Translate this page into:
Minimally Invasive Sacroiliac Fixation for Extension of Fusion in Cases of Failed Lumbosacral Fusion
Address for correspondence: Dr. Mazda K. Turel, Department of Neurosurgery, Rush University Medical Center, 1725 W Harrison Street, Suite 855. E-mail: mazdaturel@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Sacroiliac fusion and instrumentation extension for correction of failed lumbosacral fusions traditionally requires a long revision surgery. Reopening of the prior surgical incision to expose the prior instrumentation requires a large incision with increased blood loss, increased operative time, increased risk of infection, and longer hospitalization times. We describe the first case series using a minimally invasive surgical sacroiliac screw technique for extension of a prior fusion to the pelvis. Using two small 3-cm paramedian incisions on each side, we were able to obtain autologous iliac crest bone graft, place the sacroiliac screw minimally invasive, perform an arthrodesis, and connect the prior surgical hardware to the sacroiliac screw safely. A detailed review of surgical technique, clinical cases, and brief review of the literature is discussed.
Keywords
Minimally invasive spine surgery
pseudoarthrosis
sacroiliac fusion
INTRODUCTION
The incidence of instrumented fusion for degenerative and other lumbosacral pathology has increased. The instrumentation for fusions of the lower lumbar spine and sacrum has a well-defined failure rate.[12] Fusion failure rates are especially prevalent at L5/S1 where the S1 pedicle is large, and pedicle screw fixation may lack the cortical purchase found at other levels. The rate of pseudoarthrosis depends on the number of levels fused, the type of fusion, and the medical risk factors such as tobacco use.[3] Revision surgery typically involves a long-segment fusion with the extension of the instrumentation to the pelvis. Pelvic fixation is sometimes necessary because pelvic screws have a large diameter and length and can be placed safely as a distal anchor. Pelvic screws extend anterior to the spine in the sagittal plane and lateral to the spine in the coronal plane.[4] The placement of pelvic fixation has traditionally been done using a very large open method, exploring the previous incision, and is associated with a longer hospital stay, greater blood loss, and prolonged operative time.[5] The lateral entry point for pelvic screws requires extensive open dissection. In our described technique, we describe two patients with pseudoarthrosis after previous long segment lumbosacral fusion requiring an extension of their instrumentation to the pelvis. The surgical technique allows for a significantly decreased incision size and operative morbidity.
CASE REPORTS
Case 1
The patient is a 63-year-old man who had a prior fusion from T10 to S1, 3 years ago and an L5–S1 ALIF (anterior lumbar interbody fusion) 1 year ago, now presented with difficulty in walking for a few months and required the aid of a walker to walk. He had debilitating low back pain and had failed nonoperative treatment including physical therapy and epidural injections. The patient was on multiple narcotic pain medications. On examination, he was unable to stand upright and was bent forward. Power was grade 5 in all muscle groups, except right dorsiflexion, which was grade 4. He had reduced sensations in both L5-S1 dermatomes. The plain radiographs showed loss of sagittal balance. The computed tomography (CT) scan showed a pseudoarthrosis at L5-S1. There was lucency around the S1 screw and dissociation of the rod from S1. The magnetic resonance imaging, in addition, showed a right L5-S1 foraminal stenosis [Figure 1]. Discussion of an extension surgery involving a pedicle subtraction osteotomy at L3 and instrumentation to the ileum with its risks and benefits was discussed although the patient declined given the risks and his medical comorbidities.
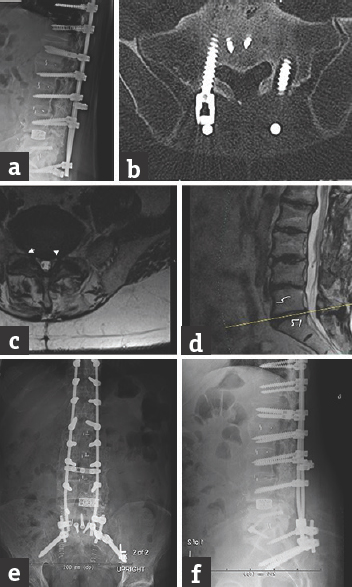
- (a) Lateral radiograph and (b) axial computed tomography of a patient with a previous long-segment lumbosacral fusion with pseudoarthrosis as evidenced by the left S1 screw lucency. (c) Axial and (d) sagittal magnetic resonance imaging showing residual foraminal stenosis at L5-S1. (e) Anteroposterior and (f) lateral postoperative radiograph after minimally invasive extension of the fusion to the pelvis
Surgical technique
The L5/S1 levels were localized using fluoroscopy. Two paramedian incisions were made in the midline measuring 3 cm in length. The incisions were made using anteroposterior fluoroscopy to localize the distal end of the instrumentation and extended cephalad. The monopolar cautery was used to extend the incision through the posterior lumbar fascia. The facet and transverse process of L5/S1 were exposed in a subperiosteal fashion. Retractors were introduced. The rods were identified from the previous construct. The monopolar cautery was used to identify the crest, and a Leksell rongeur was used to remove cortical bone. A curette was used to remove more cancellous bone graft.
The right-sided S1 screw was then identified and was not connected to the rod. The set screw was removed, and the screw was removed. Each iliac crest was cannulated, tapped, and sounded to ensure no cortical breach. We then placed 9 mm × 80 mm long screws. Anteroposterior and teardrop view fluoroscopy was used to help in pedicle screw placement. A short 40 mm rod was then secured to the new iliac screw, and a cross-connector was used to connect the rod to the existing hardware/rod. We decorticated the transverse process of L5, sacral ala, and ileum and then medial lamina and then placed an iliac crest autograft as well as cancellous allograft chips and bone autograft derived from morselized spinous process and facets to achieve a posterolateral arthrodesis at L5/S1 and the sacrum-ileum area.
The patient had a dramatic improvement in pain. He was discharged home on postoperative day #1. He was readmitted 6 weeks later for a superficial wound infection with cultures growing Escherichia coli and treated effectively with oral ciprofloxacin.
Case 2
The patient was a 42-year-old female underwent a prior L2-S1 fusion following which she had transient improvement. She had a recurrence of bilateral leg pain for a few months. She had failed nonoperative treatment including physical therapy, pain medication, and epidural injections. On examination, she had no neurological deficits but had sacroiliac tenderness. Imaging showed lumbar spondylosis and pseudoarthrosis at L5-S1 with lucency around the S1 screws [Figure 2]. She had some abnormality of the sacrum with incomplete fusion around the left facet and an L5/L6 transitional level.
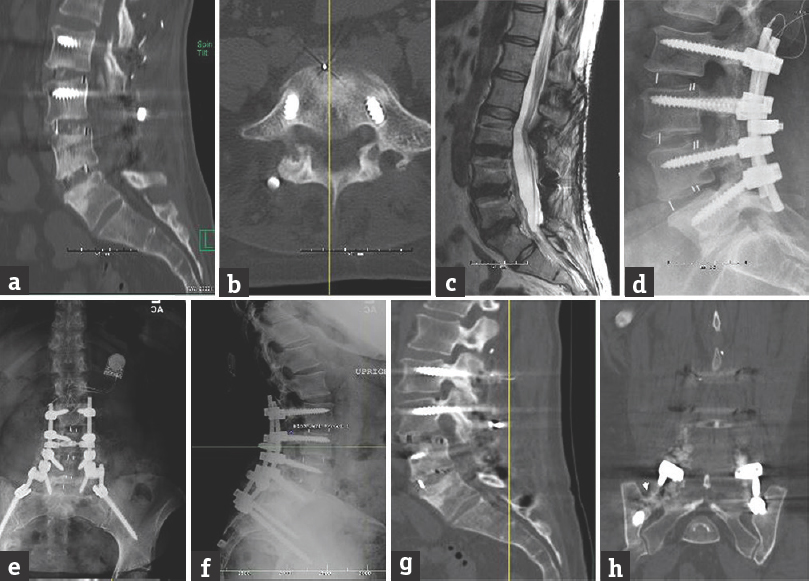
- Preoperative (a and b) computed tomography scan and (c and d) magnetic resonance imaging of a patient with a previous lumbosacral fusion with evidence of pseudoarthrosis. (e) Anteroposterior and (f) lateral postoperative radiograph after minimally invasive extension of the fusion to the pelvis. Six months’ postoperative (g) sagittal and (h) coronal computed tomography scan showing evidence of fusion from the pelvis to L5
Surgical technique
The L5/S1 levels were localized using fluoroscopy. Two Wiltse type incisions were made measuring 3 cm in length. Anteroposterior fluoroscopy was used to make the incision centered on the caudal end of the instrumentation. The monopolar cautery was used to extend the incision through the posterior lumbar fascia. The facet and transverse process of L5/S1 were exposed in a subperiosteal fashion. Retractors were introduced. The previous instrumentation was identified, and the caudal rods were exposed. Pseudoarthrosis and scar were curetted and removed to expose the underlying L5/S1 facet joint and transverse process of L5 and sacral alae. The iliac crest was then exposed. Some bone was removed and used as autograft from the iliac crest.
The entry point for the iliac crest screws was identified. We used a gearshift, and we placed 9 mm × 80 mm long screws. Fluoroscopy was used to help in pedicle screw placement. Views included the “tear-drop” view and inlet and pelvic outlet views. On both sides, a side-to-side rod connector was used and connected to 40 mm rods that extended to the pelvic screws. Rods were then contoured and secured using blockers. A counter-torque was used, and final tightening applied. Fluoroscopy demonstrated good instrumentation placement. We decorticated the transverse process at L5, sacral ala, and the ileum and then medial lamina. We then placed cancellous allograft chips and bone autograft derived from morselized crest and facets to achieve a posterolateral arthrodesis at L5/S1 and an open sacral to iliac crest/pelvic fusion. The patient was discharged home on postoperative day #1.
The patient had equivocal improvement in pain, and her CT showed fusion at 6 months extending from L5 to the ileum.
DISCUSSION
Despite advances in techniques of lumbosacral fixation, pseudoarthrosis at the lumbosacral junction is not an uncommon problem. This is partly due to a large pedicle of the sacrum which often provides less rigid fixation and increased shear forces at the L5-S1 interspace.[6] Complications related to pseudoarthrosis such as screw pull out and implant failure are particularly seen in long fusion constructs ending across the lumbosacral junction, as demonstrated in both our cases. The treatment options for dealing with a failed lumbosacral fusion include anterior L5-S1 interbody fusion, minimally invasive L5-S1 interbody fusions, lumbosacral pedicle screw placement, sacroiliac fusion, and sacro-alar-iliac screw placement.
Minimally invasive techniques for sacroiliac fixation have been well described in cases of trauma and sacral insufficiency fractures either due to osteoporosis or metastasis.[789]
Ohya et al.[10] described a technique of S-2 alar-iliac (S2AI) screw fixation in two patients – one case was a sacral insufficiency fracture following a long-segment fusion in a patient with a transitional S-1 vertebra and the other case involved pseudarthrosis following lumbosacral fixation. They claim that S2AI screws offer rigid fixation, are low profile, and allow easy connection to the lumbosacral rod. Martin et al.[11] had previously described a minimally invasive approach for this technique that allows percutaneous insertion of the screws; however, it was not for prior lumbosacral fusion but in patients with sacral fractures due to metastasis. Similarly, Wang et al.[1213] have described the placement of percutaneous iliac screws for adult degenerative deformity. However, these were not revision cases, which required an extension of previously, failed instrumentation.
Our technique [Figures 3 and 4] utilizes paramedian incisions with subfascial exposure of the facet and transverse process. The iliac crest screws are inserted under fluoroscopic-guided direct vision. Side-to-side connectors and a short adjunct rod connect the new screw to the existing rod, obviating the need for removal of the previous instrumentation. The exposure of the facet and transverse process allows for bone graft material to be layered promoting fusion at the fixation site. As with other minimally invasive techniques due to limited soft-tissue dissection, this is likely to result in less blood loss, lower infection rates, reduced postoperative pain, and a more rapid postoperative recovery than that associated with the more widely used open techniques.

- An illustration of bilateral paramedian incisions depicting exposure of only the lower end of the long segment fusion construct to facilitate sacroiliac fixation
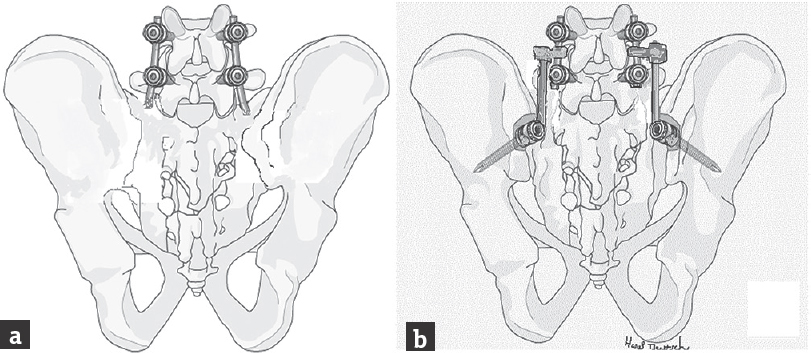
- (a) The previous instrumentation extending down to S1 is noted. (b) The side connectors connect a rod, which is then secured to the two iliac screws placed
Financial support and sponsorship
There are no conflicts of interest.
Conflicts of interest
Dr. Deutsch receives consulting royalties from RTI Surgical, Inc.
REFERENCES
- Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976). 2004;29:1996-2005.
- [Google Scholar]
- Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27:776-86.
- [Google Scholar]
- Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976). 2006;31:S80-8.
- [Google Scholar]
- Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976). 2002;27:818-24.
- [Google Scholar]
- Introduction to lumbosacral and sacropelvic fixation strategies. Neurosurg Focus. 2016;41(Video Suppl 1):1.
- [Google Scholar]
- Percutaneous S2 alar iliac fixation for pelvic insufficiency fracture. Orthopedics. 2014;37:e1033-5.
- [Google Scholar]
- Feasibility of minimally invasive sacropelvic fixation: Percutaneous S2 alar iliac fixation. Spine (Phila Pa 1976). 2010;35:460-4.
- [Google Scholar]
- Percutaneous ilio-sacral screw fixation in supine position under fluoroscopy guidance. Kathmandu Univ Med J (KUMJ). 2015;13:56-60.
- [Google Scholar]
- Technique and nuances of an S-2 alar iliac screw for lumbosacral fixation in patients with transitional and normal anatomy. Neurosurg Focus. 2016;41 Video(Suppl 1):1.
- [Google Scholar]
- Sacropelvic fixation: Two case reports of a new percutaneous technique. Spine (Phila Pa 1976). 2011;36:E618-21.
- [Google Scholar]
- Percutaneous iliac screws for minimally invasive spinal deformity surgery. Minim Invasive Surg 2012 2012:173685.
- [Google Scholar]
- Minimally invasive percutaneous iliac screws: Initial 24 case experiences with CT confirmation. Clin Spine Surg. 2016;29:E222-5.
- [Google Scholar]






