Translate this page into:
Medicine Revisited: Safeguard Yourself against “Oblivious to the Obvious”
Address for correspondence: Dr. Gopal Krishna Dash, Department of Neurosciences, Mazumdar Shaw Hospital, Narayana Hrudayalaya, Plot - 258/A Bommasandra Industrial Area, Hosur Road, Anekal Taluk, Bengaluru - 560 099, Karnataka, India. E-mail: dashdrgk@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We are writing to you to describe the case of a young male who presented with innocuous clinical features while subsequent investigations directed us to an unexpected diagnosis. A young male was diagnosed locally as abdominal tuberculosis and empirically started on antitubercular therapy. He was referred to us with acute onset right-sided abducens nerve palsy and right-sided lower motor neuron LMN type of facial nerve palsy. Magnetic resonance imaging (MRI) of the brain with contrast showed pachymeningeal thickening and enhancement [Figure 1]. Cerebrospinal fluid (CSF) analysis revealed elevated CSF proteins (123 mg/dL). Investigations for infective etiology, granulomatous disorder, and autoimmune disease yielded no results. We postulated idiopathic hypertrophic pachymeningitis (HPM) as a causative which could explain the neurological presentation. Subsequently, the patient developed anisocoria with delirium. General and neurological deterioration due to multiorgan dysfunction continued despite optimal antibiotics and supportive treatment. Repeat neuroimaging showed no fresh changes. Subtle clues such as persistent anemia and thrombocytopenia despite blood product transfusion, no response to steroids or antitubercular therapy, and steady clinical worsening prompted a diagnostic bone marrow study. It suggested acute leukemic changes for which prompt treatment was instituted. Our patient was a case of acute leukemia with HPM notoriously disguised as abdominal tuberculosis with systemic dissemination.
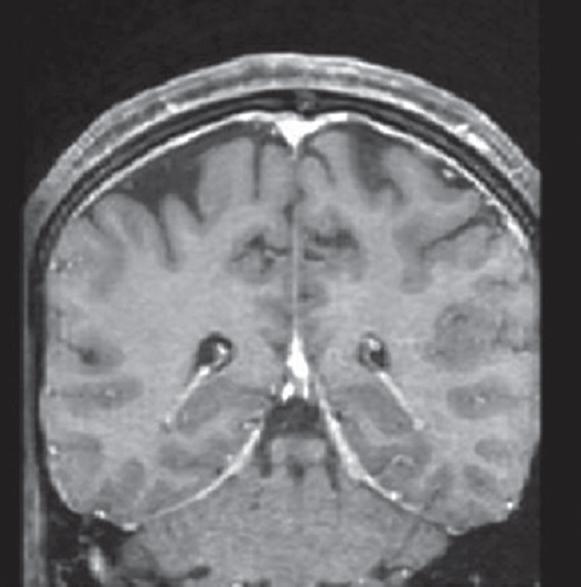
- Coronal section of contrast-enhanced magnetic resonance imaging of brain showing pachymeningeal enhancement. The enhancement iuniform without a hypointense streak between adjacent folds of falx cerebri, indicative of secondary hypertrophic cranial pachymeningitis
Leukemic involvement of the central nervous system is well known. Dural involvement has been reported in solid tumors, lymphoma, and leukemia.[1] Differentiation between the two forms of HPM-idiopathic and secondary is difficult. Contrast-enhanced MRI showing “Eiffel-by-night sign” is noted in up to 60% of idiopathic HPM patients and 12% with secondary HPM. Pathologically diffusely thickened fibrosed dura with inflammatory cell infiltration, more marked at the periphery, imparts a hyperintense signal on T1 sequences. This new sign if found points toward idiopathic HPM.[2] Clear indications for meningeal biopsy, which is the gold standard investigation, are lacking. We deferred meningeal biopsy due to progressive thrombocytopenia despite platelet cover. While steroids remain the mainstay of treatment for HPM, alternatives include azathioprine, cyclophosphamide, methotrexate, and cyclosporine, alone or in combination with steroids. Withdrawal of steroids may trigger the recurrence of neurodeficits, hence should be monitored closely. In cases similar to ours, specific treatment such as focal radiotherapy must be tried. Systemic chemotherapy is of limited value as it may not be able to reach the dural space.[1]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Detection of dural involvement by magnetic resonance imaging in adult patients with acute leukemias – Preliminary experience. Ann Hematol. 1995;70:243-9.
- [Google Scholar]
- Clinico-radiological spectrum and outcome in idiopathic hypertrophic pachymeningitis. J Neurol Sci. 2015;350:51-60.
- [Google Scholar]





