Translate this page into:
Magnetic resonance imaging: Clinical experience with an open low-field-strength scanner in a resource challenged African state
Address for correspondence: Dr. Godwin Inalegwu Ogbole, Department of Radiology, University College Hospital, PMB 5116, Ibadan 200001, Nigeria. E-mail: gogbole@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Despite the fact that an magnetic resonance imaging (MRI) has been in clinical use for over 20 years, its use and availability in Nigeria, a West African state, is still extremely low. Hence, only few publications are available on the clinical experience with MRI from Nigeria. We set out to evaluate our initial clinical experience with a low-field-strength MRI in a Nigeria's foremost university hospital.
Materials and Methods:
A retrospective review of all studies, performed with an open 0.2 Tesla MAGNETOM Concerto (Siemens Medical) MRI scanner over a 5-year period (2006 - 2010) was conducted. All patients with complete records were evaluated for their clinical and demographic characteristics.
Results:
The records of 799 MRI studies were available. Patients’ ages ranged from 1 day to 90 years, with a mean of 40.1 years (± 20.7 SD). There were 463 (57.9%) males and 336 (42.1%) females. Over 90% of the studies were requested to evaluate brain or spine lesions. Low back pain represented the commonest (161/799, 20.7%) clinical indication for MRI. The largest number of patients was referred by physicians from surgical specialties (65.6%).
Conclusion:
The awareness and competence for proper use of MRI in Nigeria appears high. Low back pain is the commonest indication for MRI in our institution, and surgeons make a greater use of the facility. The provision of high-signal strength MRI may be beneficial in making a wider range of applications available to clinicians.
Keywords
Clinical experience
magnetic resonance imaging
Nigeria
Introduction
The use of magnetic resonance imaging (MRI) has been recognized as the most promising new technology in the clinical imaging arena since the advent of computed tomography in the early 1970s.[12] While this modality has been present for over 20 years, clinicians in developing African countries like Nigeria, have only recently had access to its potentials. All major organ systems, in absence of any ferro-magnetic implants, are acquiescent to MR imaging, and some are revealed with superior definition compared with their appearance in studies using the older alternative imaging technologies.[23] The comparative superior contrast resolution in MR images of the brain and spinal cord is of particular interest in clinical evaluation.[3]
Another benefit is its putative lack of biologic hazard to patients: An MRI is entirely non-invasive, and the radio-frequency photons are non-ionizing, therefore, there is no exposure to harmful ionizing radiation. The potential sources of hazard that have been identified, such as static magnetic fields, changing magnetic fields and radiofrequency heating, can be reasonably well-contained. No permanent side effects, even in pregnancy, have so far been recorded.[45]
At present, the number of MR imaging units in Nigeria is extremely low in proportion to the nation's number of teaching hospitals and its population of over 150 million.[6] There is, therefore, a dearth of publications on clinical experience with MRI in the country. Hence, the aim of this work is to evaluate and report on the initial clinical experience with MRI in our country's foremost university teaching hospital.
Materials and Methods
The records of all patients, referred to our hospital's department of radiology, for MRI investigations between January 2006 and December 2010 were reviewed. The demographic data, sources of referral, clinical indications and imaging findings were obtained. The MR equipment was a Siemens 0.2 T open low-field unit (Magnetom Concerto). Scanning sequences employed in imaging evaluation included T1-weighted, T2-weighted, T2-FLAIR (fluid attenuated inversion recovery), PD (proton density) and TOF (time of flight) sequences.
MR protocols were modified appropriately for individual scans of various parts of the body. Gadolinium-DTPA (Magnevist) was routinely used for contrast enhancement to provide useful additional information.
All patients had duly-filled consent forms and received counseling prior to examinations. An appropriate sedation was used for infants and children. Parents or guardians were permitted to stay with relatives during the imaging studies to ensure cooperation and to allay their fears.
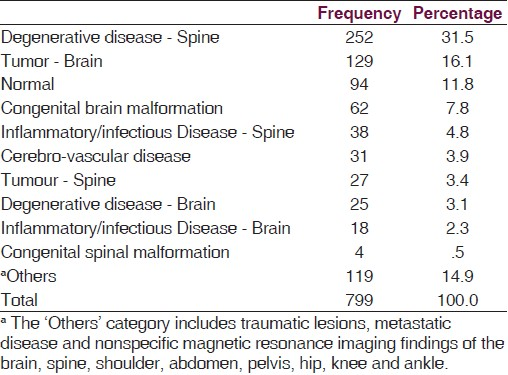
The indications for MRI or the main presenting complaints were categorized into 11 groups to accommodate the diverse and varied presenting symptoms [Table 1]. The MR imaging findings and diagnosis were classified, based on the ICD - 10 into the following categories: Normal, degenerative disease, infection / inflammation, tumors, cerebro-vascular disease, congenital anomalies and Others. The ‘others’ category includes traumatic lesions, metastatic disease and non-specific MRI findings of the brain, spine, shoulder, abdomen, pelvis, hip, knee and ankle [Table 2].

The clinical specialty of referring physicians were also recognized and grouped into 3 categories of ‘medical’, ‘surgical’ and ‘general / family practice’. The ‘surgical’ group includes physicians in neurosurgery, orthopedics and ophthalmology while the ‘medical’ group comprised physicians from specialties such as neurology, endocrinology and pediatrics among others.
The data was analyzed using the statistical programme for the social sciences (SPSS) version 17 (SPSS Inc, IL, USA). Descriptive statistics were presented in sizes and proportions (percentages, means ± standard deviation), and associations between some variables were explored with either the chi-square (or Fisher's exact) test, or the student t-test, as appropriate. The level of statistical significance was set at a P-value of ≤ 0.05.
Results
Of the 832 patients referred for MR studies, only the 799 (96.0%) who had complete records were used for the analysis during the period of study. Over the 5-year study period, nearly a 3rd (29.3%) of all the studies were performed in the 1st year of MRI usage at our center (2006) while only 32 (4%) studies were performed in 2008, representing the least number of cases. The average number of studies per year was 160.
The patients’ ages ranged from 1 day to 90 years with a mean of 40.1 years (SD ± 21.7). 133 (16.6%) patients were children below 16 years; Figure 1 shows the age distribution of the study population. Out of the 799 patients seen, males constituted 57.9% while females were 42.1% . Of all the referrals for MRI, 15.5% (124 / 799) were referred directly to the department from outside facilities while the remaining 84.5% (675 / 799) were patients, referred from various units by our hospital clinicians.
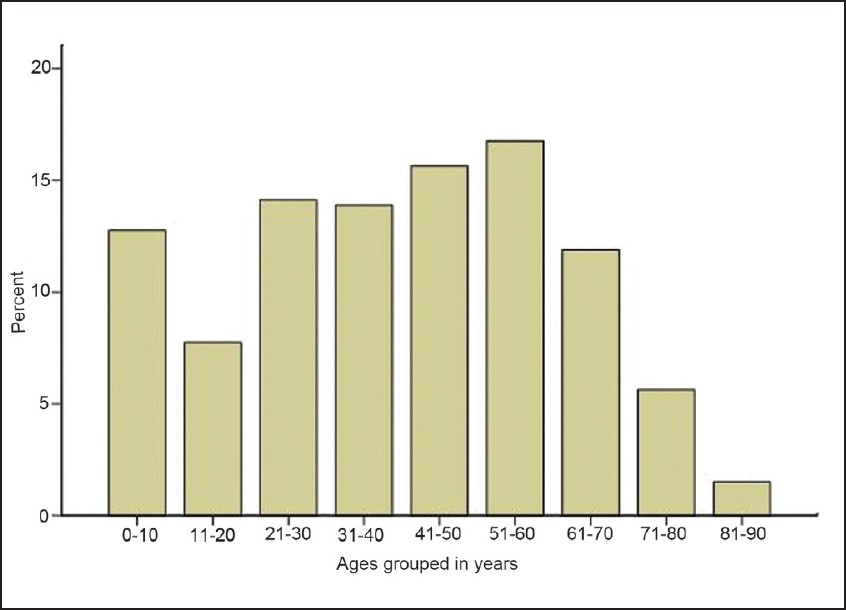
- Bar chart showing the age distribution of the study population
Table 1 shows the distribution of the main presenting complaints / indications for MRI evaluation. The commonest study indication was low back pain (20.5%), followed closely by paraplegia / paraparesis (15.1%) and headache (15.0%). The brain (49.9%) was the commonest single body region examined, followed by various parts of the spine (45.6%). Other regions of the body altogether represented only 4.5% of MR studies. Of the 799 patients evaluated, 136 (17.0%) had more than one body region examined. The spine represented 79.4% of the 2nd part of the body examined for patients. Only 2 adult patients had an examination of the whole spine. Intravenous contrast agent was administered in 455 (57%) patients. This amounts to an average of 91 patients per year. Of these, 74% (337 / 455) patients were required for cranial studies. The use of contrast was least required for cervical spine studies (31 / 455).
There were more referrals from surgical specialties (65.5%), especially from neurosurgery, compared to the medical (31.7%) and general / family practice (2.6%) specialties. There was no significant association between MRI indications with the specialty of the referring physician (P < 0.325).
General / family practice physicians (23.8%) were more likely to have referred patients with normal findings, compared to physicians in medical (19.4%) and surgical specialties (7.5%) (P < 0.001).
Among referrals from general / family practice physicians, there was a more likelihood of obtaining a finding of either degenerative disease of the spine (42.9%) or a normal study (23.8%). Also, the medical specialties tended to refer more patients, diagnosed with degenerative disease of the brain, (56.5%) compared with other specialties (P < 0.01).
The ICD-10 categorized MRI diagnosis showed degenerative diseases of the spine to represent the commonest finding with 31.5% [Figure 2]. 66 patients (8.3%) had congenital anomalies of the brain or spine. 93 patients (11.6%) were reported as normal. Understandably, an MRI based diagnosis showed adults to more likely present with a brain or spinal tumor [Figures 3–5] than children (P < 0.001) while children were more likely to be diagnosed with congenital anomalies of the brain or spine [Figure 6].

- T2-weighted image of the lumbosacral region showing multiple posterior disc herniation between L2 and L5 vertebral bodies with associated L4/L5 mild spondylolisthesis
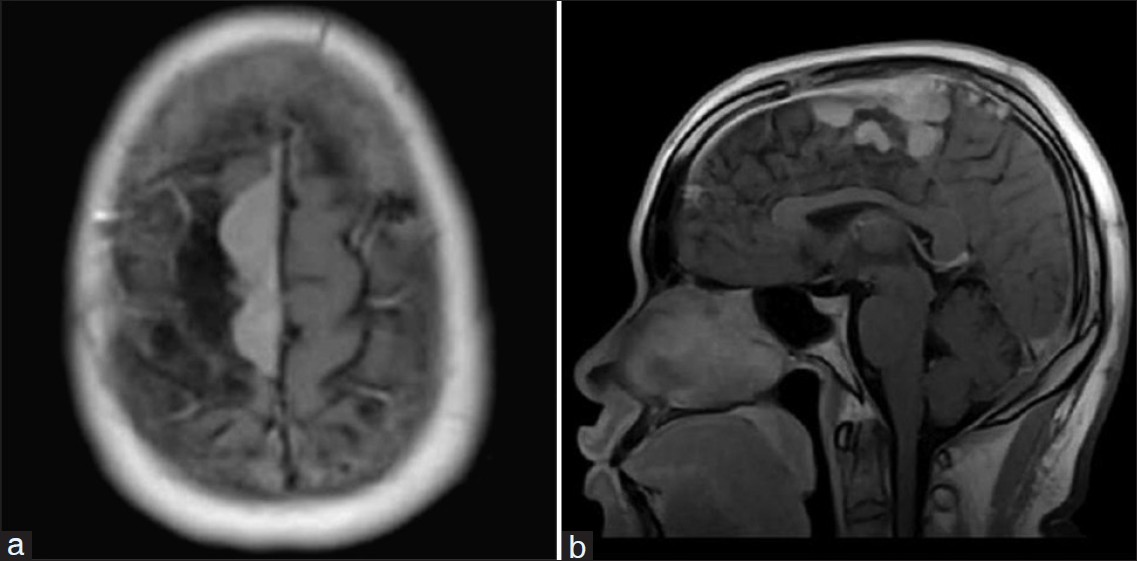
- T1-weighted post gadolinium axial (a) and sagittal (b) images showing a right parafalcine brilliantly enhancing meningioma in a 45-year-old male
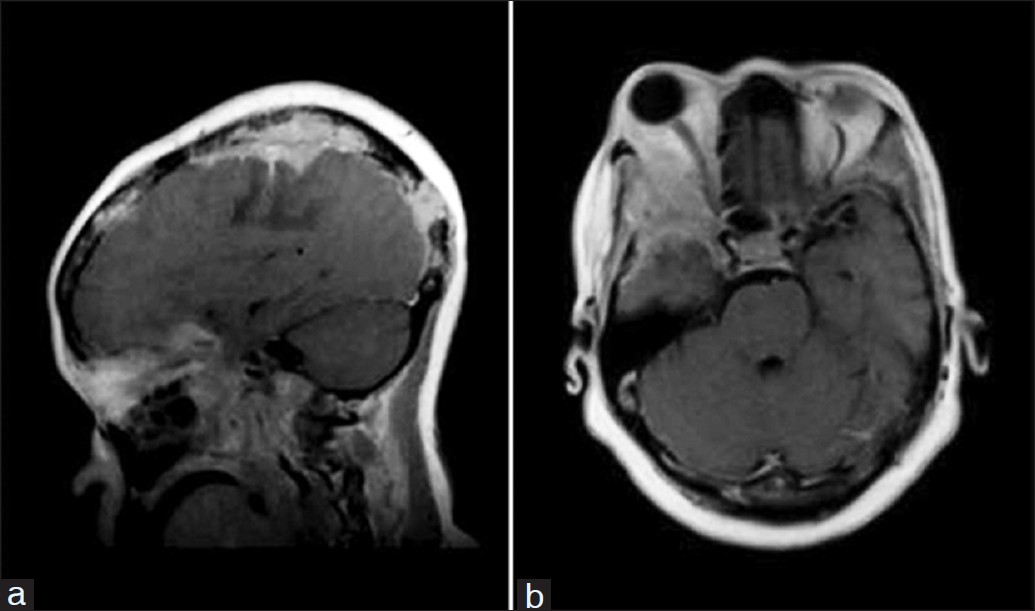
- Magnetic resonance images (a and b) showing multiple skull, leptomeningeal and orbital metastasis in a 43-year-old female with carcinoma of the breast
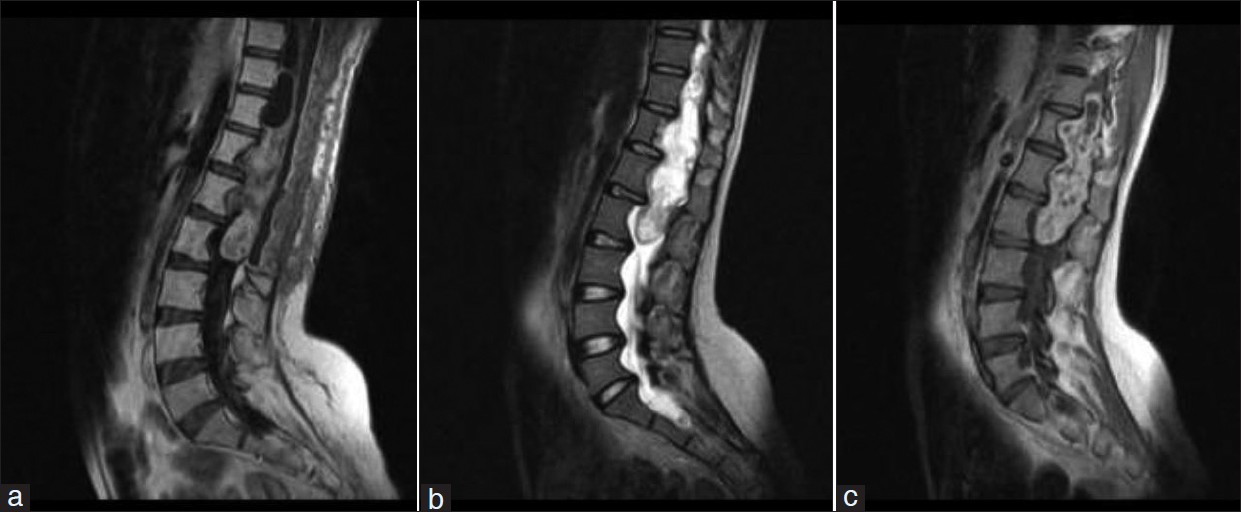
- Lumbosacral magnetic resonance images showing an extensive intra-spinal tumor in a 30-year-old female. The mass is isointense on T1-weighted images (a) but heterogeneous on T2-weighted images (b). It shows a heterogeneous enhancement with contrast (c). Note the posterior scalloping of the vertebral bodies
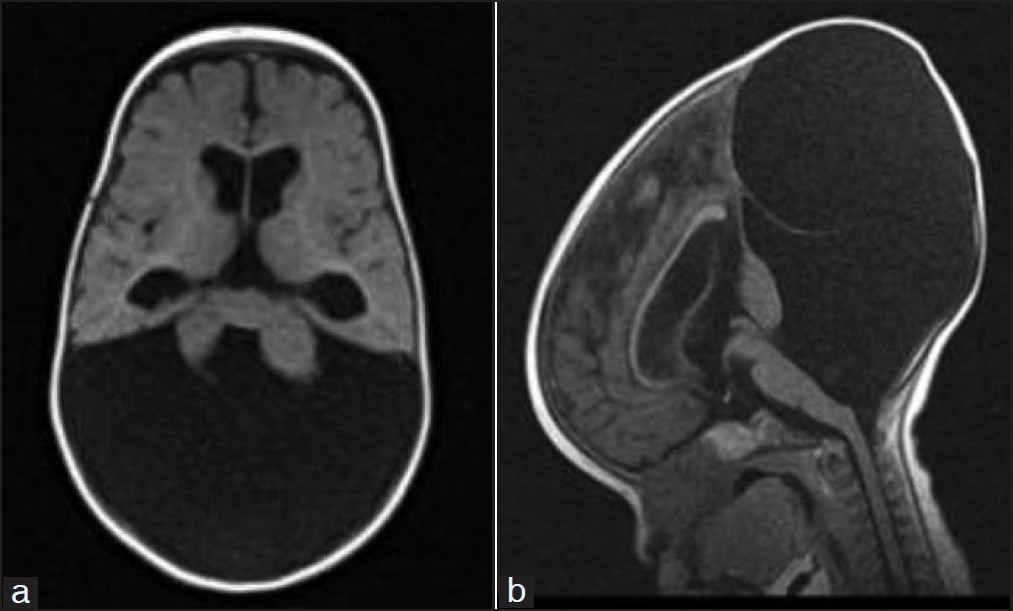
- Magnetic resonance images (a and b) showing cystic dilatation of the posterior fossa with hypoplasia of the cerebellar vermis and elevation of the torcular heterophils and tentorium in a 9-month- old male infant with Dandy-Walker syndrome
No pregnant patient was evaluated during the period of this study, and there was no record of an adverse contrast reaction. Sedation with a use of chloral hydrate, paraldehyde or diazepam was used for all children who were active and fully conscious during the scanning period, as indicated. The anesthetists were only called in to assist in only 3 cases. There were also no documented adverse events from anesthesia or sedation.
Discussion
Since the introduction of MRI for medical diagnostic use in the early 1970s, an extraordinary progress has been made in its clinical applications and in the evolvement of newer MRI techniques that more exquisitely reveal various organ systems’ anatomy and pathology.[1–3] In most parts of Africa and certainly in Nigeria, this technology has only recently become available. There is however no readily available official data to ascertain the number of functional MRI units in Nigeria. An estimate among Nigerian radiologists suggest less than 10 MRI units, representing less than 1/15 million people. This number is considered exceptionally small by international standards.[7] However, our center was arguably the first among the few university teaching hospitals to have installed a fully-functional unit, accessible to patients from all parts of the country where there had been none as at 2004. The 5-year- review period of this study provided a sufficient duration for assessing the benefits, state of usefulness and challenges of this relatively new imaging modality in Nigeria.
The yearly average number of scans we performed was notably small, compared to the world average of 41 / 1000 population and the 28,000 scans per year in the United States of America.[7] It is not likelythat other Nigerian hospitals with an MRI facility could have achieved a higher average, considering that our center is the largest referral hospital in the country. The long period of machine down-times and non-functionality affected the overall average number of studies performed as shown in the sharp decline in the number of studies performed in the year 2008. These occasional periods of non-functionality were essentially due to the lack of an adequate technical support and / or service materials.
The high cost of an MRI examination is also of concern regarding the volume of scans achieved, as over 70% of the over 150 million Nigerians live on < $1 per day.[5] Traditionally, the cost of an MRI has been known to be high, compared to competing technologies. An average cost of an MRI in our unit in Ibadan is about 500 US Dollars in local currency. Since our health care system is based on an out-of-pocket payment system, many patients that require an MRI are not able to afford it. However, for the fraction of the population who go to great lengths to have an MRI study, it may in the long run prove to be cost-effective as it usually obviates the need for either further imaging tests or for prolonged hospital stay.[8–11] Also, in-patient facility charges that invasive tests such as myelogram, cisternogram, or cerebral arteriogram would require, can be avoided.[8–11]
In Nigeria, there is unrestricted access to request for an MRI by general practitioners (GPs) unlike in the UK where strict guidelines exist.[12] Clinical authorities may need to develop similar local guidelines for our practice as our study shows that GPs are more likely to request studies that eventually were considered radiologically not significant and not likely to have led to changes in patient management.
In spite of this, it appears that physicians’ awareness of the clinical value of MRI in diagnostic evaluation in our center is high.
The accuracy in MRI interpretation requires technical and interpretation skills, which can vary with the level of training and type of equipment.[1213] Though users of our MRI unit received only a short period of training and employed low-field signal strength equipment, they were able to make diagnosis of a wide spectrum of abnormalities, ranging from cerebral white mater lesions to myelopathies and congenital anomalies.
We analyzed the archived patients’ records and radiologists’ reports, which provided details of the radiological findings. The individual images were not reviewed. An assessment of the images for their quality and possible value in directing or changing the course of patient management would have been beneficial in giving an insight into the efficacy of our low field system. We hope to make this the focus of a future study.
The availability of over 95% of patients’ information is commendable for a records unit where all patients’ record are still only stored in books or files. The missing records were mostly due to volunteers that were initially used for machine tests or for patients, subjected to MRI investigations for research purposes whose records were not readily accessible.
The largest number of studies was performed for brain and spinal abnormalities in this review, and though low-field MRI systems such as ours produce rather lower-resolution images than high-field systems, we have found it relatively suitable for the evaluation of gross and even some subtle lesions of the brain and spine in our hospital. The sensitivity of low-field MRI for brain and spinal lesions is known to be undoubtedly greater than CT.[14] Regarding the diagnosis of brain tumors, an MRI shows more anatomic details[1415] and is most suitable for cerebellopontine angle and 8 cranial nerve tumors, and other posterior fossa lesions in general, in contrast to CT.
The use of a low field strength system definitely had a bearing in the distribution of studies, performed in the study period. The reason for the comparatively few extremity studies is not clear; some have suggested the possible lack of confidence in the image quality of a low field system. Nevertheless, a number of studies have shown that low field systems are technically capable of detecting radiographic occult joint lesions.[1617]
The availability of an MRI has had an impact in improving the quality of imaging diagnosis and care in our center.[18] It is now the preferred modality for evaluating spinal diseases, ranging from radiculopathies to malignancy and to spinal cord injury. This has been particularly because an evaluation requires no intra-thecal injection and images of the entire spine rather than just a segment of the spinal cord is presented, thus making it a more comprehensive imaging modality.
Most of our findings in the spine were of degenerative disease which usually shows as loss of signal intensity of the inter-vertebral disc, indicating physiologic changes [Figure 1]. We found most of the degenerative changes in our series occurred in the lumbo-sacral region, which is consistent with findings in the literature.[1819]
Because of its non-utilization of ionizing radiation, MRI is particularly preferred in the imaging of children for whom an exposure to the ionizing radiation from other imaging modalities poses more serious potential hazards than in adults.[20] However, an age distribution in our study did not show any greater use of the facility for children, compared to adults. Nevertheless, it is noteworthy that neonates as young as 1 day old were evaluated.
Previously, worldwide and even in our setting, sonography has conventionally been used in evaluating children with congenital anomalies of the neuro-axis. However, MRI has provided an alternative imaging technique for resolving questionable sonographic abnormalities.[3] This is well-reflected in our study as a significant number of congenital cerebral and spinal abnormalities were detected during the study period, and it appears that these were cases that would have been technically difficult to fully evaluate using an ultrasound only.
The foremost problem of imaging children is being able to get their co-operation.[20] Sedation was used to achieve this in uncooperative children as well as in adults. Up to a 5th of children, undergoing sedation for diagnostic procedures may experience an adverse event.[2021] The data of the number of failed sedations resulting in failed procedures in children was not available for our review, but our empirical experience suggests that it is similar to what is recorded in literature.[2021]
Safety evaluations indicate that non-contrast MRI is safe for most patients, including pregnant women.[2223] Pacemakers, metallic cerebral aneurysm clips, intraocular metal and cochlear implants are definite contraindications to MRI. Other metallic, non-compatible implants require thorough individual patient evaluation.[24] The presence of these materials causes incomplete or technically inadequate studies and may harm the patient. In our practice, a thorough screening interview is usually performed by an MRI nurse to ensure safety and production of readable diagnostic images.
Paramagnetic contrast agents improve confidence in diagnosis in 45% to 75% of scans and actually change the apparent diagnosis in up to 30% of patients.[2526] Paramagnetic contrast agents cross the placenta and typically are contraindicated during pregnancy,[22] but all are otherwise safe.[27–29] Minor adverse reactions to the agents occurs in 2% to 3% of patients, and anaphylaxis occurs in about 1 in 100000 patients.[30]
Spinal MRI dominated the referrals we received during the study period.
The fact that low back pain was the commonest presenting symptom is probably responsible for this finding. It is interesting to note, however, that a meta-analysis of spinal studies showed an equivalent accuracy for spinal canal stenosis, a recognizable cause of low back pain, using plain spinal CT, myelographic CT and MRI.[3] Low back pain as the commonest symptom of presentation is likely due to the understanding that an MRI provides exquisite views of the soft tissues and nerves around the lumbar spine. Evidence of disc changes is also easily detectable with the use of the multi-planner functionality of MRI. Although our low-field-strength MRI system may not be comparable to high-field machines, it has been suitable for establishing significant radiologic diagnosis in patients with low back pain and guiding management of many other conditions in our center, particularly in the brain and the spine.
In conclusion, although a relatively new modality in Nigeria, awareness and competence for proper use of MRI in clinical practice appears to be high. Low back pain is the commonest indication for MRI in Ibadan, and surgeons show a greater use of the facility. The provision of local guidelines for its use and provision of high-field strength units may be beneficial in making a wider range of applications available to clinicians.
We sincerely appreciate all the MRI staff of the University College Hospital, Ibadan for their contributions in providing useful information and access to data used in preparing the manuscript for this work.
Source of Support: Nil
Conflict of Interest: The authors declare that they have no competing interests.
References
- Computerised transverse axial scanning (tomography) Description of system. Br J Radiol. 1973;46:1016-22.
- [Google Scholar]
- Magnetic resonance imaging.Part 11-Clinical applications [MedicalProgress] West J Med. 1984;141:638-48.
- [Google Scholar]
- The Clinical Efficacy of magnetic resonance imaging in Neuroimaging. Ann Intern Med. 1994;120:856-71.
- [Google Scholar]
- ACR Blue Ribbon Panel on MR Safety. ACR guidance document for safe MR practices: 2007. AJR Am J Roentgenol. 2007;188:1447-1474.
- [Google Scholar]
- MRI of the arthritic small joints: Comparison of extremity MRI (0.2 T) vs high-field MRI (1.5 T) Eur Radiol. 2011;11:1030-8.
- [Google Scholar]
- Dynamic gadolinium-enhanced magnetic resonance imaging of the wrists in patients with rheumatoid arthritis can discriminate active from inactive disease. Arthritis Rheum. 2003;48:1207-13.
- [Google Scholar]
- New radiographic bone erosions in the wrists of patients with rheumatoid arthritis are detectable with magnetic resonance imaging a median of two years earlier. Arthritis Rheum. 2003;48:2128-31.
- [Google Scholar]
- Number of .net. Available from: http://www.numberof.net/number ofMRI scans per year/
- [Google Scholar]
- A 5 year audit of myelographic findings in patients with spine related diseases referred to a private radiological outfit in south-eastern Nigeria. West African Journal of Radiology conference proceeding. 2005;12:97-99.
- [Google Scholar]
- Prospective study of lacunar infarction using magnetic resonance imaging. Stroke. 1990;21:546-54.
- [Google Scholar]
- Diagnosis of acute cerebral infarction: Comparison of CT and MR imaging. AJNR Am J Neuroradiol. 1991;12:611-20.
- [Google Scholar]
- Intracranial meningiomas.Comparison of plain and contrast-enhanced examinations in CT and MRI. Neuroradiology. 1990;32:12-8.
- [Google Scholar]
- Sensitivity of Gd-DTPA-enhanced MR imaging of benign extraaxial tumors. Radiology. 1988;166:829-33.
- [Google Scholar]
- Degenerative disease of the spine. In: CT and MR Imaging of the whole body (4th ed). St Louis: Mosby; 2003. p. :735.
- [Google Scholar]
- Sedation and general anaesthesia in children undergoing MRI and CT: Adverse events and outcomes. Br J Anaesth. 2000;84:743-8.
- [Google Scholar]
- Growth rates in pediatric diagnostic imaging and sedation. Anesth Analg. 2009;108:1616-21.
- [Google Scholar]
- Biological effects and safety aspects of magnetic resonance imaging. Magn Reson Q. 1989;5:243-61.
- [Google Scholar]
- MR procedures and biomedical implants, materials, and devices: 1993 update. Radiology. 1993;189:587-99.
- [Google Scholar]
- Clinical safety and efficacy of gadoteri-dol: A study in 411 patients with suspected intracranial and spinal disease. Radiology. 1991;181:701-9.
- [Google Scholar]
- Multicenter study of gadodiamide injection as a contrast agent in MR imaging of the brain and spine. Radiology. 1991;181:693-9.
- [Google Scholar]
- Efficacy of gadoteridol for magnetic resonance imaging of the brain and spine. Invest Radiol. 1992;27(Suppl l):S22-32.
- [Google Scholar]
- Gd-DTPA: Tolerance and safety after 4 years of clinical trials in more than 7000 patients. In: Proceedings of the Second European Congress of NMR in Medicine and Biology. 1988. p. :50.
- [Google Scholar]
- Safety assessment of gadopentetate dimeglumine in U.S. clinical trials. Radiology. 1990;174:17-23.
- [Google Scholar]
- Gadopentetate dimeglumine in craniospinal magnetic resonance imaging: Common uses and some potential pitfalls. Can Assoc Radiol J. 1992;43:100-10.
- [Google Scholar]
- Cerebrovascular magnetic resonance angiography: A critical verification. J Vase Surg. 1992;16:619-28.
- [Google Scholar]
- The diagnostic yield of magnetic resonance imaging (MRI) of the brain and spine requested by general practitioners: Comparison with hospital clinicians. Br J Gen Pract. 1999;49:559-61.
- [Google Scholar]






