Translate this page into:
Leptospirosis presenting as neuroretinitis
Address for correspondence: Dr. Ashok K. Kayal, Department of Neurology, Gauhati Medical College and Hospital, Indrapur, Guwahati – 781 032, Assam, India. E-mail: akkayal.gmcneuro@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We report a 25-years-old man, presented with sudden onset of reduced vision of the left eye for 1 week duration. Initially, it was a central field loss, which had then progressively involved the whole visual field. It was associated with floaters but was painless with no eye redness, itchiness or discharge. The left eye had normal function. There were no other constitutional symptoms like fever, body ache, jaundice etc. He denied any contact with animals. Past medical history was insignificant. However, he often indulged in swimming in the river during his current posting.
On examination, the best corrected visual acuity was 6/24 OD and 6/6 OS. The right eye had decreased color vision with presence of RAPD. Bulbar and palpebral conjunctival hyperemias were absent. Visual field testing revealed a centrocecal scotoma and cells were present in the vitreous of the right eye on slit lamp examination. Fundoscopic examination revealed a hyperemic optic disc with blurring of margin with macular edema and hard exudates in star shaped arrangement [Figure 1] without any evidence of vasculitis or retinal hemorrhage. Optical coherence tomography (OCT) revealed subretinal and intraretinal fluid in the macula. The left eye findings were normal. General physical and systemic examinations were normal. There were no features of systemic leptospirosis such as fever, conjunctival suffusion, jaundice and hepatosplenomegaly.
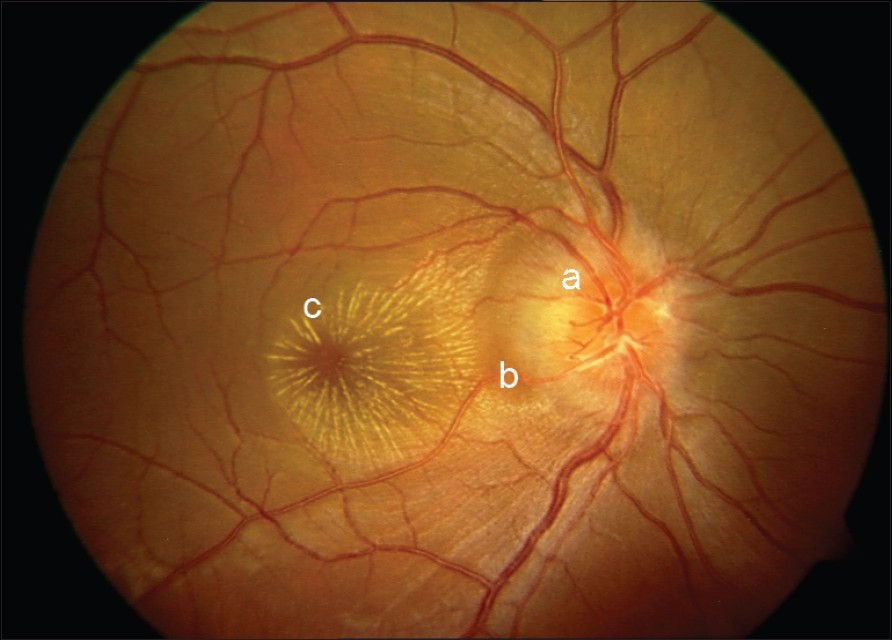
- Neuroretinitis showing (a) swelling of disc with (b) retinal edema and (c) macular star
The clinical findings of optic disc edema, coupled with subretinal fluid and a macular star, were consistent with a diagnosis of neuroretinitis. On investigation, there was mild leucocytosis with neutrophilia and ESR of 5 mm at the end of 1st hour. Blood biochemistry, urine examination was normal. A systemic workup revealed a positive leptospira IgG titer in serum 11.0 U/mL (positive > 9), leptospira IgM 25 U/mL (positive > 20). Other tests such as Mantoux test, ANA, VDRL, HIV, serologic tests for hepatitis B and C, toxoplasmosis, cysticercosis were negative. CT scan of head and thorax revealed no abnormalities. VEP demonstrated a prolonged latency in the right eye.
He was treated as a case of leptospirosis with neuroretinitis, with intravenous ampicilin 1 g IV 6 hourly and oral doxycycline 100 mg orally twice daily for 2 weeks, based on recommendation by CDC, Atlanta. Oral prednisolone was started at a dose of 1 mg/kg body weight for 2 weeks, with gradual taper over 2 weeks. Follow-up at 1 and 3 months showed an improvement of VA to 6/6 OD with normal color vision; however, the disc swelling and macular star persisted with mild vascular sheathing [Figure 2]. Last follow-up at 5 months revealed normal vision and optic disc with few retinal pigment epithelial changes [Figure 3] and normal OCT.
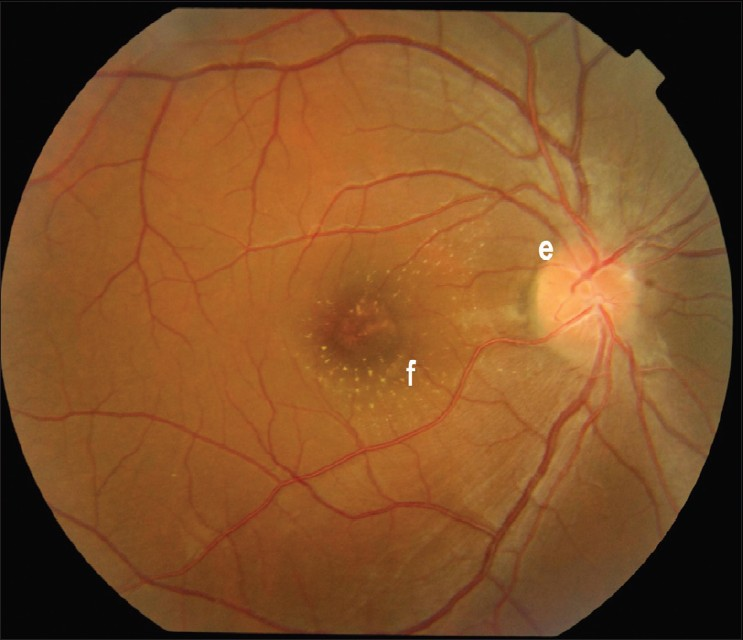
- Partial resolution of (e) disc edema with (f) few hard exudates in macular area
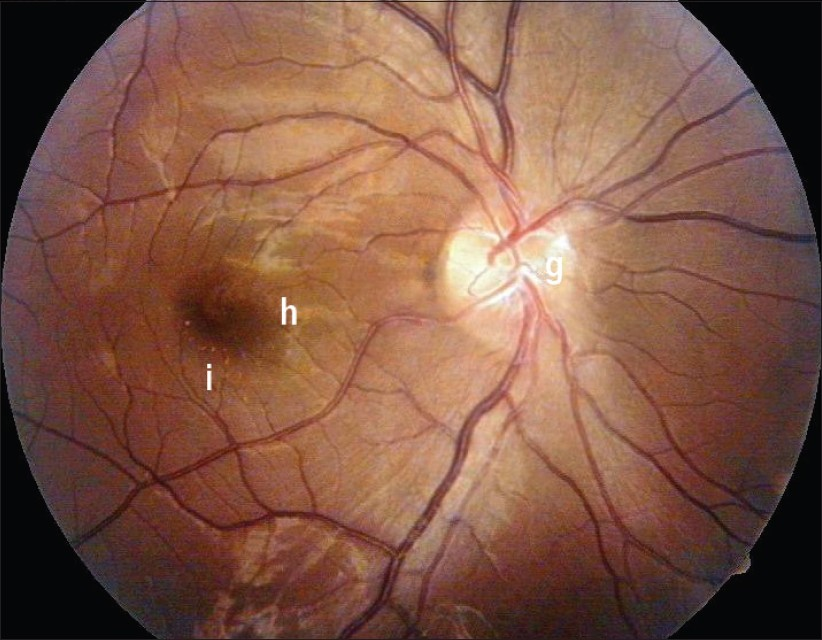
- Fundus revealing (g) mild sheathing of vessels over the disc and (h) complete resolution of retinal and macular edema with few (i) retinal pigment epithelial changes
Neuroretinitis is thought to be a result of an infectious or immune mediated process that may be precipitated by a number of bacterial, viral and parasitic agents.[1–3] The hallmark of neuroretinitis is optic disc edema with a macular star, which develops approximately 9 - 12 days after an onset and starts to disappear after 1 month, but can take 6 - 12 months for total resolution.[4]
Leptospirosis remains under-diagnosed despite its widespread prevalence due to various reasons.[4] Ocular findings in leptospirosis have been reported in 3 to 92%. Conjunctival hyperemia with engorged vessels is the most characteristic finding. Uveitis occurs in 10% of patients, from 2 weeks to 1 year after an initial infection with a good prognosis.[5]
Leptospirosis presenting as neuroretinitis without systemic manifestations has not been reported in Indian literature previously. Hence, the knowledge of this condition and institution of prompt treatment may result in full visual recovery. Treatment with anti-microbial agents (Amoxycillin, Doxycycline etc) is indicated in systemic leptospirosis. However, steroids are the mainstay of treatment for uveitis.[2]
Although neuroretinitis is the disease of varied etiology, and the extent of diagnostic workup should be determined by detailed history and examination.[4] It is a potentially treatable condition with a favorable outcome.
Acknowledgment
The authors thank Dr. Monalisa Bhoktiari, MD and Dr. Rahul Jain, MD for helping in preparation and writing of this manuscript.
References
- Neuroretinitis. In: Clinical neuroopthalmology (3rd ed). Baltimore Md: Williams and Wilkins Co; 1982. p. :234-5.
- [Google Scholar]
- Diseases of the optic nerve that may simulate macular disease. Trans Am Acad Ophthalmol Otolaryngol. 1977;83:766-9.
- [Google Scholar]





