Translate this page into:
Migration of Self-Introduced Acupuncture Needle into the Brainstem
Address for correspondence: Dr. Shadi El-Wahsh, Department of Neurosurgery, Liverpool Hospital, Locked Bag 7130, Liverpool BC, New South Wales 1871, Australia. E-mail: selwahsh@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acupuncture-related injuries to the central nervous system are a rare but well-documented occurrence. This report describes the case of a self-introduced acupuncture needle migrating into the brainstem following an initial failed attempt at surgical extraction. The patient displayed no neurological deficits, and the needle was eventually successfully removed under direct vision intraoperatively. We discuss the role of various imaging modalities in pre- and post-operative assessment of penetrating foreign bodies in the brainstem. We also discuss the options available for the management of such foreign bodies, including possible approaches for operative intervention, and the risks involved with both surgical and conservative management.
Keywords
Acupuncture
brainstem
foreign body
needle
INTRODUCTION
Injury to the central nervous system is a rare but serious complication of acupuncture.[1] The majority of such injuries involve the spinal cord; although rarely, direct injury to the brainstem has been reported. Abumi et al. were the first to describe a case of brainstem injury following acupuncture: a 60-year-old patient presented with motor and sensory deficits to the right upper extremity nearly 18 years after undergoing acupuncture needle treatment.[2] The needle was removed surgically, and the patient made a complete neurological recovery. More recently, Hama and Kaji described the case of a 70-year-old man presenting with left facial paraesthesia following the migration of an acupuncture needle into the medulla. In this case, the decision was made not to surgically remove the needle because of treatment-related risks.[3] Our report describes the first case of a self-introduced acupuncture needle migrating into the brainstem following a failed initial surgical attempt at extraction.
CASE REPORT
History and examination
A elder right-handed male remove query presented to the emergency department of a district hospital after a needle he was using to perform self-acupuncture broke off in the right posterior aspect of his neck due to incorrect withdrawal of the needle after it became bent. He could not retrieve the broken needle as it immediately became buried subcutaneously. In the emergency department, a small palpable lump was felt in the right suboccipital area, but there was no sign of a needle or puncture mark. The patient was pain-free and displayed no neurological deficits. Cervical spine X-rays showed the needle to be 8 mm deep in the soft tissues of the neck [Figure 1].
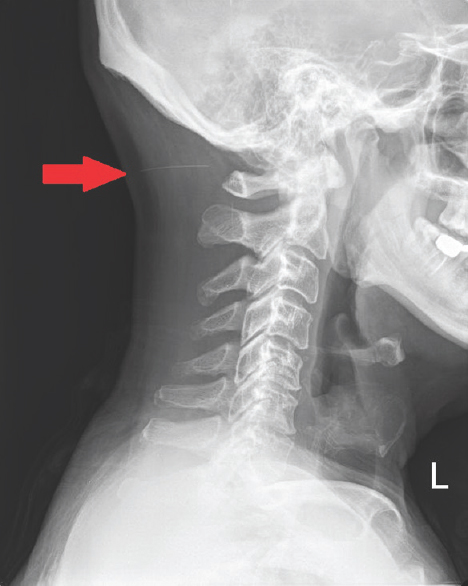
- Lateral neck plain radiograph showing the acupuncture needle (red arrow) in the posterior neck between the occipital bone and posterior arch of C1 at a depth of 8 mm from the skin
A first attempt to explore the neck under local anesthesia in the emergency department was unsuccessful. The patient subsequently underwent exploration of the neck under general anesthetic the following day by the general surgical team. Dissection down to the paraspinal muscles with the aid of intraoperative image intensification failed to identify the needle, and the procedure was abandoned. The needle could not be visualized with ultrasound, and so a computed tomography (CT) scan of the head and neck was obtained. This revealed that the needle had migrated cranially through the foramen magnum and had pierced the dura, with the tip resting within the dorsal brainstem [Figure 2]. At this point, 4 days after his initial presentation, the patient was transferred across to our neurosurgical unit with cervical spine immobilization for further management. He displayed no signs of meningism or any neurological deficits on examination.
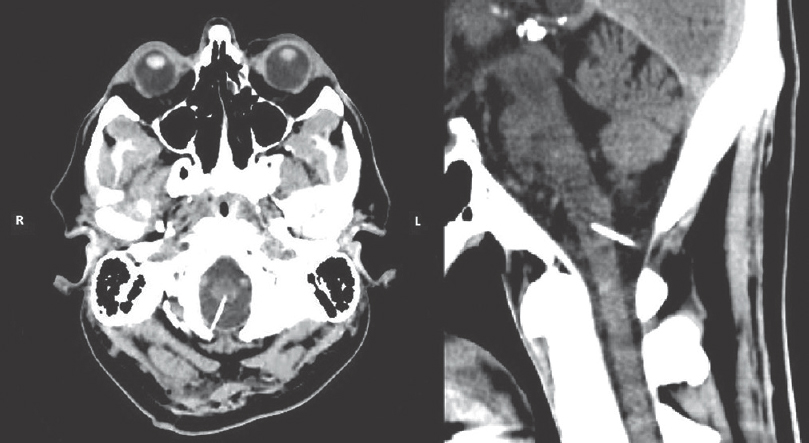
- Noncontrast computed tomography brain showing axial (left) and sagittal (right) views of the needle as it penetrates the brainstem. The needle crosses the midline, with the tip located along the anterolateral aspect of the medulla to the left of the midline
Operation
The decision was made to remove the acupuncture needle intraoperatively. A midline occipital craniectomy was performed to expose the dura with the needle passing through it. Given that the needle passed high above C1, the posterior arch of C1 was preserved. A durotomy was performed rostral to the entry site of the needle, revealing the needle to be passing through a superficial vessel on the dorsal surface of the medulla and into the brainstem parenchyma [Figure 2]. The needle was carefully removed without causing any bleeding. It was found to be a 0.25 mm × 30 mm stainless steel acupuncture needle, with its distal tip angulated medially in situ. The dura was carefully repaired with a synthetic dural patch and sealant to ensure no postoperative cerebrospinal fluid (CSF) leakage.
Postoperative course
The patient had an uneventful postoperative recovery and remained neurologically intact. He received intravenous antibiotics for 48 h and showed no clinical or biochemical signs of infection (WCC 7.0, CRP 4). A magnetic resonance imaging (MRI) brain performed 3 days postoperatively revealed the needle tract within the rostral medulla, without any evidence of tract hematoma or ischemic/traumatic parenchymal abnormalities [Figure 3]. The patient was discharged day 4 postoperatively on a course of oral antibiotics and remained asymptomatic at 1-month follow-up.

- T2-weighted axial magnetic resonance imaging showing angled needle tract mark (tip of red arrow) through the left dorsal medulla. No evidence of surrounding inflammation, ischemia, or hemorrhage
DISCUSSION
This case raises several key points regarding the assessment and management of acupuncture-related accidents and other penetrating injuries in the neck region. In the first instance, it is crucial to obtain CT imaging to assess the location and depth of the foreign body, thus guiding appropriate removal. In this case, the use of plain radiographs, intraoperative image intensification, and ultrasound were all unhelpful in locating the needle and led to an unsuccessful extraction attempt that most likely pushed the needle deeper and into the foramen magnum and brainstem. Penetrating injuries to the brainstem can cause a wide variety of neurological deficits depending on the location, size, and type of foreign body.[4] While our patient displayed no neurological deficits, the decision was made to surgically remove the needle to prevent complications such as further needle migration, vascular injury, and infection. Options for surgical removal included a “pull and see” approach without durotomy or removal of the needle under direct vision through durotomy. The latter approach was chosen to allow for immediate control of any bleeding during needle extraction. The dura was carefully repaired intraoperatively to minimize the risk of CSF leakage. Interestingly, a retrospective review of patients with penetrating spinal injuries showed that the development of CSF leaks was higher in patients who underwent intradural exploration compared to those managed conservatively.[5] However, given the location of the needle in the brainstem and the aforementioned risks, surgical removal with careful dural repair was preferred here. The risk of delayed meningitis and abscess formation was mitigated by the administration of antibiotics. Given that acupuncture is not practiced under sterile conditions, skin flora may likely have been introduced into the brain parenchyma. Monitoring for clinical and biochemical signs of infection is an important aspect of follow-up, as well as ongoing imaging to assess for the presence of delayed abscess formation.
Following removal of a penetrating foreign body within the brainstem, postoperative imaging is useful for assessing for tract hematoma, intra-/extra-axial hemorrhage, ischemic infarction, pseudoaneurysm formation, and CSF collection. MRI with magnetic resonance angiography is the imaging modality of choice postoperatively; this could not be performed preoperatively given the presence of a non-MRI compatible steel acupuncture needle.[6] Although not available in this case, the use of diffusion tensor imaging may have provided useful insights into the involvement of the major ascending/descending tracts within the brainstem. Given the location of the needle, it is possible that the tip traversed the dorsal columns among other important structures within the medulla. DTI has previously been utilized to assess spinal cord tract integrity following penetrating injuries,[7] and its use may have shed light on the lack of neurological deficits in this case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- Acupuncture: Does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755-64.
- [Google Scholar]
- Migration of an acupuncture needle into the medulla oblongata. Eur Spine J. 1996;5:137-9.
- [Google Scholar]
- Penetrating brain stem injury from crossbow bolt: A case report and review of the literature. Arch Emerg Med. 1990;7:224-7.
- [Google Scholar]
- Treatment of acute penetrating injuries of the spine: A retrospective analysis. J Trauma. 1989;29:42-6.
- [Google Scholar]
- Diffusion tensor tractography demonstration of partially injured spinal cord tracts in a patient with posttraumatic Brown Sequard syndrome. J Magn Reson Imaging. 2010;32:978-81.
- [Google Scholar]






