Translate this page into:
Mental Healthcare Delivery in Rural Greece: A 10-year Account of a Mobile Mental Health Unit
Address for correspondence: Dr. Vaios Peritogiannis, 1 Moulaimidou Street, Ioannina, Greece. E-mail: vaios.peritogiannis@medai.gr
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Patients living in rural and remote areas may have limited access to mental healthcare due to lack of facilities and socioeconomic reasons, and this is the case of rural areas in Eastern Europe countries. In Greece, community mental health service delivery in rural areas has been implemented through the development of the Mobile Mental Health Units (MMHUs).
Methods:
We present a 10-year account of the operation of the MMHU of the prefectures of Ioannina and Thesprotia (MMHU I-T) and report on the impact of the service on mental health delivery in the catchment area. The MMHU I-T is a multidisciplinary community mental health team which delivers services in rural and mountainous areas of Northwest Greece.
Results:
The MMHU I-T has become an integral part of the local primary care system and is well known to the population of the catchment area. By the end of 2016, the majority of patients (60%) were self-referred or family-referred, compared to 24% in the first 2 years. Currently, the number of active patients is 293 (mean age 63 years, 49.5% are older adults), and the mean caseload for each member of the team is 36.6. A significant proportion of patients (28%) receive care with regular domiciliary visits, and the provision of home-based care was correlated with the age of the patients. Within the first 2 years of operation of the MMHU I-T hospitalizations of treatment, engaged patients were reduced significantly by 30.4%, whereas the treatment engagement rates of patients with psychotic disorders were 67.2% in 5 years.
Conclusions:
The MMHU I-T and other similar units in Greece are a successful paradigm of a low-cost service which promotes mental health in rural, remote, and deprived areas. This model of care may be informative for clinical practice and health policy given the ongoing recession and health budget cuts. It suggests that rural mental healthcare may be effectively delivered by integrating generic community mental health mobile teams into the primary care system.
Keywords
Community mental health teams
economic crisis
mental healthcare
Mobile Mental Health Units
primary care
rural areas
INTRODUCTION
Patients living in rural and remote areas may have limited access to healthcare due to lack of facilities and socioeconomic reasons. For those underserved areas, a number of mobile health units have been developed throughout the world. Their impact on ease of access to healthcare, health outcomes of the served population, and patients’ satisfaction with this type of care has been recently reviewed[1] and it was found to be high.
Community mental health services are the cornerstone of mental health service delivery in developed countries. They were first introduced in the mid-fifties and expanded widely the following decades.[2] Those services gradually evolved to specialized and highly specialized teams and had become an alternative to inpatient mental health treatment. The effectiveness of those community interventions for severe mental illness has been supported by several studies, which have demonstrated that such care can reduce psychopathology, days of hospitalization, and comorbidity with substance abuse and can improve functioning and treatment adherence.[3] Community mental health services are thus an important component of current psychiatric practice and policy. However, the delivery of mental health services in rural and remote areas is still challenging and this is the case of rural areas in Eastern Europe countries, which do not receive adequate mental health care due to socioeconomic and geographical reasons and distant facilities.[4] With regard to Greece, it has been previously reported that several rural areas were mostly uncovered by mental healthcare facilities.[5]
In Greece, the mobile component of community mental health service delivery has been implemented through the development of the Mobile Mental Health Units (MMHUs). Early efforts were made in the early eighties,[6] and over the last decade, there was a tendency toward the introduction of such services in rural and remote areas of the mainland and in several of the numerous Greek islands. They were introduced with the aim of facilitating access to mental health services in those underserved areas of Greece.[7] The aim of this article is to present a 10-year account of the operation of the MMHU of a catchment area, namely the prefectures of Ioannina and Thesprotia (MMHU I-T); to report on the impact of the service on mental health delivery in the catchment area; and to stress the potential implications of such type of care for the contemporary mental health system.
METHODS
The catchment area
The MMHU I-T delivers services in a rural area of 5000 km2 with a population grossly estimated at 100,000 in Epirus, Northwest Greece [Figure 1]. This area is mostly mountainous, which makes access difficult, particularly in winter. It should be noted that Epirus is one of the poorest regions in the European Union,[8] with dispersed settlement structure. According to the 2011 census, almost one-third of the population in those rural areas is older adults.[9]

- The area of Epirus. Green color: The catchment area of the Mobile Menatl Health Unit of the Prefectures of Ioannina and Thesprotia (rural areas of the prefectures of Ioannina and Thesprotia). White color: Areas of the prefectures of Ioannina and Thesprotia not covered by the Mobile Mental Health Unit of the Prefectures of Ioannina and Thesprotia (urban and suburban areas). Gray color: Other prefectures of Epirus
The development of the Mobile Mental Health Unit of the Prefectures of Ioannina and Thesprotia
The MMHU I-T is being implemented by a nongovernmental organization, namely the Society for the Promotion of Mental Health in Epirus, and is financed by national resources. The provided services include diagnosis and evidence-based treatment, such as pharmacotherapy and psychotherapeutic interventions, as well as enhancement of patients’ social skills; education and support for the families; and educational programs for the community. All services are free of charge. The operational cost of the service is low because the MMHU I-T uses the resources and infrastructures of the primary healthcare system.
A total of 12 employees consist the workforce of the MMHU I-T. The multidisciplinary team consists of one psychiatrist, who is also the team's supervisor, two psychologists, two nurses, two health visitors, and two social workers. Members of the personnel are also an administrative officer and two professional drivers as the transportation of the team in those remote and mountainous areas is not always an easy task, especially in winter, and often requires special driving skills.
In rural areas in Greece, there is a well-developed primary healthcare system, constituted by local health centers and regional medical offices.[10] The MMHU I-T visits the eight primary health care centers of the catchment area weekly and has the potential for domiciliary visits. Patients are followed up weekly, fortnightly, or monthly, by the MMHU I-T according to the case management role.
Patients’ recording
After 10 years of establishment, a large number of patients have been examined and treated by the MMHU I-T. All patients’ medical charts have been recorded to our electronic database, which is regularly updated. Demographic data and information regarding diagnoses and referrals that are presented here were retrieved from the database.
RESULTS
The integration of the Mobile Mental Health Unit of the Prefectures of Ioannina and Thesprotia into the primary healthcare system
The first priority was the establishment of cooperation with primary care professionals. Primary care professionals were expected initially to be the main source of patient referrals to the MMHU I-T. In most cases, the integration of our unit within the local healthcare network was successful and complete. The MMHU I-T is now an integral part of the local primary care system and well known to the population of the catchment area. After 10 years, this is reflected to the current patient referral status. By the end of 2016, the majority of patients (60%) were self-referred or family-referred, whereas still a large proportion of patients (29%) were referrals from primary care physicians. Those rates in the first 2 years were 24% and 41.3%, respectively.[11] The rest patients were referred from local social services or general hospitals. Over the decade, there was a significant trend toward more self- or family-referrals and less referrals from other sources (Pearson Chi-square 144.682; df 2; P = 0.000).
The contribution of the Mobile Mental Health Unit of the Prefectures of Ioannina and Thesprotia to the mental health of the catchment area
It is worth noting that within the first 2 years of operation of the MMHU I-T hospitalizations of treatment engaged patients were reduced significantly by 30.4%.[11] A subsequent 5-year study showed that treatment engagement rates of patients with psychotic disorders were as high as 67.2%. None of the examined patient-related factors were associated with treatment engagement, and these rates were better explained as service-related. It seems that patients with psychotic disorders may engage to treatment due to the easiness of access and the nonrestrictive care setting.[12] More recently, we reported on the regular benzodiazepine prescription in patients with a psychotic disorder who regularly attended follow-up appointments with the MMHU I-T. Rates were rather high (39%) although within the range previously reported in the literature, and such prescription was found to be correlated to previous history of alcohol/substance abuse. We discussed the potential implications of these results for mental health services and for primary care settings in rural areas.[13]
Due to the increased proportion of elderly patients attending our service, we were able to study this population and we have shown that the provision of care based on regular visits at patients’ homes was correlated with the age of the patients: the older the patient, the more likely they were to receive home-based care.[14] Moreover, in the population of older adult patients, we found that patients with a diagnosis of dementia and patients with psychotic disorders were more likely to receive home-based care by the multidisciplinary team.[15]
During this decade among the large number of patients who have been examined and treated by the MMHU I-T, there were several rare and interesting cases.[16171819] The clinical work of the MMHU I-T allowed for the establishment of a publication record that is worthy to mention.
The present caseload status
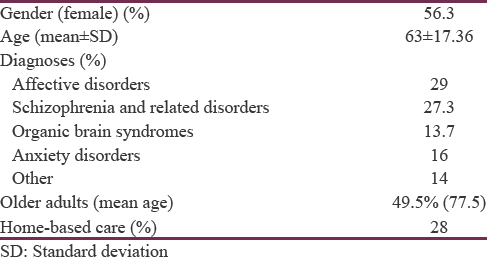
By the end of 2016, the total number of active patients (that is patients regularly attended scheduled follow-up appointments) was 293 (mean age 63 years). Almost half of them (49.5%) were older adults, with a mean age of 77.5 years and a total of 29.7% of the patients being ≥75 years old. Most common diagnoses are affective disorders and psychotic disorders [Table 1]. Moreover, 70 additional patients were rated as “partially engaged,” that is they do not attend follow-up appointments regularly, but they still visit our service sometimes. Each of the team members has a high caseload (mean 36.6 patients). A significant proportion of patients (n = 82, 28%) receive care with regular domiciliary visits.
DISCUSSION
In this paper, we report on the operation of a community mental health mobile service, the MMHU I-T, and present a 10-year account of delivering services in rural, remote, and deprived areas of Greece. The MMHU I-T has contributed to the reduction of patients’ hospitalizations and to the treatment engagement of patients with psychotic disorders. Moreover, it provides home-based services for the challenging population of older adults. All these indices may indirectly suggest that this service can reduce the burden of disease and the total costs associated with mental illness in the underserved population of rural areas. Yet, cost-effectiveness assessment is urgently needed to form definite conclusions regarding the relevance of this model of care for the health system.
Currently, the number of active patients is 293, which is much more than the proposed 200–250 cases, considered the maximum for most teams to exploit multidisciplinary working.[20] The mean caseload for each member of the multidisciplinary team is 36.6 (excluding the psychiatrist/supervisor, who is responsible for all patients), which exceeds the maximum of 30 recommended,[20] and this raises challenges for the maintenance of quality of the delivered care. It should be noted that patient discharge to primary care is not always feasible, due to the chronicity and complexity of the cases, to patients’ unwillingness, and to primary care physicians’ reluctance. A significant proportion of patients (28%) receive home-based care. This practice is resource- and time-consuming but is necessary for the elderly and for the severely mentally ill patients because it facilitates their access to care, and but for most, this is the only opportunity to receive mental health care at their place of residence.
Over this decade, the number of self- or family-referred patients raised dramatically, which may suggest that the integration of the MMHU I-T into the primary healthcare system was successful and the service is acceptable to patients and easily accessible. Other parameters associated with the integration of the MMHU I-T in the primary care system have not been studied. These include the impact on the perceived stigmatization of patients in those areas and the impact on primary care professionals’ training in mental health issues. Moreover, the impact on primary care professionals’ attitudes toward mental illness is an area for the future research.
There are several similar MMHUs in our country, operating in rural areas and in some of the numerous Greek islands, which follow uniform operational principles. Their contribution to the mental health care of the underserved population is significant, yet their work remains mostly unpublished in the international literature, with few exceptions.[621]
The impact of economic crisis
The effects of the Greece's economic crisis on the population's health and on health services are well documented.[2223] Mental health services have been affected by the recession, in terms of budget cuts, personnel's morale, and infrastructure issues,[24] while needs are increasing, due to the increased rates of psychiatric disorders in recent years.[25262728] That makes the provision of low-cost, easily accessible services by MMHUs even more relevant.
Perhaps, the economic adversities may partly explain the increased proportion of self- or family-referred patients to the MMHU I-T by the end of 2016, compared to the first 2 years. Many patients would previously prefer to be examined in the well-developed private psychiatric sector in our area,[29] but now, they turn to the free of charge services provided by the MMHU I-T. However, other factors should be considered. After 10 years of successful integration of the MMHU I-T in the primary care system, our service has become more acceptable to patients. Moreover, with the continuing education of the community, the impact of stigma toward mental illness may have become less profound and may not prevent patients from seeking help from a local mental health service.
The future
Major challenges for the MMHU I-T are ahead. First, half of the members of the multidisciplinary team have been working continuously for a decade. Rural working has been associated with several adversities for health professionals,[30] and this may impact on the personnel's morale and performance. Although still motivated, the members of the multidisciplinary team face many demands and perhaps regular renewal of the personnel is warranted to protect them from distress and exhaustion. On the other hand, despite the adversities in working remotely, the practice of mental health service delivery in those rural areas may be rewarding in several aspects. For instance, case complexity may be challenging and requires a high index of professionalism and keeping up to date with current scientific knowledge.
Another important issue in rural areas is the ongoing aging of the population. Elderly patients are almost half of active patients of the MMHU I-T and their percentage is expected to rise in the future. The care of those patients is challenging for the mental health system. There is inconclusive evidence that highly specialized teams for older adults provide effective services,[31] yet preventive interventions for this vulnerable population have not been adequately developed.[32] Our intention is to incorporate principles and skills of psychogeriatric care in regular clinical practice so as to deliver even more effective services to those patients. There are a necessity for further training of the multidisciplinary team in psychogeriatrics and a need for training in general medical conditions as those are commonly encountered in the elderly in routine clinical practice.
Another challenge that MMHU I-T faces is the increased rates of physical morbidity in patients with serious mental illness.[33] A previous study on patients who received community psychiatric services reported high rates of physical disorders, such as diabetes, lung disease, and liver problems.[34] Most importantly, evidence suggests that medical problems of patients with severe mental illness may go unrecognized at the level of primary care.[35] The integration of the MMHU I-T into the primary healthcare system facilitates patients’ referral and coordination of care.
Another issue to be concerned about is the impact of the economic crisis on the resources of the MMHU I-T. Previously, there were periods with delays in the pay of the personnel and subsequently some salary cuts. It is not yet clear whether future funding will be adequate for the operation of MMHUs in our country, given the ongoing effects of recession and austerity. However, it is alarming that even in high-income countries, with a strong background in community mental health services, such as England, there have been some recent substantial reductions in the resources for mental health treatment.[36]
Implications for care
This study may have potential implications for practice and policy. It suggests that despite the adversities of working remotely, a highly motivated workforce can deliver mental health services in the most underserved areas. Distance from mental health facilities has been adversely associated with the use of the services,[37] and this and other socioeconomic reasons are particularly relevant for rural areas.[4] The MMHUs approach may contribute significantly to overcome these barriers in mental health service delivery in those areas.
MMHUs in Greece deliver generic mental health services. This model of care currently receives little attention in most Western countries where research has been focused on highly resourced specialized teams.[38] However, there is a controversy over the specialization of mental health services. Although it is generally viewed as evolution and progress, there is evidence that the effectiveness of generic community mental health teams may be comparable to the more specialized and highly resourced assertive community treatment at much lower cost.[3940] Service cost and funding are important issues nowadays in Greece and worldwide. This report points out the utility of generic mental health provision as an alternative to more specialized care in cases of underresourced settings. Moreover, our report is in line with recent suggestions that low-cost community mental health interventions should be prioritized in Greece, to alleviate the effects of austerity to the mental health of the population.[41]
We believe that this type of care may be relevant for most rural and remote settings. It is suggested by experts that low-income countries can rely on primary health care and local mental health services, for the provision of mental health care.[42] Conceivably, in high-income countries, this model of care delivery would be even more feasible and effective, if adequately supported.
CONCLUSIONS
The MMHU I-T and other similar units in Greece are a successful paradigm of a low-cost service which promotes mental health in rural, remote, and deprived areas. This model of care may be informative for clinical practice and health policy, given the ongoing recession and health budget cuts. It suggests that rural mental healthcare may be effectively delivered by integrating generic community mental health mobile teams into the primary care system.
In the era of economic crisis and austerity, with increased rates of mental disorders and limited resources, there is obvious need for flexible, low-cost services, such as the MMHUs which can address the patients’ needs in remote and deprived areas. MMHUs in our country may reduce the total cost of mental illness by reducing hospitalizations and the total burden of disease, yet their cost-effectiveness has to be studied. The Greek state should ensure adequate funding of these services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Mobile health units: Mobilizing healthcare to reach unreachable. Int J Healthc Manag. 2016;9:58-66.
- [Google Scholar]
- Team structures in community mental health. In: Morgan C, Bhugra D, eds. Principles of Social Psychiatry (2nd ed). Oxford: Wiley-Blackwell; 2010. p. :387-96.
- [Google Scholar]
- Efficacy of community treatments for schizophrenia and other psychotic disorders: A literature review. Front Psychiatry. 2013;4:116.
- [Google Scholar]
- Thornicroft G, Semrau M, Alen A, Drake RE, Ito H, Mari J, eds. Community Mental Health: Putting Policy into Practice Globally. New York, USA: Willey-Blackwell; 2011.
- The mental health care delivery system in Greece: Regional variation and socioeconomic correlates. J Ment Health Policy Econ. 1999;2:169-76.
- [Google Scholar]
- Mobile Mental Health Units on the islands: The experience of cyclades. In: Stylianidis S, ed. Social and Community Psychiatry. Switzerland: Springer; 2016. p. :167-91.
- [Google Scholar]
- Community mental health teams in Greece: The paradigm of Mobile Mental Health Units. Arch Hell Med. 2014;31:71-6.
- [Google Scholar]
- Socioeconomic indicators for analyzing convergence: The case of Greece: 1960-2004. Soc Indic Res. 2009;93:315-30.
- [Google Scholar]
- Hellenic Statistical Authority. Available from: http://www.statistics.gr/
- The contribution of a Mobile Mental Health Unit to the promotion of primary mental health in Rural areas in Greece: A 2-year follow-up. Eur Psychiatry. 2011;26:425-7.
- [Google Scholar]
- Treatment engagement of psychotic patients with a Mobile Mental Health Unit in Rural areas in Greece: A five-year study. Schizophr Res Treatment. 2013;2013:613956.
- [Google Scholar]
- Long-term benzodiazepine treatment in patients with psychotic disorders attending a mental health service in Rural Greece. J Neurosci Rural Pract. 2016;7(Suppl 1):S26-30.
- [Google Scholar]
- Home-based mental health care for the elderly in a Rural area in Greece. Psychiatry Clin Neurosci. 2013;67:458-9.
- [Google Scholar]
- Mental healthcare for older adults in Rural Greece. Int Psychogeriatr. 2016;28:698-700.
- [Google Scholar]
- Duloxetine-induced hypomania: Case report and brief review of the literature on SNRIs-induced mood switching. J Psychopharmacol. 2009;23:592-6.
- [Google Scholar]
- Induced delusional disorder in rural areas: A case of folie a quatre. Eur Psychiatry. 2009;24(Suppl 1):S955.
- [Google Scholar]
- First episode of psychosis in a middle-aged patient with a 14-year history of conversion disorder. Case Rep Psychiatry 2014 2014:804930.
- [Google Scholar]
- Atypical antipsychotics for the treatment of musical hallucinations in an elderly patient without a psychiatric disorder. J Neurosci Rural Pract. 2016;7:606-8.
- [Google Scholar]
- Planning and providing mental health services for a community. In: Gelder M, Andreasen N, Lopez-Ibor JJ, Geddes J, eds. New Oxford Textbook of Psychiatry (2nd ed). New York: Oxford University Press; 2009. p. :1452-62.
- [Google Scholar]
- Utilization of technological resources within the framework of operation of a Mobile Mental Health Unit. Psychiatriki. 2016;27:287-95.
- [Google Scholar]
- Effects of the economic crisis on health and healthcare in Greece in the literature from 2009 to 2013: A systematic review. Health Policy. 2014;115:111-9.
- [Google Scholar]
- The “depression” of mental health care in general hospitals in Greece in the era of recession. J Psychosom Res. 2013;74:530-2.
- [Google Scholar]
- Suicidal ideation and reported suicide attempts in Greece during the economic crisis. World Psychiatry. 2013;12:53-9.
- [Google Scholar]
- Major depression in the era of economic crisis: A replication of a cross-sectional study across Greece. J Affect Disord. 2013;145:308-14.
- [Google Scholar]
- Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry. 2013;13:163.
- [Google Scholar]
- Enduring financial crisis in Greece: Prevalence and correlates of major depression and suicidality. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1015-24.
- [Google Scholar]
- Rates of first episode of psychosis in a defined catchment area in Greece. Clin Pract Epidemiol Ment Health. 2013;9:251-4.
- [Google Scholar]
- Rural mental health workforce difficulties: A management perspective. Rural Remote Health. 2010;10:1519.
- [Google Scholar]
- Variations in structures, processes and outcomes of community mental health teams for older people: A systematic review of the literature. Aging Ment Health. 2012;16:861-73.
- [Google Scholar]
- Excess mortality in persons with severe mental disorders: A multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16:30-40.
- [Google Scholar]
- Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. J Nerv Ment Dis. 2004;192:421-7.
- [Google Scholar]
- Health care for patients with serious mental illness: Family medicine's role. J Am Board Fam Med. 2009;22:187-95.
- [Google Scholar]
- Specialist mental health services in England in 2014: Overview of funding, access and levels of care. Int J Ment Health Syst. 2015;9:34.
- [Google Scholar]
- How are caseload and service utilisation of psychiatric services influenced by distance? A geographical approach to the study of community-based mental health services. Soc Psychiatry Psychiatr Epidemiol. 2011;46:881-91.
- [Google Scholar]
- Intensive case management for severe mental illness. Cochrane Database Syst Rev. 2017;1:CD007906.
- [Google Scholar]
- The rise and fall of assertive community treatment? Int Rev Psychiatry. 2010;22:130-7.
- [Google Scholar]
- Low cost community health interventions to address the mental health crisis arising from Greece's financial austerity measures. Univ Ott J Med. 2014;4:28-31.
- [Google Scholar]
- Thornicroft G, Tansella M, eds. Better Mental Health Care. New York, USA: Cambridge University Press; 2008.






