic disc swelling and its differential diagnoses as well as optic atrophy should be possible.[3263] However, to perform such a fundoscopy and to judge the findings adequately practice and experience are necessary. In general, the direct fundoscopy is decreasingly applied in emergency rooms and unfortunately seems to become a “dying” art.[64] An interesting alternative may be in the future nonmydriatic ocular fundus photography [Figure 7] or even smartphone fundoscopy which has been shown to be useful in the emergency situation with notable advantages over direct ophthalmoscopy.[65666768]
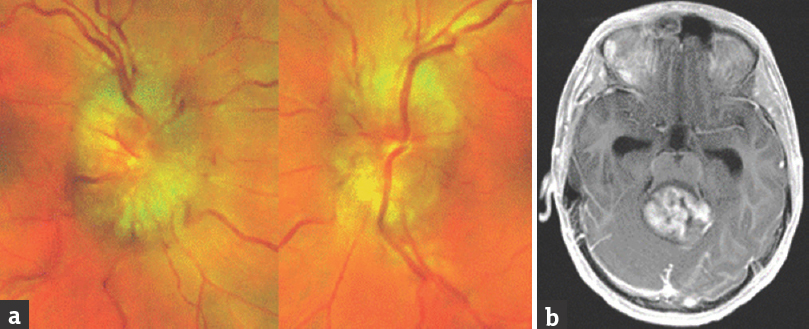
- Patient 15-year-old, headache during soccer play, slight diplopia. (a) Nonmydriatic ocular fundus photography revealed pronounced papilledema prompting MRT (b) which revealed a space occupying process of the posterior fossa. (Courtesy of Dr. Kretz, Ophthalmologist, Landshut; Courtesy of PD Dr. H.P. Dinkel, Department of Radiology, Municipal Hospital Landshut, Germany)
Higher visual disturbances
Higher visual disturbances can be caused by functional and structural disorders of the visual cortex and its associative structures.[6970] They are rare and often not readily reported by the patient spontaneously. Phenomenologically, they can present quite differently such as in the form of hallucinations, visual perseverations, palinopsia, prosopagnosia, object agnosia, achromatopsia, neglect, or Bálint-Holmes syndrome.[7172] In most cases, these disorders are clinical presentations of stroke, encephalitis or tumor. These higher visual disorders are frequently associated by additional neurologic symptoms and signs. This topic is described elsewhere in detail.[69707173] The mentioned disorders are often transient and have a good tendency to resolve spontaneously depending on the underlying cause. It is important for the physician to be ready to pay attention to such phenomena of the patient and to ask the patient in more detail when such disorders are assumed. The experience of visual hallucinations in visually impaired individuals, namely Charles Bonnet syndrome, not only occurs in the elderly but also among young subjects.[74]
Amsler-grid
By this method, central scotoma and other disorders of the central retina can be detected; the size of the testing field represents the central 30° of the visual field. Each eye is tested separately, in presbyopic patients with adequate spectacle correction. The test card shows a grid with a central fixation mark; the patient is asked whether he sees dark or blurred spots, curved lines, gaps or whether he is able to see the central dot. Any disturbances indicate a disorder of the central retina/macula and necessitate a thorough ophthalmologic examination. The Amsler-grid is available as a test card [Figure 2] for the doctor's white coat as well as in a computerized form at the screen of a personal computer. It is important that the distance between the grid and the test person's eyes is about 30–40 cm. Recently, this simple test was used to detect optic maculopathy associated with intake of antirheumatoid drugs.[75]
Examination with the nystagmus drum
With this test, smooth pursuit and reset saccades can be examined both horizontally and vertically.[76] The drum [Figure 2] is rotated at a velocity of 90°–180° per se cond and the patient focuses on the pictures of the drum. The examiner observes the smooth pursuit in the direction of the drum's movement and the reset saccades in the opposite direction. By turning the drum about 90°, the vertical eye movements are tested in a similar way. It is of interest that for instance, an impairment of vertically induced reset-saccades is quite pathognomonic for early Niemann–Pick's disease.[4]
DISCUSSION
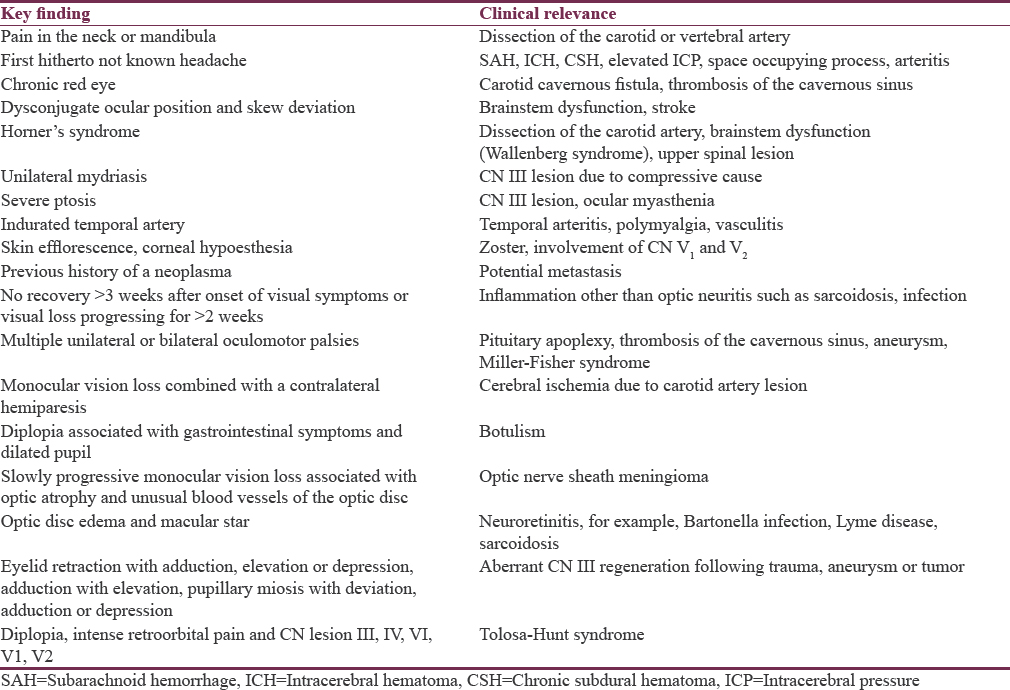
The great value of an accurate clinical neuro-ophthalmologic examination is that clinical findings can be correlated well with the localization of the lesion. In other words, the result of the examination gives an answer to the primordial question in clinical neurology “where is the lesion.” As a rule of thumb disturbances of the vertical eye movements indicate a dysfunction at the midbrain level and disturbances of the horizontal eye movements a dysfunction of the pontine brainstem. The syndrome of internuclear ophthalmoplegia allows the assumption of a lesion of the longitudinal medial fascicle which connects the nuclei of the optomotor nerves in the paramedian pons near the aqueduct. Hemianopic visual fields point to a retrochiasmatic lesion of the visual pathway. A sudden monocular blurred vision requires a particular view on the ipsilateral internal carotid artery. It is highly interesting that in single conditions a neuro-ophthalmological finding such as the impairment of vertical saccades can be pathognomonic for a systemic disease such as Steele-Richardson-Olszewski syndrome or the Niemann–Pick disease while abnormalities of the horizontal saccades can be pathognomonic for Gaucher disease. Niemann–Pick disease can be treated nowadays after early diagnosis.[4] In headache of different origin, the neuro-ophthalmological status is of outstanding importance. Together with the headache history the clinical findings identify the red flags of headache and guide the diagnostic process [Table 2].[7778]
In the general neurological emergency medicine, the neuro-ophthalmological examination is of great value as its findings enable a sophisticated deduction and a judicious use of technical investigations.[79] For instance vestibular nystagmus in the context of a harmonic vestibular syndrome allows diagnosis of acute vestibulopathy or the findings of “Head Impulse, Nystagmus, Test of Skew” are helpful in the diagnosis of an acute stroke of the posterior circulation.[5]
The neuro-ophthalmological examination can be rapidly done, needs little instrumental equipment [Figure 2] and can thus guide more sophisticated diagnostic investigation such as brain imaging, lumbar puncture and additional tests.[808182] However, it is difficult to acquire examination competency in neuro-ophthalmology. Besides studying the anatomical and physiological background, intensive clinical exercises are mandatory to familiarize the examiner with this field of clinical medicine. Modern audiovisual aids – meanwhile available through the internet – can be very useful in teaching clinical neuro-ophthalmology. Step by step demonstrations and instructive case vignettes of basic knowledge and practical skills can be conveyed to the interested self-taught learner.[2449838485] Special “clinical image”-sections in scientific journals support the learning process.[43868788899091] In recent years, medical education curricula increasingly emphasize the learning of practical skills such as the neurological examination including the neuro-ophthalmological examination or the ophthalmological exam.[92939495] In our view, this general trend of more practical teaching at the medical schools should be supported with emphasis. By this way, diagnosis in clinical medicine can be made easier and more cost-effective. Regarding practical skills, unfortunately, the competency of direct fundoscopy is discussed and a demise of direct ophthalmoscopy is feared.[64] Technical improvement such as the “PanOptic”-ophthalmoscope may ease the learning process of ophthalmoscopy and actually enable a broader view on the ocular fundus.[96] Recently, the nonmydriatic digital fundus photography was developed and judged to be more sensitive than direct ophthalmoscopy in several settings. It can be feasibly performed in the emergency situation and improve neurological and cerebrovascular diagnosis.[66] Its costs should markedly decrease as it can be applied meanwhile with a smartphone.[67] It is of interest that methods which were sparsely used in the last years, now have a certain renaissance such as the optokinetic nystagmus testing by a drum.[76] This test is very easy to perform and gives valuable information on the patient's capacity of smooth pursuit and reset saccades horizontally and vertically. Thus a number of neuro-ophthalmological disorders can be detected early in the course of the disease. In how far new technical methods such as the video-oculography, the scanning laser Doppler flowmetry, laser scanning tomography or optical coherence tomography may find their way into routine clinical neuro-ophthalmological praxis even in countries with lower income remains unsettled.[39979899]
The statement of the Nestor of modern neuro-ophthalmology W. F. Hoyt comparing the neuro-ophthalmology with a harp, which is necessary for every orchestra but not at all times, is confirmed by our experience. Clinical competency in neuro-ophthalmology is not always mandatory in every neurological patient. However, if clinical neuro-ophthalmological competency is available in caring for patients with neuro-ophthalmological disorders a straightforward diagnostic process can be initiated generating a viable working diagnosis and applying cost-extensive methods considerately.[100] It is, therefore, a pleasing development that in a number of developing countries the importance of neuro-ophthalmology is acknowledged leading to the foundation of neuro-ophthalmological units.[101102103]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Klinische Neuroophthalmologie. Stuttgart: Thieme Verlag; 1998.
- Central oculomotor disturbances and nystagmus: A window into the brainstem and cerebellum. Dtsch Arztebl Int. 2011;108:197-204.
- [Google Scholar]
- Central ocular motor disorders, including gaze palsy and nystagmus. J Neurol. 2014;261(Suppl 2):S542-58.
- [Google Scholar]
- Acute dizziness in rural practice: Proposal of a diagnostic procedure. J Neurosci Rural Pract. 2015;6:272-6.
- [Google Scholar]
- Clinical Neuro-Ophthalmology. Berlin, Heidelberg: Springer; 2007.
- Walsh & Hoyt's Clinical Neuro-Ophthalmology: The Essentials (3rd ed). Alphen aan den Rijn: Wolters Kluwer; 2016.
- Neuro-Ophthalmology Illustrated. Stuttgart: Thieme; 2015.
- Neuro-Ophthalmology: What do I do now?. Oxford and New York: Oxford University Press; 2012.
- Clinical reasoning: A 42-year-old man who developed blurred vision and dropped his iPod while jogging. Neurology. 2014;83:e89-94.
- [Google Scholar]
- Pupillary disorders – Diagnosis, diseases, consequences. Klin Monbl Augenheilkd. 2010;227:845-51.
- [Google Scholar]
- Internal ophthalmoplegia: First sign of compressive third cranial nerve palsy? Klin Monbl Augenheilkd. 2010;227:862-3.
- [Google Scholar]
- Simultaneous involvement of third and sixth cranial nerve in a patient with lyme disease. Neuroradiology. 2003;45:85-7.
- [Google Scholar]
- Achard-Lévi syndrome: Pupil-sparing oculomotor nerve palsy due to midbrain stroke. Cerebrovasc Dis. 2003;16:109-10.
- [Google Scholar]
- Oculomotor nerve palsy and diffuse large B cell lymphoma. Acta Neurol Belg. 2017;117:743-4.
- [Google Scholar]
- Dissection of extracranial arteries supplying the brain. Dtsch Med Wochenschr. 2000;125:1333-6.
- [Google Scholar]
- Ophtho Book: The Free Eye Book and Lecture Series. Available from: https://timroot.com/ophthobook/
- Bilateral tonic pupils secondary to Ross syndrome: A case report. J Optom. 2014;7:106-7.
- [Google Scholar]
- Myasthenia gravis in ophthalomological practice. Z Prakt Augenheilkd. 2006;27:433-40.
- [Google Scholar]
- Optic disc swelling: A compilation of relevant differential diagnoses. Ophthalmologe. 2016;113:967-81.
- [Google Scholar]
- Intravenous thrombolysis with low-dose recombinant tissue plasminogen activator in central retinal artery occlusion. Am J Ophthalmol. 2008;146:700-6.
- [Google Scholar]
- Progression of optic neuritis to multiple sclerosis: An 8-year follow-up study. Clin Neurol Neurosurg. 1999;101:189-92.
- [Google Scholar]
- The eye in neurology: Evaluation of sudden visual loss and diplopia – Diagnostic pointers and pitfalls. Ann Acad Med Singapore. 2001;30:143-7.
- [Google Scholar]
- Neurogenic vision loss: Causes and outcome. An experience from a tertiary center in northern India. J Neurosci Rural Pract. 2014;5:340-8.
- [Google Scholar]
- De Myer's the Neurologic Examination, a Programmed Text (6th ed). New York: McGraw Hill; 2011.
- Performing a Standard Eye Examination in Neurology. Eye Movement Disorders Information Center. Available from: http://www.neurocular.com/
- [Google Scholar]
- The language of neurology: Symptoms, signs and basic investigation. In: Clarke C, Howard R, Rossor M, Shorvon S, eds. Neurology: A Queen Square Textbook. Oxford: Blackwell; 2009. p. :75-107.
- [Google Scholar]
- Acute diplopia: Differential diagnosis and treatment options. Klin Monbl Augenheilkd. 2017;234:1348-53.
- [Google Scholar]
- Neurogenic diplopia: Paralysis of cranial nerves III, IV, and VI. Optom Clin. 1996;5:53-76.
- [Google Scholar]
- Clinical approach to supranuclear brainstem saccadic gaze palsies. Front Neurol. 2017;8:429.
- [Google Scholar]
- Slowing of number naming speed by King-Devick test in Parkinson's disease. Parkinsonism Relat Disord. 2014;20:226-9.
- [Google Scholar]
- The King-Devick (K-D) test of rapid eye movements: A bedside correlate of disability and quality of life in MS. J Neurol Sci. 2014;343:105-9.
- [Google Scholar]
- Mobile universal lexicon evaluation system (MULES) test: A new measure of rapid picture naming for concussion. J Neurol Sci. 2017;372:393-8.
- [Google Scholar]
- The diagnostic value of saccades in movement disorder patients: A practical guide and review. J Clin Mov Disord. 2015;2:14.
- [Google Scholar]
- Internuclear and supranuclear disorders of eye movements: Clinical features and causes. Eur J Neurol. 2009;16:1265-77.
- [Google Scholar]
- Klinisch-Neurologische Untersuchungstechniken. Stuttgart: Thieme Verlag; 2012.
- Diagnostic accuracy of confrontation visual field tests. Neurology. 2011;76:1192-3.
- [Google Scholar]
- The demise of direct ophthalmoscopy: A modern clinical challenge. Neurol Clin Pract. 2015;5:150-7.
- [Google Scholar]
- Nonmydriatic retinal photography in the evaluation of acute neurologic conditions. Neurol Clin Pract. 2013;3:527-31.
- [Google Scholar]
- Diagnostic accuracy and use of nonmydriatic ocular fundus photography by emergency physicians: Phase II of the FOTO-ED study. Ann Emerg Med. 2013;62:28-33.
- [Google Scholar]
- Nonmydriatic ocular fundus photography in neurologic emergencies. JAMA Neurol. 2015;72:455-9.
- [Google Scholar]
- Vision disorders in retrochiasmatic lesions of the visual pathways. Ther Umsch. 1996;53:31-6.
- [Google Scholar]
- Central vision disorders – Visual phenomena caused by lesions of the primary visual cortex and associated regions. Klin Monbl Augenheilkd. 2009;226:R51-70.
- [Google Scholar]
- Combination of attentional and spatial working memory deficits in Bálint-Holmes syndrome. Ann N Y Acad Sci. 2015;1339:165-75.
- [Google Scholar]
- The Neurology of Vision. Oxford: Oxford University Press; 2001.
- Charles Bonnet's syndrome: Not only a condition of the elderly. Graefes Arch Clin Exp Ophthalmol. 2016;254:1637-42.
- [Google Scholar]
- Utility of red Amsler grid screening in a rheumatology clinic. J Rheumatol. 2004;31:1754-5.
- [Google Scholar]
- Is there a role for optokinetic nystagmus testing in contemporary orthoptic practice? Old tricks and new perspectives. Am Orthopt J. 2014;64:1-10.
- [Google Scholar]
- Headache medicine meets neuro-ophthalmology: Exam techniques and challenging cases. Headache. 2013;53:703-16.
- [Google Scholar]
- Neuro-ophthalmological emergencies: Which ocular signs or symptoms for which diseases? Acta Neurol Belg. 2013;113:215-24.
- [Google Scholar]
- The Neuro-Ophthalmology Virtual Education Library. Available from: http://www.novel.utah.edu/
- 2014. Continuum, Lifelong Learning in Neurology, Neuro-ophthalmology. 20 Available from: http://www.journals.lww.com/continuum/toc/2014/08000
- Ebrain: An e-learning resource supporting training in the clinical neurosciences. Available from http://www.ebrain.net/
- Teaching neuroImages: Unmasking raccoon eyes: A classic clinical sign. Neurology. 2014;83:e58-9.
- [Google Scholar]
- Images in clinical medicine. Bilateral internuclear ophthalmoplegia in multiple sclerosis. N Engl J Med. 2013;368:e3.
- [Google Scholar]
- Effects of peer-assisted training during the neurology clerkship: A randomized controlled study. Eur J Neurol. 2008;15:1365-70.
- [Google Scholar]
- OSCE in the neurology clerkship. Experiences at the neurological department of the university hospital Erlangen. Fortschr Neurol Psychiatr. 2009;77:32-7.
- [Google Scholar]
- Introducing neurological examination for medical undergraduates – How I do it. Pract Neurol. 2013;13:49-50.
- [Google Scholar]
- A systematic review of best practices in teaching ophthalmology to medical students. Surv Ophthalmol. 2016;61:83-94.
- [Google Scholar]
- Optic disc assessment in the emergency department: A comparative study between the PanOptic and direct ophthalmoscopes. Emerg Med J. 2012;29:1007-8.
- [Google Scholar]
- Laser scanning tomography of the optic nerve vs CSF opening pressure in idiopathic intracranial hypertension. Neurology. 2004;62:1221-3.
- [Google Scholar]
- The contribution of optical coherence tomography in neuromyelitis optica spectrum disorders. Front Neurol. 2017;8:493.
- [Google Scholar]
- Pattern of neuro-ophthalmic disorders in a tertiary eye centre in Nigeria. Niger J Clin Pract. 2007;10:147-51.
- [Google Scholar]






