Translate this page into:
Minimally Invasive versus Open Spine Surgery: What Does the Best Evidence Tell Us?
Address for correspondence: Dr. Shearwood McClelland III, Department of Orthopaedic Surgery, Spine Research Institute, NYU Hospital for Joint Diseases, 306 East 15th Street, Ground Floor, New York, NY 10003, USA. E-mail: drwood@post.harvard.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Spine surgery has been transformed significantly by the growth of minimally invasive surgery (MIS) procedures. Easily marketable to patients as less invasive with smaller incisions, MIS is often perceived as superior to traditional open spine surgery. The highest quality evidence comparing MIS with open spine surgery was examined.
Methods:
A systematic review of randomized controlled trials (RCTs) involving MIS versus open spine surgery was performed using the Entrez gateway of the PubMed database for articles published in English up to December 28, 2015. RCTs and systematic reviews of RCTs of MIS versus open spine surgery were evaluated for three particular entities: Cervical disc herniation, lumbar disc herniation, and posterior lumbar fusion.
Results:
A total of 17 RCTs were identified, along with six systematic reviews. For cervical disc herniation, MIS provided no difference in overall function, arm pain relief, or long-term neck pain. In lumbar disc herniation, MIS was inferior in providing leg/low back pain relief, rehospitalization rates, quality of life improvement, and exposed the surgeon to >10 times more radiation in return for shorter hospital stay and less surgical site infection. In posterior lumbar fusion, MIS transforaminal lumbar interbody fusion (TLIF) had significantly reduced 2-year societal cost, fewer medical complications, reduced time to return to work, and improved short-term Oswestry Disability Index scores at the cost of higher revision rates, higher readmission rates, and more than twice the amount of intraoperative fluoroscopy.
Conclusion:
The highest levels of evidence do not support MIS over open surgery for cervical or lumbar disc herniation. However, MIS TLIF demonstrates advantages along with higher revision/readmission rates. Regardless of patient indication, MIS exposes the surgeon to significantly more radiation; it is unclear how this impacts patients. These results should optimize informed decision-making regarding MIS versus open spine surgery, particularly in the current advertising climate greatly favoring MIS.
Keywords
Lumbar spine fusion
microdiscectomy
minimally invasive spine surgery
open spine surgery
randomized controlled trials
INTRODUCTION
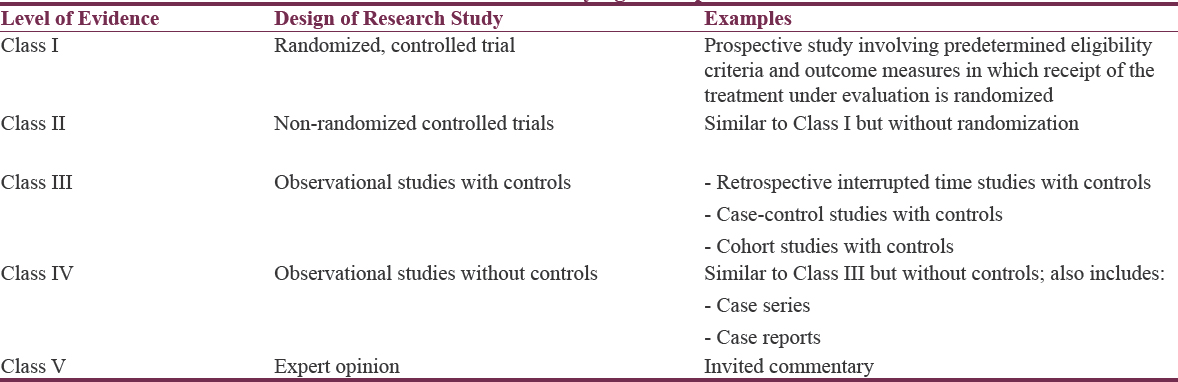
Research studies provide an objective method of evaluating the efficacy of medical and surgical therapies. The degree to which a study influences management is related to the level of evidence that it provides. There are generally five classes of evidence within which research studies fall, which are listed in Table 1. Of these classes, Class I evidence – derived from a prospective randomized controlled trial (RCT) – is the most powerful in assessing the virtue of a particular treatment modality. This review examines the existing highest quality evidence examining minimally invasive surgery (MIS) versus conventional open surgery for three procedures: Cervical disc herniation, lumbar disc herniation, and posterior lumbar fusion. Literature searches were made systematically using the Entrez gateway of the PubMed database for articles published in English up to and through December 28, 2015.
Minimally invasive surgery versus conventional open surgery: Cervical disc herniation
Five studies of Class I evidence were found examining MIS versus conventional open surgery in treating cervical disc herniation. These comprised four RCTs – two conducted in Germany, one in Korea, and one in Egypt and one systematic review examining studies up to January 12, 2014.[12345] The RCTs comprised a total of 219 MIS patients and 212 open surgery patients, with long-term follow-up ranging from 104 to 121 weeks.
Of note, the open surgery group was comprised discectomy without fusion in only one of the four RCTs, comprising 19 of the 212 open surgery patients (9%).[14] The remaining 193 open surgery patients received fusion as well as discectomy through anterior cervical discectomy and fusion.[235] In contrast, only 37 of the 219 MIS patients (17%) received fusion, whereas 100 of the remaining 182 MIS patients received posterior foraminotomy.[125] Of the remaining 82 MIS patients, 60 underwent anterior cervical discectomy, whereas 22 received either foraminotomy or discectomy (specific procedure per patient not reported).[34]
With regard to operative approach, only 97 of the 219 MIS patients (44%) in RCTs underwent an anterior approach, whereas 193 of the 212 conventional open patients (91%) in RCTs underwent an anterior approach.[1]
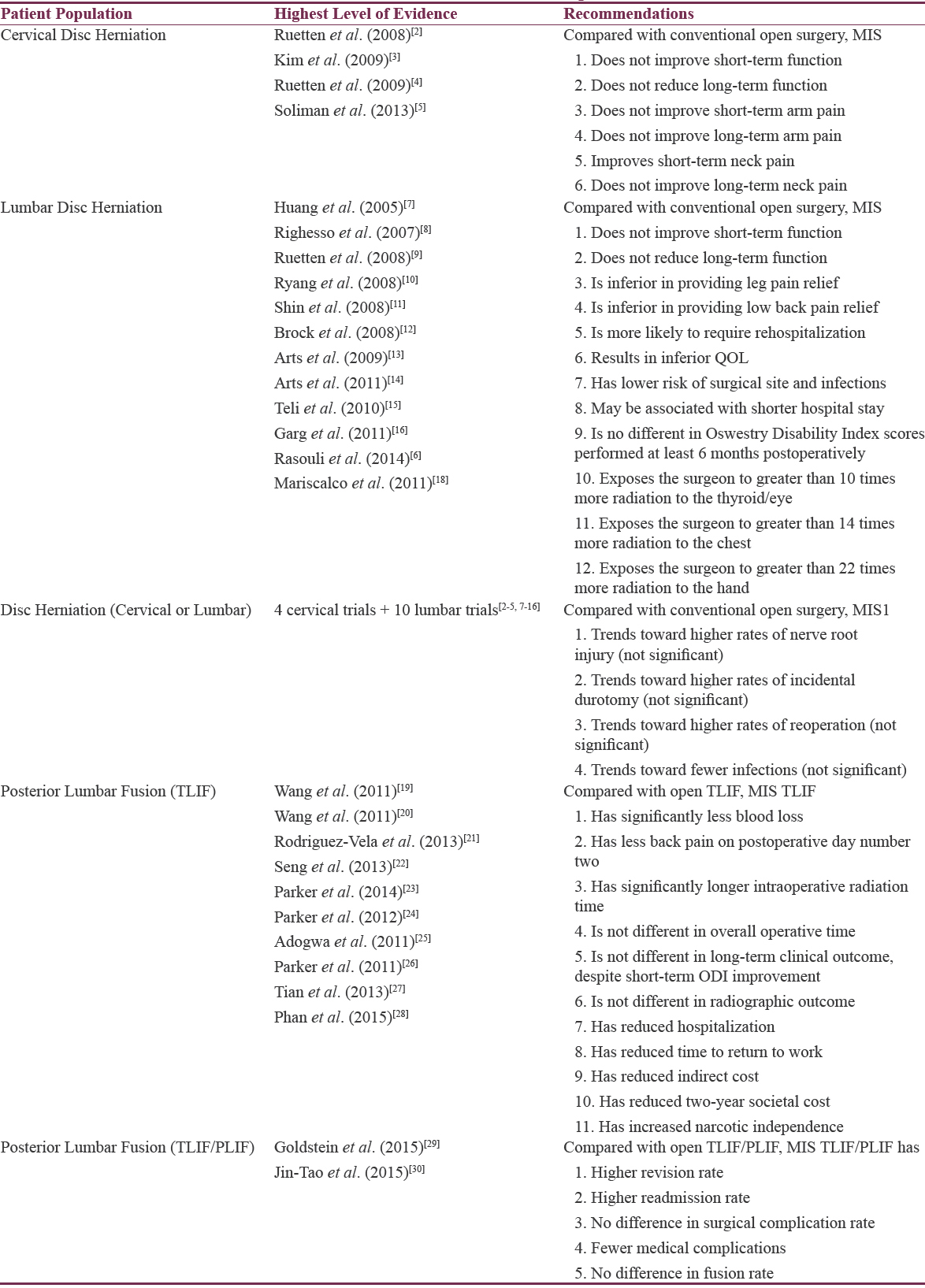
The collective results of these RCTs [Table 2] indicate that compared with conventional open surgery for cervical disc herniation, MIS does not improve function (short- or long-term), arm pain (short- or long-term), or long-term neck pain. MIS did improve short-term neck pain, but this finding was not significant when included in the pooled estimate analysis including lumbar cases.[1]
Minimally invasive surgery versus conventional open surgery: Lumbar disc herniation
Twelve studies of Class I evidence were found examining MIS versus conventional open surgery in treating lumbar disc herniation. These were comprised ten RCTs and two systematic reviews.[1678910111213141516] The ten RCTs comprised a total of 586 MIS patients and 573 conventional open patients. No patients in either group received fusion. All 573 open patients received discectomy, whereas 564 of the 586 MIS patients received discectomy; the remaining 22 MIS patients (4%) received percutaneous nucleotomy. Eight of the ten RCTs had follow-up longer than 1 week; in these studies, follow-up ranged from 52 to 104 weeks.
The collective results of these studies [Table 2] indicated that MIS was inferior to conventional open surgery for lumbar disc herniation with regard to leg pain relief, low back pain relief, quality-of-life, and rehospitalization rate (due to increased disc reherniation).[6] However, MIS was associated with lower risk of infection and shorter hospital stay.[6] There was no difference in short-term function, long-term function, or 6-month postoperative Oswestry Disability Index (ODI) scores.[16]
A recent nonrandomized study examining operating field sterility between MIS and open lumbar microdiscectomy found no difference in colony counts between MIS and open cases; the authors, therefore, conclude that any decreased rate of infection reported for MIS may be related to extraoperative factors such as patient selection and postoperative care.[17]
The issue of radiation exposure to the surgeon was addressed in one Class II in vivo prospective study comparing radiation exposure during ten MIS versus ten open lumbar microdiscectomy cases.[17] MIS resulted in more than 10 times the radiation to the thyroid/eye of the surgeon, 14 times more radiation to the chest of the surgeon, and 22 times more radiation to the surgeon's hand compared with open surgery [Table 2].[18]
Minimally invasive surgery versus conventional open surgery: Disc herniation (cervical or lumbar)
One systematic review performed a pooled analysis of cervical and lumbar disc herniations from 14 RCTs. Compared with conventional open surgery, MIS trended toward decreased infection, but increased nerve root injury, durotomy, and reoperation rates; however, none proved statistically significant [Table 2].[1]
Minimally invasive surgery versus conventional open surgery: Posterior lumbar fusion
Three RCTs were found examining MIS versus open transforaminal lumbar interbody fusion (TLIF).[192021] In the first study (52 patients; 25 MIS versus 27 open), MIS compared to open surgery revealed no difference in operative time, clinical results, or radiographic results; mean follow-up was 27.5 months (range = 12–38 months). However, MIS patients had significantly less blood loss, significantly less back pain on postoperative day 2 but had significantly longer intraoperative radiation time.[19] An important caveat of this study is that all patients had previously undergone open lumbar spine surgery before randomization. The second study involved 79 patients (41 MIS, 38 open) with single-level degenerative lumbar spine disease who had no previous surgical treatment of segmental defects; mean follow-up was 32.7 months (range = 24–37 months).[20] Compared with open surgery, MIS was not significantly different with regard to operative time, blood loss, or postoperative hospital time. However, MIS had significantly less postoperative drainage and shorter postoperative recovery time (40 days versus 76 days) at the cost of more than twice the intraoperative fluoroscopy time. Visual analog scale (VAS) scores at 3, 6, 12, and 24 months postoperatively were not significantly different between the two groups, whereas the ODI was initially better in MIS but became insignificantly different at 12 and 24 months postoperatively.[20] The third study involved 41 patients (21 MIS, 20 open) with minimum 3-year follow-up (range = 36–54 months) who underwent single-level TLIF and found that despite improved functional status of the MIS TLIF group in the short-term, there were no clinically relevant differences from the open TLIF group when follow-up was performed at least 3 years postoperatively.[21]
Several prospective nonrandomized trials found MIS TLIF to be superior with regard to narcotic independence, 2-year societal cost, and accelerated return to work.[2223242526] A meta-analysis comprising one RCT, five prospective trials, and five retrospective trials found MIS to have similar operative time, complication rate, and reoperation rate, with MIS TLIF having less blood loss and shorter hospital stay at the cost of significantly increased X-ray exposure compared with open TLIF.[27] A second meta-analysis of 21 studies found MIS TLIF to have lower blood loss and infection rates with superior postoperative ODI and VAS back pain scores at the cost of higher radiation exposure for the surgical team.[28]
A recent systematic review including TLIF or posterior lumbar interbody fusion (PLIF) found equipoise in patient-reported clinical outcomes between MIS and open fusions, with equivalent rates of surgical complications but lower rates of medical complications in MIS.[29] Another recent meta-analysis comparing MIS TLIF to open TLIF/PLIF found the two procedures to have equivalent fusion rates and complications rates; however, the MIS group had both a higher revision rate and readmission rate.[30]
CONCLUSION
The highest levels of evidence do not support MIS over open surgery for either cervical or lumbar disc herniation. However, for fusion cases, MIS TLIF demonstrates advantages, most prominently in reduced hospitalization, societal cost, and time to return to work at the cost of higher revision and readmission rates. There has yet to be a RCT comparing MIS TLIF solely with open PLIF, which would provide useful information.
Regardless of patient indication, MIS results in significantly more radiation exposure to the surgeon, particularly in surgery involving the lumbar spine. It is unclear whether this exposure impacts patients as well, and this area certainly deserves further study.
These results from an analysis of the current highest levels of evidence should be made clear to patients to give them the best chance to make an informed decision when choosing MIS versus open spine surgery, particularly given the current medical advertising climate which greatly favors the choice of MIS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Minimally invasive versus open surgery for cervical and lumbar discectomy: A systematic review and meta-analysis. CMAJ Open. 2014;2:E295-305.
- [Google Scholar]
- Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: A prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:940-8.
- [Google Scholar]
- Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Int Orthop. 2009;33:1677-82.
- [Google Scholar]
- Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: Results of a randomized controlled study. J Korean Med Sci. 2009;24:649-53.
- [Google Scholar]
- Cervical microendoscopic discectomy and fusion: Does it affect the postoperative course and the complication rate? A blinded randomized controlled trial. Spine (Phila Pa 1976). 2013;38:2064-70.
- [Google Scholar]
- Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;9:CD010328.
- [Google Scholar]
- Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res. 2005;23:406-11.
- [Google Scholar]
- Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: Results of a randomized controlled trial. Neurosurgery. 2007;61:545-9.
- [Google Scholar]
- Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:931-9.
- [Google Scholar]
- Standard open microdiscectomy versus minimal access trocar microdiscectomy: Results of a prospective randomized study. Neurosurgery. 2008;62:174-81.
- [Google Scholar]
- The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39-43.
- [Google Scholar]
- Lumbar microdiscectomy: Subperiosteal versus transmuscular approach and influence on the early postoperative analgesic consumption. Eur Spine J. 2008;17:518-22.
- [Google Scholar]
- Leiden-The Hague Spine Intervention Prognostic Study Group (SIPS). Tubular diskectomy vs. conventional microdiskectomy for sciatica: A randomized controlled trial. JAMA. 2009;302:149-58.
- [Google Scholar]
- Tubular diskectomy vs. conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. 2011;69:135-44.
- [Google Scholar]
- Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443-50.
- [Google Scholar]
- Microendoscopic versus open discectomy for lumbar disc herniation: A prospective randomised study. J Orthop Surg (Hong Kong). 2011;19:30-4.
- [Google Scholar]
- Comparison of operating field sterility in open versus minimally invasive microdiscectomies of the lumbar spine. Surg Neurol Int. 2013;4(Suppl 5):S295-8.
- [Google Scholar]
- Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: A prospective, controlled trial. Spine (Phila Pa 1976). 2011;36:255-60.
- [Google Scholar]
- Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011;20:623-8.
- [Google Scholar]
- Minimally invasive lumbar interbody fusion via MAST quadrant retractor versus open surgery: A prospective randomized clinical trial. Chin Med J (Engl). 2011;124:3868-74.
- [Google Scholar]
- Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Eur Spine J. 2013;22:2857-63.
- [Google Scholar]
- Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: A matched-pair comparison study. Spine (Phila Pa 1976). 2013;38:2049-55.
- [Google Scholar]
- Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: Comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82:230-8.
- [Google Scholar]
- Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. 2012;78:178-84.
- [Google Scholar]
- Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24:479-84.
- [Google Scholar]
- Post-operative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): Literature review and cost analysis. Minim Invasive Neurosurg. 2011;54:33-7.
- [Google Scholar]
- Minimally invasive versus open transforaminal lumbar interbody fusion: A meta-analysis based on the current evidence. Eur Spine J. 2013;22:1741-9.
- [Google Scholar]
- Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: Systematic review and meta-analysis. Eur Spine J. 2015;24:1017-30.
- [Google Scholar]
- Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: Meta-analysis and systematic review. J Neurosurg Spine. 2016;24:416-27.
- [Google Scholar]
- Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: A meta-analysis. Eur Spine J. 2015;24:1058-65.
- [Google Scholar]






