Translate this page into:
Long-term Benzodiazepine Treatment in Patients with Psychotic Disorders Attending a Mental Health Service in Rural Greece
Address for correspondence: Dr. Vaios Peritogiannis, 1 Moulaimidou Street, Ioannina 45444, Greece. E-mail: vaios.peritogiannis@medai.gr
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Long-term benzodiazepine (BZD) treatment in patients with mental disorders is widespread in clinical practice, and this is also the case of patients with schizophrenia, although the evidence is weak and BZD prescription is discouraged by guidelines and medical authorities. Data on BZD prescription are usually derived from national or regional databases whereas information on the use of BZD by patients with schizophrenia and related psychoses in general population-based samples is limited.
Materials and Methods:
Information for 77 patients with psychotic disorders who were regularly attending follow-up appointments with the multidisciplinary Mobile Mental Health Unit of the prefectures of Ioannina and Thesprotia, Northwest Greece, during 1-year period (2015) was obtained from our database.
Results:
From the total of 77 engaged patients, 30 (39%) were regularly prescribed BZDs in the long term, as part of their treatment regimen. Prescribed BZDs were mostly diazepam and lorazepam, in 43.3% of cases each. The mean daily dose of these compounds was 13 mg and 3.77 mg, respectively. Statistical analysis showed a correlation of long-term BZD use with the history of alcohol/substance abuse. Most patients were receiving BZD continuously for several years, and the mean dose was steady within this interval.
Conclusions:
A large proportion of patients with psychotic disorders were regularly prescribed BZD in long term. It appears that when BZDs are prescribed for some period in the course of a psychotic disorder, their use commonly exceeds the recommended interval and then becomes a regular part of the chronic treatment regimen. Future research should address the factors that may be related to the long-term BZD use by patients with psychotic disorders. Interventions for the reduction of regular BZD prescription should target the primary care setting and all those who treat first episode patients.
Keywords
Benzodiazepines
community mental health services
rural areas
schizophrenia
substance abuse
INTRODUCTION
Long-term benzodiazepine (BZD) treatment in patients with mental disorders is widespread in clinical practice although it is not recommended by international clinical guidelines and medical authorities.[1] In a recent systematic review of 41 register-based studies on definitions and prevalence of long-term BZD use, Kurko et al.[2] found a mean prevalence of 24% (ranged from 6% to 76%). Another recent study which comprised data from 7 European electronic health-care databases found the prevalence of BZD prescription to increase steadily with age and to be 2-fold higher in women than in men in all databases. A median of 18% of patients received 10 or more prescriptions in a year.[3]
In patients with schizophrenia and related disorders, BZDs such as diazepam and lorazepam are frequently co-prescribed to standard antipsychotic drug treatment in clinical practice.[4567] It has been suggested that as high as 95% of patients with schizophrenia receive a short-term BZD regimen at some point during their illness.[8] These compounds are used for managing hostile and aggressive behavior in patients with psychotic disorders. Other indications include anxiety, insomnia, and akathisia. However, recent guidelines do not recommend long-term BZD use in patients with schizophrenia. There are concerns that such use may increase the risk of dependence and may further deteriorate cognitive function.[9] Moreover, recent evidence suggests that BZD use by patients with schizophrenia is associated with increased mortality risk.[10]
Many large-scale studies on BZD prescription used data derived from national or regional databases whereas information on the use of BZD by patients with schizophrenia and related psychoses in general population-based samples is limited. A recent study from Finland reported a rate of BZD use by a sample of 55 patients with schizophrenia as high as 42% whereas 24% of patients were receiving BZD regularly.[11] The aim of the present study was to explore the long-term BZD use by community-dwelling patients with psychotic disorders, who regularly attend a mental health service within the primary care setting in rural and remote areas of Greece and to enquire for factors that may be associated with such use.
MATERIALS AND METHODS
The multidisciplinary Mobile Mental Health Unit of the prefectures of Ioannina and Thesprotia (MMHU I-T), Northwest Greece, has been established in 2007 and delivers services to a population grossly estimated at 100,000 inhabitants in rural and remote areas, mostly mountainous areas. Its contribution to the care of patients living in those areas has been reported elsewhere.[121314] The care of patients with psychotic disorders is a priority for the MMHU I-T. The MMHU I-T uses the resources of the primary care system but may also visit patients at their homes when needed.
Information for all patients with psychotic disorders who were regularly attending follow-up appointments with the MMHU I-T during 1-year period (2015) was obtained from our database, including demographic data (age and gender), clinical information (illness duration, number of admissions, and history of alcohol/substance abuse) and from prescription records. History of alcohol and substance abuse was determined according to the patients’ or family members’ accounts, or according to primary care records, without the use of a structured instrument. Patients’ psychopathology was not measured in detail as its association with BZD use could not be determined. Reason for the initial BZD prescription could not be accurately retrieved. Chronic BZD use was defined as regular use for at least 6 months within the year of the study. All the procedures were approved by the Institutional Board.
The sample comprised 77 stabilized, community-dwelling patients with schizophrenia and related disorders, according to the International Classification of Disease, 10th Revision that had been engaged to treatment with the MMHU I-T (i.e., they regularly attended scheduled follow-up appointments). Most patients (n=67, 87%) were receiving drug treatment before engagement with the MMHU I-T. Thus, prescribing patterns corresponded to the practice of several treatment settings and psychiatrists that had examined and treated those patients before they engage to treatment with the MMHU I-T. Most patients were chronic cases, and only 5 (6.5%) were first episode patients.
We reported our data separately for patients on BZD treatment and for those who did not receive BZD. Comparisons between the two patient groups were performed using Chi-square or Fisher's exact test for binary variables, and Student's t-test for continuous variables. P < 0.05 was considered statistically significant. The IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N.Y., USA) was used to perform all analyses.
RESULTS
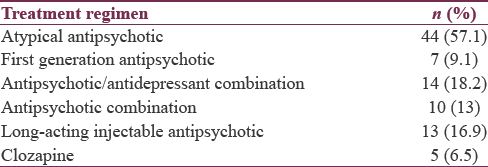
Most patients with psychotic disorders were male (66.2%) and middle-aged (mean age 54.2 years, median 54, standard deviation [SD] 14.94). The mean illness duration was 25.3 years (median 28 and SD 14.16). All but two patients were regularly refilling their antipsychotic prescriptions. The majority of the patients (n = 44, 57.1%) were receiving atypical antipsychotics whereas 18.2% of patients were receiving a concomitant antidepressant [Table 1]. A proportion of patients (n = 10, 13%) were receiving antipsychotic combination. Long-acting injectable antipsychotic was prescribed in 13 (16.9%) patients, and 5 (6.5%) patients were on clozapine treatment, but only 2 on clozapine monotherapy.
From the total of 77 engaged patients, 30 (39%) were regularly prescribed BZDs in long term, as part of their treatment regimen. Table 2 shows the correlations of chronic BZD use with several patients’ characteristics. Prescribed BZDs were mostly diazepam and lorazepam, in 13 cases each (43.3% of total patients in BZD treatment). The mean daily dose of these compounds was 13 mg and 3.77 mg, respectively. Statistical analysis showed a significant correlation of long-term BZD use with the history of alcohol/substance abuse (P = 0.013). Most patients were receiving BZD continuously for several years, and the mean dose was steady within this interval.

DISCUSSION
In this study, from the total of 77 engaged patients with psychotic disorders, 30 (39%) were regularly prescribed BZDs in long term. This rate lies within the range of the reported rates in literature which vary widely, from 16% to 79.2%, depending on definition, the treatment setting, and prescribing habits across countries.[4567] It appears that when BZDs are prescribed for some period in the course of a psychotic disorder, their use commonly exceeds the recommended interval and then becomes a regular part of the chronic treatment regimen. Given the sedative effects of BZDs and their effects on cognitive function, their long-term use is discouraged by medical authorities.[115] However, this may not be the case of everyday clinical practice.[4567]
An important finding of the present study is that the mean BZD dose was stable over time and rather moderate although somewhat higher than in the study by Wu et al.[6] This finding raises questions about the induction of tolerance in such patients, at these doses. It may be interpreted as that the therapeutic benefits of BZD treatment may be maintained over long periods of time in a proportion of patients.[9] Moreover, patients may find the sedative effects of BZD pleasant[16] and may resist to dose reduction, or discontinuation; or dependence may have occurred, which renders discontinuation too difficult.[17] These issues should be taken into account by clinicians when prescribing BZD, especially in patients with a history of substance abuse. In addition, it is possible that clinicians are reluctant to change the treatment regimen in chronic, stabilized patients with psychotic disorders to avoid the risk of decompensation.[6]
Statistical analysis showed that long-term BZD prescription was correlated with a history of alcohol/substance abuse. This finding implies that such patients are prone to regular use after initial prescription. The administration of BZD in long term, at steady doses, may have the desirable sedative and relaxant effects on those patients and importantly this use is medically monitored and not uncontrolled or illicit. This is in accordance with the recommendation of the British authorities that in patients with a history of drug dependence, a conscious decision to continue BZD treatment may be more reasonable than the alternatives.[9] Perhaps, in those cases, long-term BZD treatment in moderate and stable dose could be acceptable and may prevent patients from seeking substances or alcohol. However, cautious prescribing is always warranted as there is some evidence that BZD use by patients with co-occurring severe mental illness and a substance use disorder increases the likelihood of BZD abuse.[18]
In our study, neither patients’ age nor gender was associated with long-term BZD treatment. In a recent European study which comprised data from 7 electronic health-care databases, it found the prevalence of BZD prescription to increase steadily with age and to be 2-fold higher in women than in men in all databases.[3] These discrepancies are probably explained due to differences in the samples of patients. The study of Huerta et al.[3] included prescriptions in patients with a broad range of diagnoses whereas our sample included patients with psychotic disorders. This may mean that BZD prescription patterns in patients with psychotic disorders differ from other diagnoses’ patients.
There is a paucity of research on the use of psychiatric medications by patients with schizophrenia and related psychoses in general population-based samples.[11] This study addresses the important issue of regular BZD prescription in rural community-dwelling patients with psychotic disorders. It is well documented that mental health-care services remain inaccessible to rural communities for several reasons, including geographical barriers, economic constraints, and lack of resources, such as insufficient number of trained professionals.[1920] Mental health treatment delivery in rural and remote areas is challenging, and the results of this study are relevant for everyday clinical practice in those underserved areas.
Limitations
This study has several limitations: the evaluation of the history of alcohol/substance abuse was retrospective and was based on the patients’ records and their or other informants’ accounts. Moreover, in this sample of patients, the rates of abuse were rather low (15.6%) compared to the reported rates in literature.[21] It may be argued that in a sample of patients which would include more patients with a history of abuse, rates of regular BZD prescription would be even higher.
Current psychopathology was not measured in this study, but patients were rather rated as “stabilized”; they were community dwelling and regularly attended the follow-up appointments with the MMHU I-T. Symptomatology may not be relevant to the long-term BZD use, and it may fluctuate over time. It would be more informative to know about patients’ symptomatology at the time of initial prescription, but such information could not be retrieved. Another limitation was the lack of information regarding the reason of initial BZD prescription. Whatever the reason, the presumably short-term treatment perspective was not applied in these cases.
Strengths
This study has several strengths. While many large-scale studies on BZD prescription use data from national or regional databases, this study reports on a population-based sample of treatment engaged patients with psychotic disorders living in rural and remote areas where services are scarce and treatment delivery is difficult. Although it involves patients attending a single center, BZD prescription patterns do not correspond to the practice of a single center because most patients were receiving BZD for long before they engaged to treatment with the MMHU I-T. BZDs had been initially prescribed by several psychiatrists, working in various clinical settings at some point during the disease and their use was enduring afterward.
Studies on chronic BZD prescription usually use data derived from prescription records; however, in some cases, patients do refill their prescriptions but do not receive the prescribed drugs. In our study, patients who were engaged in long-term follow-up were most likely to receive their medication regularly.
Future research directions
Future research should address the factors that may be related to the long-term BZD use by patients with psychotic disorders. For instance, the role of personality has not been studied. Several personality traits, such as sensation or novelty seeking, have been associated with substance abuse by patients with schizophrenia,[2223] but their role in chronic BZD use is unknown. Another issue that requires further study is the implementation of strategies to reduce BZD use by patients with psychotic disorders. Recently, the results of a randomized controlled trial of two interventions to discontinue long-term BZD use by patients attending a primary care setting were reported. Both interventions led to significant reduction of BZD use, but the patient population comprised patients without severe psychiatric morbidity.[24]
Implications
In general, the results of this study are in accordance with the notions of medical authorities and suggest that the results of large, register-based reports may be applied to everyday community-dwelling patients with psychotic disorders in rural and remote areas. A potential implication of this study is a call for initiations to reduce BZD prescription to those patients.
Given the lack of mental health services in rural areas of Eastern European countries,[25] this study may have some implications for primary care settings. It brings into attention of primary care physicians working in rural and remote areas the phenomenon of long-term BZD treatment of those patients. In such areas, many patients with psychotic disorders may not have access to mental health services and their only contact with the healthcare system is through local primary care physicians who regularly refill patients’ prescriptions. Physicians should be aware of the correlation of BZD use with the history of abuse and prescribe those compounds cautiously. They should also regularly review patients’ need for continuous treatment, in cases of patients who do not attend a community mental health service; or they may seek expert advice for such cases by local mental health services, if available.
BZDs are initially prescribed in patients with psychotic disorders for the short-term management of several symptoms, but they are gradually become an integrated part of the treatment. Perhaps an opportunity for prevention of long-term BZD use is the treatment of patients with the first episode of psychosis (FEP). In a recent study, in our area, it was shown that most FEP patients are treated by private practice psychiatrists and selection of the treatment setting was predicted by a history of substance/alcohol abuse.[26] In the present report, such a history was found to be correlated with long-term BZD use in chronic patients. Taken together, these observations should raise awareness of private practice psychiatrists to spare BZD prescription in FEP patients with a history of abuse to avoid future regular prescription. Importantly, an earlier study from Singapore suggested that a proportion of FEP patients were already abusing BZD and highlighted the need for cautious prescription of these medications in this patient population.[27]
CONCLUSIONS
In our sample of community-dwelling patients with psychotic disorders attending a community mental health service in rural areas, a large proportion received BZD as part of their regular treatment regimen, and a history of alcohol/substance abuse was associated with regular BZD use. Although the generalizability of our findings may be limited by differences in prescribing habits among different settings and countries, they could inform clinical practice in rural settings, given the lack of studies in general population-based samples of patients. There is a need for research on mental health treatment in rural, remote, and frequently underserved areas, where mental health care may be inaccessible. Community mental health services in those areas may facilitate access to quality treatment, in collaboration with primary care providers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- British Medical Association. Royal Pharmaceutical Society of Great Britain. British National Formulary. London: BMJ Group and Pharmaceutical Press; 2012.
- Long-term use of benzodiazepines: Definitions, prevalence and usage patterns – A systematic review of register-based studies. Eur Psychiatry. 2015;30:1037-47.
- [Google Scholar]
- Exposure to benzodiazepines (anxiolytics, hypnotics and related drugs) in seven European electronic healthcare databases: A cross-national descriptive study from the PROTECT-EU Project. Pharmacoepidemiol Drug Saf. 2016;25(Suppl 1):56-65.
- [Google Scholar]
- Effects of polypharmacy on outcome in patients with schizophrenia in routine psychiatric treatment. Acta Psychiatr Scand. 2012;125:372-81.
- [Google Scholar]
- Benzodiazepine prescription practices and substance abuse in persons with severe mental illness. J Clin Psychiatry. 2004;65:151-5.
- [Google Scholar]
- Benzodiazepine use among patients with schizophrenia in Taiwan: A nationwide population-based survey. Psychiatr Serv. 2011;62:908-14.
- [Google Scholar]
- Prescription patterns for patients with schizophrenia in Korea: A focus on antipsychotic polypharmacy. Clin Psychopharmacol Neurosci. 2014;12:128-36.
- [Google Scholar]
- Concomitant medication of psychoses in a lifetime perspective. Hum Psychopharmacol. 2011;26:322-31.
- [Google Scholar]
- Benzodiazepines: Risks and benefits. A reconsideration. J Psychopharmacol. 2013;27:967-71.
- [Google Scholar]
- Benzodiazepine use and risk of mortality among patients with schizophrenia: A retrospective longitudinal study. J Clin Psychiatry. 2016;77:661-7.
- [Google Scholar]
- Use of psychiatric medications in schizophrenia and other psychoses in a general population sample. Psychiatry Res. 2016;235:160-8.
- [Google Scholar]
- The contribution of a mobile mental health unit to the promotion of primary mental health in rural areas in Greece: A 2-year follow-up. Eur Psychiatry. 2011;26:425-7.
- [Google Scholar]
- Treatment engagement of psychotic patients with a mobile mental health unit in rural areas in Greece: A five-year study. Schizophr Res Treatment 2013 2013:613956.
- [Google Scholar]
- Mental healthcare for older adults in rural Greece. Int Psychogeriatr. 2016;28:698-700.
- [Google Scholar]
- Re-examining the role of benzodiazepines in the treatment of schizophrenia: A systematic review. J Psychopharmacol. 2015;29:212-23.
- [Google Scholar]
- The misuse of benzodiazepines among adolescents: Psychosocial risk factors in a national sample. Drug Alcohol Depend. 2014;137:137-42.
- [Google Scholar]
- Do benzodiazepines still deserve a major role in the treatment of psychiatric disorders? A critical reappraisal. Eur Psychiatry. 2013;28:7-20.
- [Google Scholar]
- Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr Serv. 2003;54:1395-401.
- [Google Scholar]
- Access to rural mental health services: Service use and out-of-pocket costs. J Rural Health. 2010;26:214-24.
- [Google Scholar]
- Lost in the rush to national reform: Recommendations to improve impact on behavioral health providers in rural areas. J Health Care Poor Underserved. 2012;23:842-56.
- [Google Scholar]
- Drug and alcohol misuse in first episode psychosis: An observational study. Neuropsychiatr Dis Treat. 2008;4:417-23.
- [Google Scholar]
- Sensation-seeking, social anhedonia, and impulsivity in substance use disorder patients with and without schizophrenia and in non-abusing schizophrenia patients. Psychiatry Res. 2012;200:237-41.
- [Google Scholar]
- Sensation/novelty seeking in psychotic disorders: A review of the literature. World J Psychiatry. 2015;5:79-87.
- [Google Scholar]
- Comparative efficacy of two interventions to discontinue long-term benzodiazepine use: Cluster randomised controlled trial in primary care. Br J Psychiatry. 2014;204:471-9.
- [Google Scholar]
- Thornicroft G, Semrau M, Alen A, Drake RE, Ito H, Mari J, eds. Community Mental Health: Putting Policy into Practice Globally. New York, USA: Willey-Blackwell; 2011.
- Rates of first episode of psychosis in a defined catchment area in Greece. Clin Pract Epidemiol Ment Health. 2013;9:251-4.
- [Google Scholar]
- Substance abuse in schizophrenia. A Singapore perspective. Soc Psychiatry Psychiatr Epidemiol. 2002;37:326-8.
- [Google Scholar]






