Translate this page into:
Lumbosacral epidermoid with seedlings along the spinal cord central canal and intracranial extension
Address for correspondence: Dr. Suresh Kumar, Neuroradiology Cell, Department of Radiodiagnosis and Imaging, Indira Gandhi Medical College, Shimla - 171 001, Himachal Pradesh, India. E-mail: thakursuresh67@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Spinal epidermoid cyst is a slowly progressing benign tumor which account for less than 1% cases in adults and less than 3% in children. Rarely, the epidermoid may rupture, resulting in dissemination of its contents into subarachnoid space and ventricles.[1] We are reporting a case of a 23- year-old male adult presented with low backache since 2 years and urinary incontinence since 6 months. There was no history of any spinal trauma or lumbar puncture. On MRI possibility of an intraspinal epidermoid cyst was given [Figures 1a–d]. The patient underwent subtotal excision of the cyst and histopathology revealed it to be an epidermoid cyst. The patient again presented with low backache and urinary incontinence 6 months after the surgery. On MRI of lumbosacral spine, there was presence of a cystic lesion in the region of cauda equina which was about 11 × 3 cm extending from L5 to S1 level causing scalloping on the posterior aspect of the vertebral bodies. The lesion was heterogeneously hyperintense on T2-weighted images [Figure 2a], iso to hypointense on T1-weighted images [Figure 2b] and hyperintense on STIR [Figure 2c]. It showed restricted diffusion [Figures 2d and e] and on post contrast study there was peripheral enhancement [Figure 2f]. A diagnosis of recurrent intraspinal epidermoid was given. After 15 days, the patient presented with pain, weakness and numbness in left upper limb and left half of body. MRI of the whole spine was done. The central canal of the spinal cord was dilated throughout the length of spinal cord suggestive of syrinx formation. There were fat particles in the central canal of the cervical spinal cord [Figure 3], ambient cistern, quadrigeminal plate cistern, superior cerebellar cistern, lateral ventricle, third ventricle, fourth ventricle, along the sulci of cerebral hemispheres and cerebellar folia [Figure 4a–f]. There was no meningeal enhancement on post contrast images. A diagnosis of ruptured lumbosacral epidermoid with seedlings in the CSF subarachnoid space, ventricles and along central canal of spinal cord was given. The patient is being managed conservatively and is on corticosteroids for symptomatic relief.
![Pre-operative MR images of the lumbosacral spine show the presence of an intraspinal cystic lesion causing scalloping of the posterior aspects of bodies of L4, L5 and S1 vertebrae. It is heterogeneously hyperintense on T2 [as shown with white arrows in figure 1a], hypointense on T1 [Figure 1b], hyperintense on STIR [Figure 1c] and shows heterogeneous post contrast enhancement [Figure 1d]. There is presence of fat component in the lesion which is hyperintense on T1 and suppressed on STIR (as shown with red arrows in Figure 1b and c)](/content/150/2015/6/2/img/JNRP-6-286-g001.png)
- Pre-operative MR images of the lumbosacral spine show the presence of an intraspinal cystic lesion causing scalloping of the posterior aspects of bodies of L4, L5 and S1 vertebrae. It is heterogeneously hyperintense on T2 [as shown with white arrows in figure 1a], hypointense on T1 [Figure 1b], hyperintense on STIR [Figure 1c] and shows heterogeneous post contrast enhancement [Figure 1d]. There is presence of fat component in the lesion which is hyperintense on T1 and suppressed on STIR (as shown with red arrows in Figure 1b and c)
![MRI of the lumbosacral region shows presence of an intraspinal cystic lesion causing scalloping on the posterior aspects of bodies of L5 and S1 vertebra. It is heterogeneously hyperintense on T2), hypointense on T1-weighted images and hyperintense on STIR (as shown with white arrows in Figures 2a, b and 2c, respectively). It shows restricted diffusion (white arrows in Figure 2d and e) and peripheral enhancement in post contrast images (white arrow in Figure 2f). The cauda equina nerve roots cannot be seen separately in this region and there is syrinx formation in the scanned spinal cord [Figure 2a]. There is presence of another cystic lesion in the paraspinal region which is not showing any restricted diffusion which is postoperative collection (as shown with yellow arrows in the figures)](/content/150/2015/6/2/img/JNRP-6-286-g002.png)
- MRI of the lumbosacral region shows presence of an intraspinal cystic lesion causing scalloping on the posterior aspects of bodies of L5 and S1 vertebra. It is heterogeneously hyperintense on T2), hypointense on T1-weighted images and hyperintense on STIR (as shown with white arrows in Figures 2a, b and 2c, respectively). It shows restricted diffusion (white arrows in Figure 2d and e) and peripheral enhancement in post contrast images (white arrow in Figure 2f). The cauda equina nerve roots cannot be seen separately in this region and there is syrinx formation in the scanned spinal cord [Figure 2a]. There is presence of another cystic lesion in the paraspinal region which is not showing any restricted diffusion which is postoperative collection (as shown with yellow arrows in the figures)
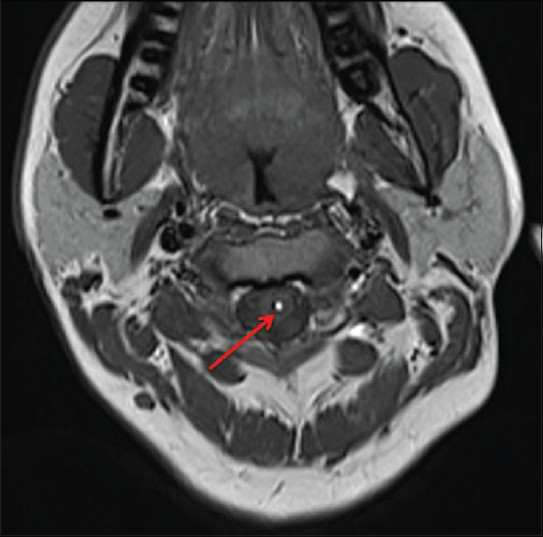
- Axial MRI T1-weighted image shows seedling along the central canal of spinal cord
![MRI of the cervical spine shows presence of altered signal intensity foci in the lateral ventricle, central canal of the spinal cord, fourth ventricle, cisterns and along the sulci, which are hyperintense on T1-weighted images (as shown with red arrows in Figure 4a–c), hyperintense on T2 [Figure 4d], suppressed on STIR [Figure 4e] and no post contrast enhancement [Figure 4f]. There is also formation of syrinx [Figure 4d and e]](/content/150/2015/6/2/img/JNRP-6-286-g004.png)
- MRI of the cervical spine shows presence of altered signal intensity foci in the lateral ventricle, central canal of the spinal cord, fourth ventricle, cisterns and along the sulci, which are hyperintense on T1-weighted images (as shown with red arrows in Figure 4a–c), hyperintense on T2 [Figure 4d], suppressed on STIR [Figure 4e] and no post contrast enhancement [Figure 4f]. There is also formation of syrinx [Figure 4d and e]
The rupture of epidermoid may occur spontaneously, during surgery or due to increased spinal and abdominal pressure. Spontaneous rupture of the epidermoid resulted in fat droplets in the CSF subarachnoid spaces, ventricles and along central canal of cervical spinal cord causing myelopathy changes.[2] Intraventricular fat particles may result in obstructive hydrocephalus. The inflammatory effect of fat on the vessels may result in vasospasm and ischemia. Symptoms due to cyst rupture may be due to encephalomeningitis or neurological symptoms due to inflammatory response. The patient may present with acute paraplegia, gradual paralysis or spinal cord injury. In severe cases the rupture of cyst may be fatal or rarely it may be asymptomatic.[13]
Diffuse subarachnoid or ventricular fat component may show resorption over a period of months. For symptomatic relief, palliative therapy such as corticosteroids or in recalcitrant cases surgical intervention such as CSF diversion is required. In the absence of symptomatic chemical meningitis, ruptured epidermoid cysts are treated with surgical removal with extensive rinsing of the subarachnoid space.[1]
References
- Ruptured epidermoid cyst of lateral ventricle. Available from: http://www.Panarabjn.org
- [Google Scholar]
- Magnetic resonance imaging of ruptured spinal dermoid tumors with spread of fatty droplets in the central spinal canal and/or spinal subarachnoidal space. J Neuroimaging. 2013;23:71-4.
- [Google Scholar]
- Paraplegia due to spinal epidermoid cyst rupture at asthma attack. Ann Rehabil Med. 2013;37:274-9.
- [Google Scholar]





