Translate this page into:
Magnetic resonance imaging findings of isolated abducent nerve palsy induced by vascular compression of vertebrobasilar dolichoectasia
Address for correspondence: Dr. Hidetaka Arishima, Department of Neurosurgery, University of Fukui, 23-3, Matsuokashimoaizuki, Eiheiji-cho, Yoshida-gun, Fukui, 910-1193, Japan. E-mail: ari@u-fukui.ac.jp
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
If the origin of isolated abducent nerve palsy cannot be found on neuroradiological examinations, diabetes mellitus is known as a probable cause; however, some cases show no potential causes of isolated abducent nerve palsy. Here, we report a 74-year-old male who suffered from diplopia due to isolated left abducent nerve palsy. Magnetic resonance angiography and fast imaging employing steady-state acquisition imaging clearly showed a dolichoectasic vertebrobasilar artery compressing the left abducent nerve upward and outward. There were no abnormal lesions in the brain stem, cavernous sinus, or orbital cavity. Laboratory data showed no abnormal findings. We concluded that neurovascular compression of the left abducent nerve might cause isolated left abducent nerve palsy. We observed him without surgical treatment considering his general condition with angina pectoris and old age. His symptom due to the left abducent nerve palsy persisted. From previous reports, conservative treatment could not improve abducent nerve palsy. Microvascular decompression should be considered for abducent nerve palsy due to vascular compression if patients are young, and their general condition is good. We also discuss interesting characteristics with a review of the literature.
Keywords
abducent nerve palsy
basilar artery
dolichoectasia
fast imaging employing steady-state acquisition
vertebral artery
Introduction
Isolated abducent nerve palsy is sometimes detected in patients with head trauma, intracranial hyper- and hypotension, and tumor of the brain stem, cavernous sinus, or orbital cavity.[12] Although these pathological conditions usually can be seen on computed tomography (CT) or magnetic resonance imaging findings (MRI), isolated abducent nerve palsy without radiological abnormality sometimes occurs. In such cases, diabetes mellitus or hypertension is a possible cause; however, some cases show no potential causes of isolated abducent nerve palsy.[12] Recently, patients with abducent nerve palsy due to neurovascular compression have been reported;[3456789101112131415] however, only a few report showed neurovascular compression clearly. Here, we report a patient with isolated abducent nerve palsy induced by neurovascular compression of vertebrobasilar dolichoectasia, which MRI with fast imaging employing steady-state acquisition (FIESTA) and magnetic resonance angiography (MRA) source images clearly showed. We also discuss the characteristics of these cases with a review of the literature.
Case Report
A 74-year-old male suffered from diplopia, and he saw an ophthalmologist who diagnosed left abducent nerve palsy without ocular pain. He took medicine for hypertension and hyperlipidemia. Two years earlier, he underwent percutaneous coronary intervention twice for angina pectoris and took antiplatelets. Neurological examination revealed no other findings of note. Laboratory tests showed no abnormal findings.
MRI with gadolinium enhancement showed no brain stem, cavernous sinus, or orbital lesions. MRA and three-dimensional volume rendering of MRI [Figure 1a] showed dolichoectasia of the right vertebral artery (VA) and basilar artery (BA). A hypoplastic left VA was not seen. Thin-slice MRI with FIESTA clearly showed that the right abducent nerve was straight; however, the left abducent nerve was compressed upward and outward by an elongated BA [Figure 1b]. The left abducent nerves were distinguished from bilateral anteroinferior cerebellar arteries (AICA) on comparing MRA source images [Figure 1c]. We concluded that neurovascular compression of vertebrobasilar dolichoectasia caused left isolated abducent nerve palsy.
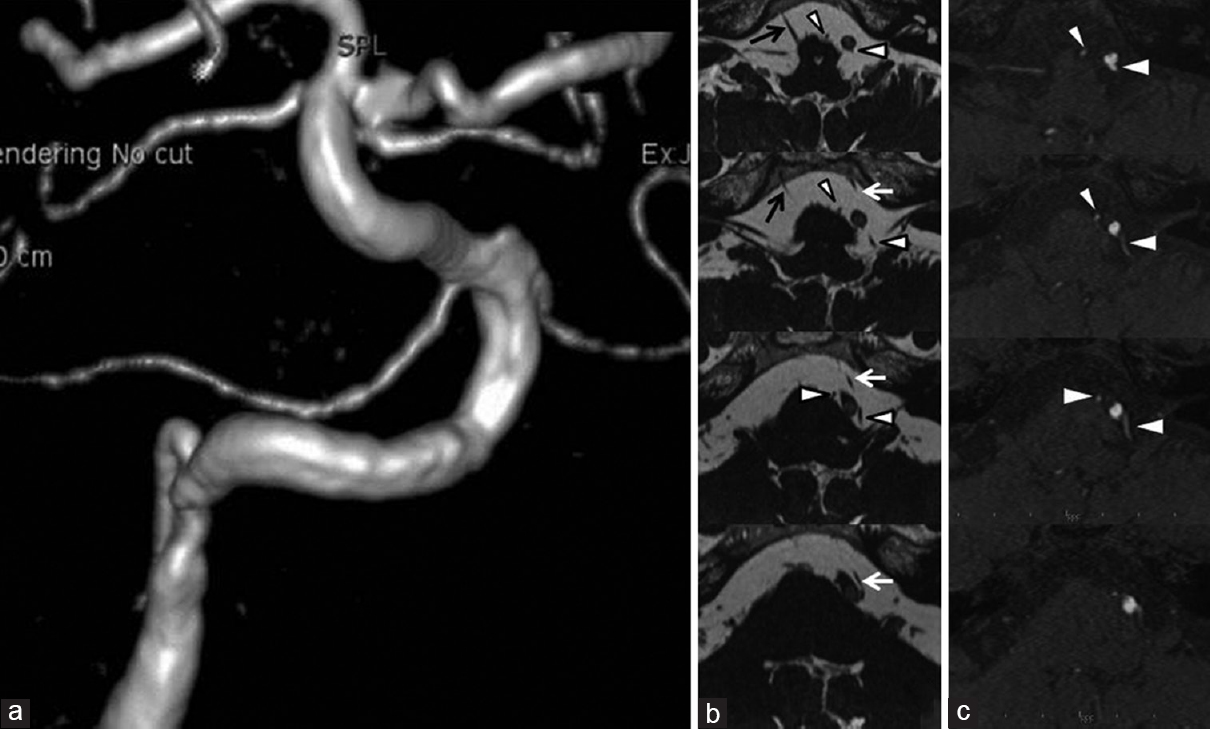
- Three-dimensional volume rendering of magnetic resonance imaging (a) showing dolichoectasia of the right vertebral artery and basilar artery. A hypoplastic left vertebral artery is not seen. Thin-slice magnetic resonance imaging with fast imaging employing steady-state acquisition (b), and magnetic resonance angiography source images (c). The right abducent nerve (black arrow) is straight; however, the left abducent nerve (white arrows) is compressed upward and outward by a basilar artery. Bilateral abducent nerves (black and white arrows) are distinguished from bilateral anteroinferior cerebellar arteries (arrowheads) shown in magnetic resonance angiography source images
Considering his age and heart disease, we observed him without surgical treatment. His symptom was temporarily improved imperfectly; however, diplopia became worse again, and the left abducent nerve palsy persisted.
Discussion
To the best of our knowledge, 15 cases with abducent nerve palsy due to nonaneurysmal vascular compression have been reported.[3456789101112131415] We summarize them in Table 1 in chronological order. Interestingly, all cases except for Case No. 4[8] were male, and most cases were not old, but middle-aged. Although the authors did not use the term “dolichoectasia” or “elongation” to describe Case No. 10,[6] they described “the vertebrobasilar arteries shifting leftward,” which means the “elongation” of vertebrobasilar arteries. Therefore, “dolichoectasia” or “elongation” of vertebrobasilar arteries induced vascular compression of the abducent nerves in all cases except for Case No. 9,[10] in which authors did not mention about “elongated” or “dolichoectasic” arteries. Usually, “dolichoectasia” means an atherosclerotic or a distinct arteriopathy characterized by elongation and dilation of the cerebral arteries; therefore, we speculate that “dolichoectasia” was used to be mostly the same as “elongation” in previous reports. Multivariate analyses by Pico et al. revealed an association between intracranial arterial dolichoectasia and the age (odds ratio: 1.04), male sex (3.31), hypertension (1.94), and previous myocardial infarction (2.68).[16] The odds ratio of age for intracranial arterial dolichoectasia was relatively lower. In addition, we speculate that those with an old age may not be accurately examined by MRI. These may offer reasons why abducent nerve palsy due to nonaneurysmal vascular compression was frequently reported in middle-aged males.
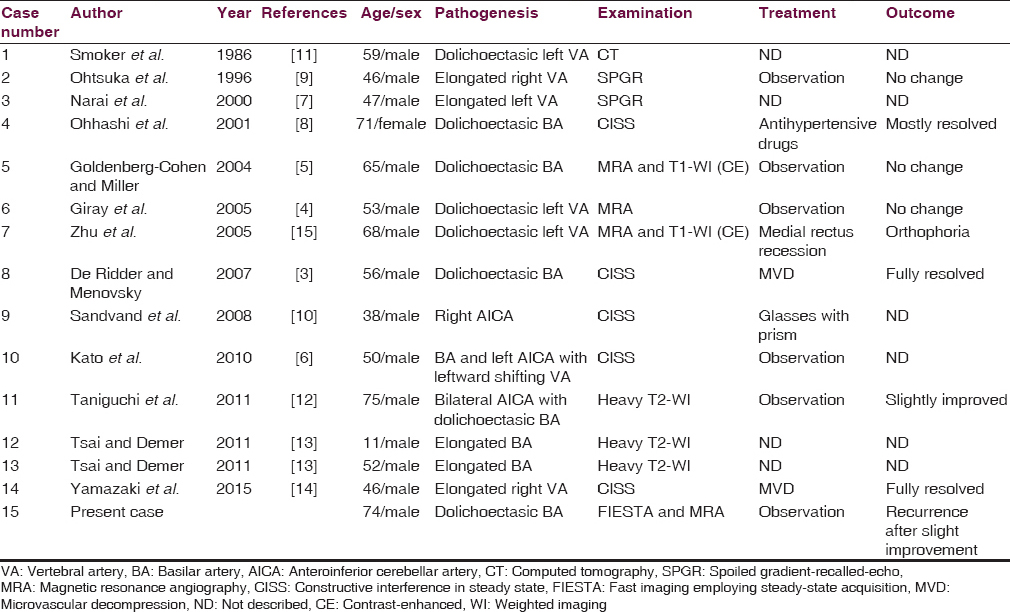
Radiological examination is important to understand this pathology. A compressed abducent nerve could not be clearly detected in the previous cases examined by CT or MRA.[451115] As recent reports showed, heavy T2-weighted imaging (WI), constructive interference in steady state (CISS), and FIESTA are essential to demonstrate vascular compression of the abducent nerve.[3678910121314] Additional MRA source images may be useful to distinguish the compressed abducent nerve from AICA, which was shown in our report.
Microvascular decompression (MVD) was performed for only two cases in which abducent nerve palsy was completely resolved, and Yamazaki et al. and De Ridder and Menovsky similarly mentioned MVD as a treatment option.[314] In their reports, the cisternal portion of the abducent nerve is more difficult to reach than the trigeminal or facial nerves, which are easily detected in MVD for trigeminal neuralgia and hemifacial spasm. King et al. reported that about 70% of cases with isolated abducent nerve palsy of an undetermined etiology resolved spontaneously within 4–6 months.[2] Therefore, Yamazaki et al. stated the importance of considering the surgical indication, for example, the age or daily activity of patients.[14] Four cases did not have descriptions of treatments or outcomes.[71113] Ophthalmological treatment was performed in two cases.[1015] Seven cases including our case and a medicated case were observed without surgical treatment,[4568912] in which two cases showed incomplete recovery.[812] Recurrent abducent nerve palsy associated with neurovascular compression was reported.[610] In our case, the left abducent nerve palsy persisted. The spontaneous recovery rate of the abducent nerve due to vascular compression seemed to be lower than that with an undetermined etiology.[2]
In the future, abducent nerve palsy due to vascular compression may be detected more frequently by MRI with CISS or FIESTA, and we can clarify the natural history of abducent nerve palsy with vascular compression and a “truly” undetermined etiology, which may lead to establishing an effective treatment for abducent nerve palsy due to vascular compression.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004;111:369-75.
- [Google Scholar]
- Spontaneous recovery rates for unilateral sixth nerve palsies. Eye (Lond). 1995;9(Pt 4):476-8.
- [Google Scholar]
- Neurovascular compression of the abducent nerve causing abducent palsy treated by microvascular decompression. Case report. J Neurosurg. 2007;107:1231-4.
- [Google Scholar]
- Isolated abducens nerve palsy caused by contralateral vertebral artery dolichoectasia. Neurol India. 2005;53:246-7.
- [Google Scholar]
- Noninvasive neuroimaging of basilar artery dolichoectasia in a patient with an isolated abducens nerve paresis. Am J Ophthalmol. 2004;137:365-7.
- [Google Scholar]
- Recurrent abducens nerve palsy associated with neurovascular compression. J Neurol Sci. 2010;295:135-6.
- [Google Scholar]
- Isolated abducens nerve palsy caused by vascular compression. Neurology. 2000;55:453-4.
- [Google Scholar]
- Isolated abducens nerve palsy caused by the compression of the basilar artery: A case report. No To Shinkei. 2001;53:69-72.
- [Google Scholar]
- Vascular compressive abducens nerve palsy disclosed by magnetic resonance imaging. Am J Ophthalmol. 1996;122:416-9.
- [Google Scholar]
- Periodic abducens nerve palsy in adults caused by neurovascular compression. J Neurol Neurosurg Psychiatry. 2008;79:100-2.
- [Google Scholar]
- High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: clinical-pathologic correlation and review. AJNR Am J Neuroradiol. 1986;7:61-72.
- [Google Scholar]
- Bilateral abducens nerve palsy by compression from bilateral anterior inferior cerebellar artery. J Neurol. 2011;258:2271-3.
- [Google Scholar]
- Nonaneurysmal cranial nerve compression as cause of neuropathic strabismus: evidence from high-resolution magnetic resonance imaging. Am J Ophthalmol. 2011;152:1067-73.
- [Google Scholar]
- Abducent nerve palsy treated by microvascular decompression: a case report and review of the literature. Acta Neurochir (Wien). 2015;157:1801-5.
- [Google Scholar]
- Sixth cranial nerve palsy caused by compression from a dolichoectatic vertebral artery. J Neuroophthalmol. 2005;25:134-5.
- [Google Scholar]
- GENIC Investigators. Intracranial arterial dolichoectasia and its relation with atherosclerosis and stroke subtype. Neurology. 2003;61:1736-42.
- [Google Scholar]






